1. International Institute for Population Sciences. National Family Health Survey (NFHS-4): 2015–16. Mumbai: International Institute for Population Sciences;2017.
2. Scrimshaw NS. Effect of infection on nutritional status. Proc Natl Sci Counc Repub China B. 1992; 16:46–64. PMID:
1631245.
3. Maggini S, Wintergerst ES, Beveridge S, Hornig DH. Selected vitamins and trace elements support immune function by strengthening epithelial barriers and cellular and humoral immune responses. Br J Nutr. 2007; 98 Suppl 1:S29–S35. PMID:
17922955.

4. Suaini NH, Zhang Y, Vuillermin PJ, Allen KJ, Harrison LC. Immune modulation by vitamin D and its relevance to food allergy. Nutrients. 2015; 7:6088–6108. PMID:
26225992.

5. Wacker M, Holick MF. Vitamin D - effects on skeletal and extraskeletal health and the need for supplementation. Nutrients. 2013; 5:111–148. PMID:
23306192.

6. Londhey V. Vitamin D deficiency: Indian scenario. J Assoc Physicians India. 2011; 59:695–696. PMID:
22616334.
7. Harinarayan CV, Ramalakshmi T, Prasad UV, Sudhakar D. Vitamin D status in Andhra Pradesh: a population-based study. Indian J Med Res. 2008; 127:211–218. PMID:
18497434.
8. Harinarayan C, Holick M, Prasad UV, Vani PS, Himabindu G. Vitamin D status and sun exposure in India. Dermatoendocrinol. 2013; 5(1):130–141. PMID:
24494046.

9. Clements MR, Johnson L, Fraser DR. A new mechanism for induced vitamin D deficiency in calcium deprivation. Nature. 1987; 325:62–65. PMID:
3025747.

10. Pettifor JM. Nutritional rickets: deficiency of vitamin D, calcium, or both. Am J Clin Nutr. 2004; 80:1725S–1729S. PMID:
15585795.

11. Khadilkar A, Kadam N, Chiplonkar S, Fischer PR, Khadilkar V. School-based calcium-vitamin D with micronutrient supplementation enhances bone mass in underprivileged Indian premenarchal girls. Bone. 2012; 51:1–7. PMID:
22503722.

12. Lappe JM, Heaney RP. Why randomized controlled trials of calcium and vitamin D sometimes fail. Dermatoendocrinol. 2012; 4:95–100. PMID:
22928064.

13. Kapil U, Jain K. Magnitude of zinc deficiency amongst under five children in India. Indian J Pediatr. 2011; 78:1069–1072. PMID:
21318393.

14. Tupe RP, Chiplonkar SA. Zinc supplementation improved cognitive performance and taste acuity in Indian adolescent girls. J Am Coll Nutr. 2009; 28:388–396. PMID:
20368377.

15. Sivakumar B, Vijayaraghavan K, Vazir S, Balakrishna N, Shatrugna V, Sarma KV, Nair KM, Raghuramulu N, Krishnaswamy K. Effect of micronutrient supplement on health and nutritional status of schoolchildren: study design. Nutrition. 2006; 22(1 Suppl):S1–S7. PMID:
16426958.

16. Thomas T, Eilander A, Muthayya S, McKay S, Thankachan P, Theis W, Gandhe A, Osendarp SJ, Kurpad AV. The effect of a 1-year multiple micronutrient or n-3 fatty acid fortified food intervention on morbidity in Indian school children. Eur J Clin Nutr. 2012; 66:452–458. PMID:
22009072.

17. Ananthakrishnan S, Pani SP, Nalini P. A comprehensive study of morbidity in school age children. Indian Pediatr. 2001; 38:1009–1017. PMID:
11568376.
18. Chowdhury SD, Ghosh T. Nutritional and socioeconomic status in cognitive development of Santal children of Purulia district, India. Ann Hum Biol. 2011; 38:188–193. PMID:
20812884.
19. Manaseki-Holland S, Maroof Z, Bruce J, Mughal MZ, Masher MI, Bhutta ZA, Walraven G, Chandramohan D. Effect on the incidence of pneumonia of vitamin D supplementation by quarterly bolus dose to infants in Kabul: a randomised controlled superiority trial. Lancet. 2012; 379:1419–1427. PMID:
22494826.

20. Aluisio AR, Maroof Z, Chandramohan D, Bruce J, Mughal MZ, Bhutta Z, Walraven G, Masher MI, Ensink JH, Manaseki-Holland S. Vitamin D3 supplementation and childhood diarrhea: a randomized controlled trial. Pediatrics. 2013; 132:e832–e840. PMID:
24019420.

21. Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H. Randomized trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010; 91:1255–1260. PMID:
20219962.

22. Lang PO, Aspinall R. Can we translate vitamin D immunomodulating effect on innate and adaptive immunity to vaccine response. Nutrients. 2015; 7:2044–2060. PMID:
25803545.

23. Kurugöl Z, Bayram N, Atik T. Effect of zinc sulfate on common cold in children: randomized, double blind study. Pediatr Int. 2007; 49:842–847. PMID:
18045283.

24. Müller O, Becher H, van Zweeden AB, Ye Y, Diallo DA, Konate AT, Gbangou A, Kouyate B, Garenne M. Effect of zinc supplementation on malaria and other causes of morbidity in west African children: randomised double blind placebo controlled trial. BMJ. 2001; 322:1567. PMID:
11431296.
25. Somé JW, Abbeddou S, Yakes Jimenez E, Hess SY, Ouédraogo ZP, Guissou RM, Vosti SA, Ouédraogo JB, Brown KH. Effect of zinc added to a daily small-quantity lipid-based nutrient supplement on diarrhoea, malaria, fever and respiratory infections in young children in rural Burkina Faso: a cluster-randomised trial. BMJ Open. 2015; 5:e007828.

26. Solar Energy Centre, MNRE. Indian Metrological Department. Typical Climatic Data for Selected Radiation Stations (The Data Period Covered: 1986–2000). Solar Radiation Hand Book (2008) [Internet]. New Delhi: Indian Metrological Department;2008. cited 2017 Oct 28. Available from:
http://www.indiaenvironmentportal.org.in/files/srd-sec.pdf.
27. Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM. Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011; 96:1911–1930. PMID:
21646368.

28. Indian Council of Medical Research. Nutrient Requirements & Recommended Dietary Allowances for Indians. Hyderabad: Expert Group of the Indian Council of Medical Research;2009.
29. Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007; 74:1131–1132. PMID:
18174655.
30. Patwardhan VG, Khadilkar AV, Chiplonkar SA, Mughal ZM, Khadilkar VV. Varying relationship between 25-hydroxy-vitamin D, high density lipoprotein cholesterol, and serum 7-dehydrocholesterol reductase with sunlight exposure. J Clin Lipidol. 2015; 9:652–657. PMID:
26350811.

31. Deb S, Dutta S, Dasgupta A, Misra R. Relationship of personal hygiene with nutrition and morbidity profile: a study among primary school children in South Kolkata. Indian J Community Med. 2010; 35:280–284. PMID:
20922107.

32. Chiplonkar SA, Agte VV, Mengale SS, Tarwadi KV. Are lifestyle factors good predictors of retinol and vitamin C deficiency in apparently healthy adults. Eur J Clin Nutr. 2002; 56:96–104. PMID:
11857042.

33. Khadilkar V, Yadav S, Agrawal KK, Tamboli S, Banerjee M, Cherian A, Goyal JP, Khadilkar A, Kumaravel V, Mohan V, Narayanappa D, Ray I, Yewale V. Indian Academy of Pediatrics Growth Charts Committee. Revised IAP growth charts for height, weight and body mass index for 5- to 18-year-old Indian children. Indian Pediatr. 2015; 52:47–55. PMID:
25638185.

35. Longvah T, Ananthan R, Bhaskarachary K, Venkaiah K. National Institute of Nutrition. Longvah T, editor. Indian Food Composition Tables. 1st ed. Hyderabad: National Institute of Nutrition;2017.
36. Chiplonkar SA, Agte VV. Extent of error in estimating nutrient intakes from food tables versus laboratory estimates of cooked foods. Asia Pac J Clin Nutr. 2007; 16:227–239.
37. Brown KH. IZiNCG Technical Brief: Assessing Population Zinc Status with Serum Zinc Concentration. Davis (CA): International Zinc Nutrition Consultative Group;2012.
38. Bruijnzeels MA, Foets M, van der Wouden JC, Prins A, van den Heuvel WJ. Measuring morbidity of children in the community: a comparison of interview and diary data. Int J Epidemiol. 1998; 27:96–100. PMID:
9563701.
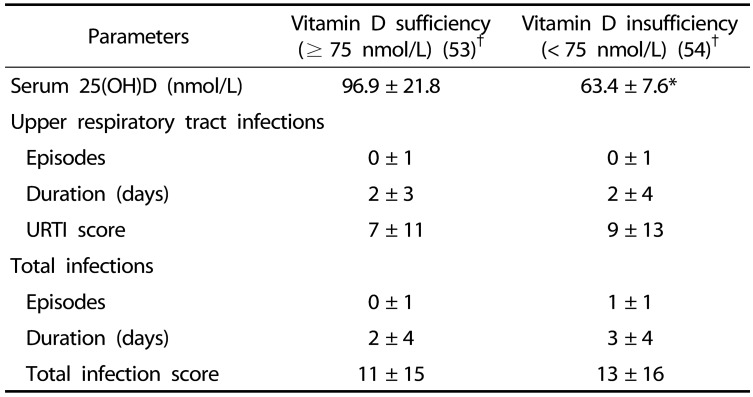
39. Mandlik R, Chiplonkar S, Kajale N, Khadilkar V, Khadilkar A. Infection status of rural schoolchildren and its relationship with Vitamin D concentrations. Indian J Pediatr. 2019; 86:675–680. PMID:
30915647.

40. Camargo CA Jr, Ganmaa D, Frazier AL, Kirchberg FF, Stuart JJ, Kleinman K, Sumberzul N, Rich-Edwards JW. Randomized trial of vitamin D supplementation and risk of acute respiratory infection in Mongolia. Pediatrics. 2012; 130:e561–e567. PMID:
22908115.

41. Shalini CN, Murthy NS, Shalini S, Dinesh R, Shivaraj NS, Suryanarayana SP. Comparison of nutritional status of rural and urban school students receiving midday meals in schools of Bengaluru, India: a cross sectional study. J Postgrad Med. 2014; 60:118–122. PMID:
24823508.

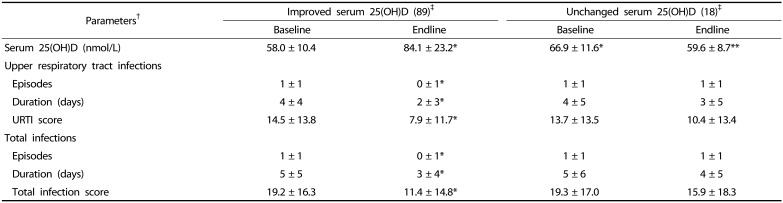
42. Mandlik R, Khadilkar A, Kajale N, Ekbote V, Patwardhan V, Mistry S, Khadilkar V, Chiplonkar S. Response of serum 25(OH)D to Vitamin D and calcium supplementation in school-children from a semi-rural setting in India. J Steroid Biochem Mol Biol. 2018; 180:35–40. PMID:
29247782.

43. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Griffiths CJ, Janssens W, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S Jr, Stelmach I, Kumar GT, Urashima M, Camargo CA Jr. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017; 356:i6583. PMID:
28202713.

44. Mayo-Wilson E, Junior JA, Imdad A, Dean S, Chan XH, Chan ES, Jaswal A, Bhutta ZA. Zinc supplementation for preventing mortality, morbidity, and growth failure in children aged 6 months to 12 years of age. Cochrane Database Syst Rev. 2014; CD009384. PMID:
24826920.

45. Moran VH, Stammers AL, Medina MW, Patel S, Dykes F, Souverein OW, Dullemeijer C, Pérez-Rodrigo C, Serra-Majem L, Nissensohn M, Lowe NM. The relationship between zinc intake and serum/plasma zinc concentration in children: a systematic review and dose-response meta-analysis. Nutrients. 2012; 4:841–858. PMID:
23016120.






 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download