Introduction
The treatment of head and neck cancer is based on 3 modalities, which can be combined or applied individually: radiotherapy, chemotherapy, and surgery. Radiotherapy, in which ionizing radiation is used to eliminate or control the neoplasm, has been adopted as a standard treatment in the early stages of head and neck cancer. Advanced cases, in contrast, commonly require chemotherapy and/or surgery.
12
The deleterious effects of radiation on bone tissue have been closely examined with the goal of elucidating the mechanisms leading to osteoradionecrosis,
3 but conclusive evidence is not yet available. Histomorphometric analysis of biopsies has proven to be a valuable laboratory method to evaluate bone quality, while clinical methods include digital radiography, ultrasonography, and computed tomography.
4
Panoramic radiographs, especially digital panoramic radiographs, are quick and easy to obtain, inexpensive, and comfortable for the patient, and they typically involve the administration of low doses of radiation. In addition, digital radiography has been considered a useful tool for the determination of systemic bone quality through the assessment of mandibular bone mass and morphology.
5 Despite conflicting results reported in the literature and limitations related to technical aspects and the reproducibility of the method, digital panoramic radiography has been described as capable of predicting osteopenia and osteoporosis after correlating those conditions with systemic bone mineral density values obtained through dual-energy X-ray absorptiometry.
6
A digital image is composed of an array of small areas known as pixels, to which specific numeric values are assigned.
5 Pixel intensity analysis of a digital panoramic radiograph can be based on a grayscale that ranges from 0 (black) to 255 (white),
7 in which pixel intensity is considered an indirect measurement of local bone mass
5. Fractal analysis is a mathematical model that describes and analyzes complex forms and structural patterns, numerically expressed as fractal dimensions.
5 Although several methods of fractal analysis have been described,
8 the box-counting technique has been the most widely applied and is suited for binary images
9 such as radiographs. This method can reveal complex interconnections of the trabecular bone, consequently indicating bone quality.
10
Thus, the aim of the present study was to evaluate the impact of radiotherapy on mandibular bone tissue in head and neck cancer patients through an analysis of pixel intensity and fractal dimension values on digital panoramic radiographs.
Go to :

Materials and Methods
Sample characteristics, eligibility criteria, and ethical issues
This retrospective study was conducted using digital panoramic radiographs from the electronic collection of the Stomatology and Oral and Maxillofacial Surgery Center at Heliópolis Hospital, obtained from patients between 2015 and 2018. To be considered eligible, individuals were required to be at least 18 years of age, to have a history of 3-dimensional (3D) conformational radiotherapy for head and neck cancer (involving the cervicofacial and supraclavicular fossa fields), and to have panoramic radiographic records available from before and after radiotherapy. As a local protocol, all initial radiographic images were taken during the oral interventions administered in the preparation for oncologic treatment, ranging from 1 to 3 weeks prior to radiotherapy.
The following exclusion criteria were applied: systemic diseases known to alter bone metabolism (e.g., osteoporosis, thyrotoxicosis, or hyperparathyroidism), use of any type of medication with known effects on bone metabolism (e.g., corticosteroids, antiangiogenic agents, or antiresorptive agents such as bisphosphonates or denosumab), poor positioning during the radiographic examination, poorquality images, and the presence of extensive mandibular pathologies (e.g., condensing osteitis, bone sclerosis, fibrous dysplasia, periapical lesions, or pathological fractures) in the areas of interest.
This study was approved by the Research Ethics Committee at Ibirapuera University (CAAE 91440318.3.0000.5597) and Heliópolis Hospital (CAEE 91440318.3.3001.5449) and was in compliance with the Declaration of Helsinki. Participants' privacy and confidentiality of information were ensured in all phases of the study.
Digital panoramic radiography
Digital panoramic radiographs were obtained using a PaX-400C device (Vatech, Hwaseong, Korea) with an exposure time of 14 s and an electric current of 8 mA. As suggested by the manufacturer, male and female subjects received peak kilovoltages of 68 kVp and 67 kVp, respectively. The images were stored digitally as 8-bit grayscale bitmap (.bmp) files with a resolution of 2900×1532 pixels.
Pixel intensity and fractal dimension analyses
The pixel intensity and fractal dimension analyses were adapted from the original studies by White and Rudolph
11 and Tosoni et al.
5 and were conducted using the image processing software ImageJ 1.52a (National Institutes of Health, Bethesda, MD, USA).
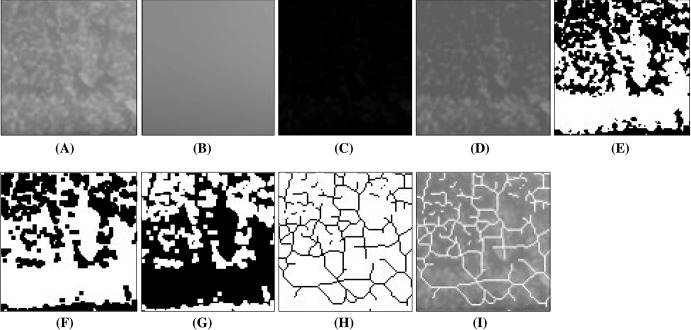
Initially, a fixed selection tool was used (100×100 pixels) to determine the region of interest (ROI) on each radiograph. This region was located unilaterally in the right angle region of the mandible (below the mandibular canal and posterior to the molar region), parallel to the posterior margin of the mandibular ramus, and included only trabecular bone (
Fig. 1).
 | Fig. 1Region of interest selection.
|
The mean pixel intensity value of each ROI was determined using the software histogram, and fractal dimension analysis was then performed. For this purpose, the image of the ROI was duplicated. This copy of the image was blurred using a Gaussian filter with a 35-pixel radius to retain only large density variations and was subtracted from the original image, generating a third image. A constant of 128 (corresponding to the half-value of the gray levels on the 8-bit scale) was added at each pixel position on the third image to ensure that variations in brightness corresponding to specific features (trabeculae and medullary spaces) were visible. The image was then converted into a binary image at a brightness threshold value of 128 to facilitate image segmentation into components that visually resembled trabeculae and medullary spaces. The image was then subjected to erosion and dilation to reduce noise and was inverted to reveal the trabeculae. Next, the image was skeletonized, or eroded until only the center pixel line remained, and superimposed over the original image to certify that the structures corresponded to the trabeculae. Finally, the box-counting method was applied with box sizes of 2, 3, 4, 6, 8, 12, 16, 32, and 64 pixels to determine the fractal dimension (
Fig. 2).
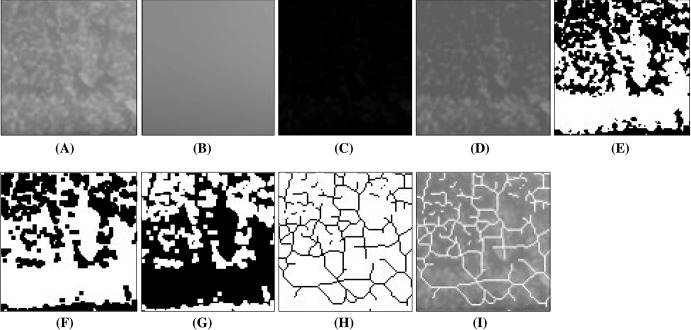 | Fig. 2Fractal dimension analysis process. A. Region of interest. B. Result of blurring of (A). C. Result of subtracting (B) from (A). D. Result of adding 128 to each pixel position of (C). E. Result of conversion of (D) into a binary image. F. Result of erosion and dilation of (E). G. Result of inversion of (F). H. Result of skeletonizing of (G). I. Result of superpositioning (H) over (A).
|
Statistical analysis
The analyses were conducted by a trained observer, who was a dentist with expertise in oral radiology. Intra-examiner reproducibility was assessed by reanalysis of 10% of the sample, performed 2 weeks after the initial analysis to reduce memory bias, and evaluated using the intraclass correlation coefficient (ICC). Another trained observer carried out analyses of 10% of the sample, and inter-examiner reproducibility was determined using the ICC as well.
The characteristics of the subjects and their oncological treatment were analyzed descriptively. The data distribution was assessed using the Shapiro-Wilk test, and the pixel intensity and fractal dimension values before and after radiotherapy were analyzed using the Wilcoxon sign-rank test. The statistical analysis was carried out using BioEstat 5.3 software (Instituto de Desenvolvimento Sustentável Mamirauá, Amazonas, Brazil) with a 5% significance level.
Go to :

Results
Thirty individuals were selected for the study, resulting in a total of 60 digital panoramic radiographs. Most of these individuals were male (80%), had a primary tumor located in the pharynx (43.4%), and had received a total radiation dose of 70 Gy (66.7%). The most common interval separating the pre- and post-radiotherapy radiographs was 12 to 24 months (43.4%). More detailed information on the sample is provided in
Table 1.
Table 1
Demographic and clinical characteristics of the participants


The normal distribution was rejected for the pixel intensity data before (P=0.088) and after radiotherapy (P=0.3081) and for the fractal dimension data after radiotherapy (P=0.3851). Intra- and extra-examiner reproducibility were confirmed for both pixel intensity (ICC, 0.89; P=0.001) and fractal dimension (ICC, 0.81; P=0.01) evaluations.
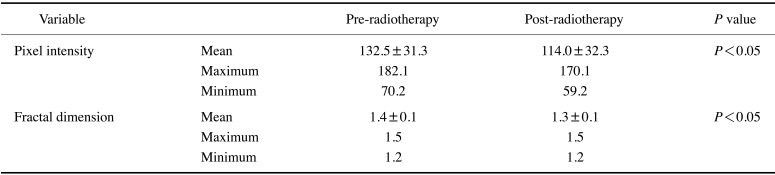
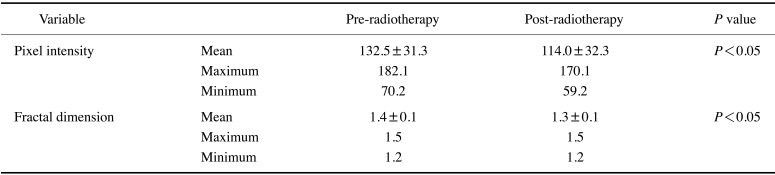
The mean values of pixel intensity before and after radiotherapy were 132.5±31.3 and 114.0±32.3, respectively, constituting a statistically significant difference (
P=0.0368). The mean fractal dimension values pre- and post-radiotherapy were 1.4±0.1 and 1.3±0.1, respectively, similarly presenting a statistically significant difference (
P=0.0495). Detailed information on the analyses is provided in
Table 2.
Table 2
Mean pixel intensity and fractal dimension values on pre- and post-radiotherapy radiographs in head and neck cancer patients

Go to :

Discussion
Bone quality is determined by the tissue microarchitecture and the degree of mineralization. Low bone quality has been directly associated with the failure of dental implants, since primary stability and osseointegration are influenced to a large extent by the characteristics of the surrounding bone.
4 Evidence has shown that patients with osteoporosis experience more rapid development and greater severity of periodontal disease, as well as a lower accumulated long-term survival rate of dental implants
12 and a higher risk of fractures, than individuals without osteoporosis.
13
The present study investigated the characteristics of mandibular bone tissue on digital panoramic radiographs, which are commonly used imaging exams in dental practice. Scientific evidence supports the use of digital panoramic radiography for the analysis of bone tissue, despite limitations inherent to the technique concerning tissue properties, such as software and image receptor configuration, parameters of the radiographic device (such as peak kilovoltage, exposure time, and current), and overlap of tissues and structures.
6 Dual-energy X-ray absorptiometry is a costly gold-standard exam for the diagnosis of osteoporosis. Panoramic radiographs can detect a reduction in mandibular mineral density at a lower cost, which allows early systemic diagnosis and prompt referral to a specialized professional.
14
A pixel is a single digital point with a variable intensity, constituting the smallest unit of an image that can be represented or controlled. In a grayscale radiographic image, the value of each pixel provides information about intensity alone.
15 For pixel intensity analysis for the indirect measurement of local bone mass, some authorities have suggested methods to normalize variations in noise and image production that could influence the comparison between radiographs obtained with the same devices and parameters, with these methods including density markers,
5 binarization, and skeletonization.
15 Herein, the direct use of histograms in ImageJ seemed to be satisfactory, making the procedures even quicker and simpler.
Analysis of the fractal dimension is a low-cost, easily applicable, non-invasive, and accurate method for quantifying the interface pattern of trabecular bone and bone marrow, with higher values indicating a more complex structure.
10 It is a technique used to identify scale-invariant structures that are not affected by the conditions under which radiographic images are produced.
89 However, a range of dental radiographic processing methods have been developed as adaptations of the original article by White and Rudolph,
11 which was used as a reference in our study.
Another conflicting point in the literature relates to the mandibular site used to determine the ROI and its size. The anterior region of the mandible seems to produce relatively inaccurate images due to the overlap of the cervical spine and relatively high likelihood of blurring.
16 In our study, we used the angle of the mandible below the mandibular canal and posterior to the molar region to avoid interference caused by masticatory stress, as proposed by Oliveira et al.,
15 and to provide bone structure even in fully edentulous aged individuals with extremely atrophic mandibles. However, this area is subject to the overlapping of other anatomical structures, such as the airways, tonsils, soft palate, tongue, and hyoid bone.
5 To date, ROI dimensions have not been standardized. The protocol proposed by Tosoni et al.
5 (100×100 pixels) was satisfactory for all individuals examined in our study and provided a suitable medullary bone area for the analyses.
Radiotherapy is an important and efficient therapeutic modality for head and neck cancer, although it also affects non-neoplastic cells in or adjacent to the irradiated area. Its effects may occur during or immediately after irradiation (acute effects) or even months or years later (late effects).
1718 Our results demonstrated that 3D conformational radiotherapy significantly affected subjects' trabecular microarchitecture and the mandibular bone mass. One hypothesis to explain this phenomenon is that intraosseous vascularization decreases as a result of exposure to ionizing radiation, with changes in the bone cell pool, progressive fibrosis, and local necrosis.
3 These alterations manifest radiologically as low bone mineral density, trabecular fracture, and loss and destruction of cortical structures.
4 Nevertheless, the various studies and models addressing this subject have presented highly heterogeneous methods and samples. It is therefore very difficult to realistically compare them and apply the results to humans.
19
To the best of our knowledge, this is the first study to investigate the impact of radiotherapy on the mandibular bone tissue of head and neck cancer patients using pixel intensity and fractal dimension analyses of digital panoramic radiographs. As limitations and suggestions for future research, some points need to be taken into account. First, further studies should consider using more representative sample sizes. In addition, accurate data on the total radiation dose received by each patient in the ROI should be provided to determine the association between the amount of ionizing radiation received and the level of bone tissue damage. Furthermore, because this was a retrospective study, the interval between the pre- and post-radiotherapy radiographs was not standardized and ranged from 3 to 35 months. Lastly, analyses of other mandibular areas, bilateral assessment by more than 1 experienced examiner, and the use of other radiographic techniques (e.g., periapical radiography) could provide more accurate and detailed information.
In summary, based on the results of pixel intensity and fractal dimension analyses, this study suggests that 3D conformational radiotherapy for head and neck cancer negatively affected the trabecular microarchitecture and mandibular bone mass.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download