This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Postoperative nausea and vomiting is one of the most common side effects after anesthesia in surgeries, such as cesarean section. This study aimed to investigate the effect of ginger and metoclopramide in the prevention of nausea and vomiting during and after cesarean section.
Methods
This clinical trial was conducted on 180 patients aged 18–40 years who underwent cesarean section under spinal anesthesia. The first group received 10 mg of metoclopramide via intravenous injection (metoclopramide group), and the second group received 1 g of oral ginger (ginger group) half an hour before spinal anesthesia. The frequency and severity of nausea and vomiting during surgery and at 2, 6, 12, and 24 hours postoperatively were compared in both groups. To analyze the results, the t-test, chi-square test, and Mann-Whitney test were used.
Results
There was no significant difference in the frequency of nausea and vomiting between the 2 groups during operation, 2 hours and 6 hours after surgery (P=0.182, 0.444 and 0.563 respectively). The severity of nausea and vomiting was also similar in the 2 groups (P=0.487 and 0.652 respectively); however, the metoclopramide group had a lower systolic blood pressure (P<0.001; df=2.176; f=18.66) and mean arterial pressure (P<0.001; df=2.176; f=6.36) than the ginger group.
Conclusion
The results revealed that ginger reduced nausea and vomiting to the same extent as metoclopramide in patients undergoing cesarean section.
Keywords: Cesarean section, Spinal anesthesia, Metoclopramide, Ginger
Introduction
Cesarean section is one of the most common surgical procedures conducted on women. Cesarean delivery is the delivery of a fetus through an incision into the abdominal cavity (laparotomy) and uterine wall (hysterotomy) [
1].
Currently, a large number of cesarean sections are performed under local anesthesia. The decision for local anesthesia depends on the patient's preference and the absence of fetal distress. General anesthesia in the presence of fetal distress is sometimes preferred because of faster preparation time and lower incidence of hypotension. However, local (epidural or spinal) anesthesia is associated with a lower probability of maternal pulmonary aspiration or fetal impairment from transplacental exposure to anesthetics. Spinal anesthesia is the most commonly selected method of anesthesia for elective cesarean section. Its use is widely accepted owing to its simplicity and high reliability as well as its rapid time-to-effect. Epidural anesthesia is an alternative technique and has the advantage of reduced rates of hypotension [
2].
Considering that one of the common causes of death during general anesthesia is complications from intubation (with the incidence approximately 10 times higher in pregnant women than in non-pregnant women), the American College of Obstetricians and Gynecologists released a statement in 2013 advising local anesthesia as the preferred method for cesarean procedures [
12].
Postoperative nausea and vomiting (PONV) is one of the most common side effects of local anesthesia, with a prevalence of 1–43%. In another study, the prevalence of PONV varied from 23% to 79% [
1]. The rates are dependent on the type of surgery, anesthesia method, patients’ sex and age, obesity, preoperative fasting rates, and history of PONV [
3].
The causes of nausea include hypotension resulting from local anesthesia; decreased cardiac output due to compression of the aorta and abdominal organs; visceral manipulation, such as removal of the uterus; and use of anesthetic medications, such as opioids or methylergonovine. While PONV can occur under both general anesthesia and local anesthesia, this side effect is more evident in the latter [
4]. Numerous studies have been conducted to address nausea and vomiting during and after cesarean section with the use of spinal anesthesia [
2356].
Nausea and vomiting is stressful for patients who have experienced it. The complications of PONV include dehydration, weakness, rupture of surgical sutures, and increased bleeding on the surgical site, all ultimately delaying the discharge of patients and increasing the cost of care. For the past 50 years, various agents have been identified for the treatment of PONV [
4].
One frequently used anti-emetic is metoclopramide, which has a centrally acting anti-dopaminergic effect and an anti-serotonergic effect at high doses. A low dose (10 mg) has no reliable anti-nausea effect for PONV prophylaxis in non-pregnant women undergoing non-obstetric surgery; however, this dose is reported to be safe for pregnant women. Moreover, it allows trans-placental absorption; thus, no significant effects on the fetus have been found at this dose [
1].
Conversely, a less commonly used anti-emetic is ginger. In recent decades, ginger (classified by the Food and Drug Administration [FDA] as one of the safest herbal medicines) has been shown to be beneficial in controlling nausea and vomiting in pregnant women, patients undergoing chemotherapy, and those with motion sickness and PONV [
35].
Traditional treatments have many advantages, including wide variety of effects, flexibility in dosing and route, availability worldwide, wide acceptance, low cost, and less dependence on technology. Ginger is considered effective mainly owing to its active compounds, which include shogaol and gingerol. It also has anti-inflammatory, anti-nausea, anti-cancer, and anti-hypertensive effects, and decreases the production of prostaglandins and digestive problems. Moreover, it is on the United States FDA list of safe herbal preparations and has no adverse effect on the fetus [
4].
Considering the high rate of cesarean section and side effects of metoclopramide, including sedation, hypotension, and extrapyramidal side effects, alternatives for nausea control in cesarean section are warranted. This study aimed to investigate the effectiveness between ginger and metoclopramide for the prevention of nausea and vomiting during and after cesarean section as well as evaluate the efficacy and complication rates of these medications.
Materials and methods
This randomized, double-blind clinical trial was conducted from March 2016 to August 2016 after obtaining approval from the local ethics committee of Qazvin University of Medical Sciences in Kowsar Training-Therapeutic Hospital. After written consent was obtained, the patients were randomized into 2 groups. This clinical trial was conducted on 180 patients aged 18–40 years who underwent cesarean section under spinal anesthesia. The indication of cesarean section for all mothers was previous cesarean section, and none of them had absolute indications (absolute disproportion, chorioamnionitis, maternal pelvic deformity, eclampsia, HELLP syndrome, fetal asphyxia, fetal acidosis, umbilical cord prolapse, placenta previa, abnormal lie and presentation, or uterine rupture).
Randomization was performed using a computerized random number generator, which divided the cohort into 2 groups. The intervention group received 2 ginger tablets equivalent to 1,000 mg produced by the Dina Qazvin Pharmaceuticals Company, with a small amount of water, and 2 mL of normal saline through intravenous injection half an hour before surgery (ginger group). The control group received 1 ampule of metoclopramide equivalent to 10 mg obtained from the Razi Pharmaceuticals Company through intravenous injection and 2 oral placebo tablets instead of ginger with a small amount of water half an hour before the start of the spinal anesthesia (metoclopramide group).
The exclusion criteria were as follows: sensitivity to metoclopramide and ginger; history of cardiac, upper gastrointestinal tract, or biliary surgeries; history of any hemorrhagic disorder, such as hemophilia; contraindication to intrathecal and epidural anesthesia; high risk for anesthesia (American Society of Anesthesiologists classification III and IV); and history of use of multiple doses of anti-nausea medications and metoclopramide 24 hours before surgery.
All mothers were hydrated with 500–1,000 mg lactated ringers before surgery. After standard monitoring (electrocardiogram, blood pressure, and pulse oximetry), spinal anesthesia was induced using 2.5 mL of 0.5% bupivacaine through intrathecal injection. After spinal anesthesia, no patients were administered with narcotics. Immediately after spinal anesthesia and then every 5 minutes, blood pressure and heart rate were measured in all patients. In cases of ≥20% drop in blood pressure, 2.5–5 mg of ephedrine was injected. In the postoperative period, ondansetron was administered to control breakthrough nausea and vomiting (as needed). The patients were then instructed to report nausea and vomiting. The frequency of nausea and vomiting during surgery and postoperatively at 2, 6, 12, and 24 hours were evaluated.
The participants were trained to evaluate the severity of nausea using a 10-cm ruler as the visual analog scale tool, with one end indicating severe nausea and the other indicating no nausea (desirable state). The severity of nausea was measured as mild (lower than 3.5), moderate (3.5–7), and severe (higher than 7). This tool has been used in several other studies, with a validity of 40–95% (7). In addition, the incidence of vomiting in the first 6 postoperative hours was defined as mild (lower than 3 times), moderate (3–5 times), and severe (higher than 5 times).
The data were analyzed using SPSS 19 (SPSS Inc, Chicago, IL, USA). The
t-test and chi-square test were used for data analysis. Based on a confidence interval of 95%, power of 80%, and expected incidence of nausea of 5% in the intervention group and 20% in the control group, the sample size calculated was 73 patients in each group. To restitute for an estimated percentage of follow-up loss of 20%, 90 patients were needed for each group [
7]. For all tests,
P-values of <0.05 were considered significant.
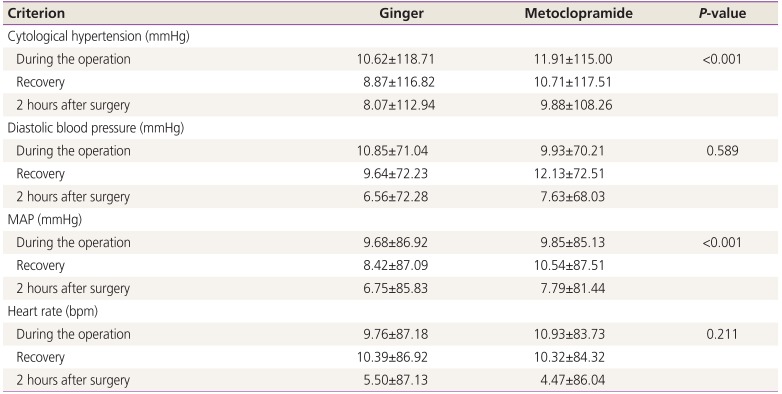
Results
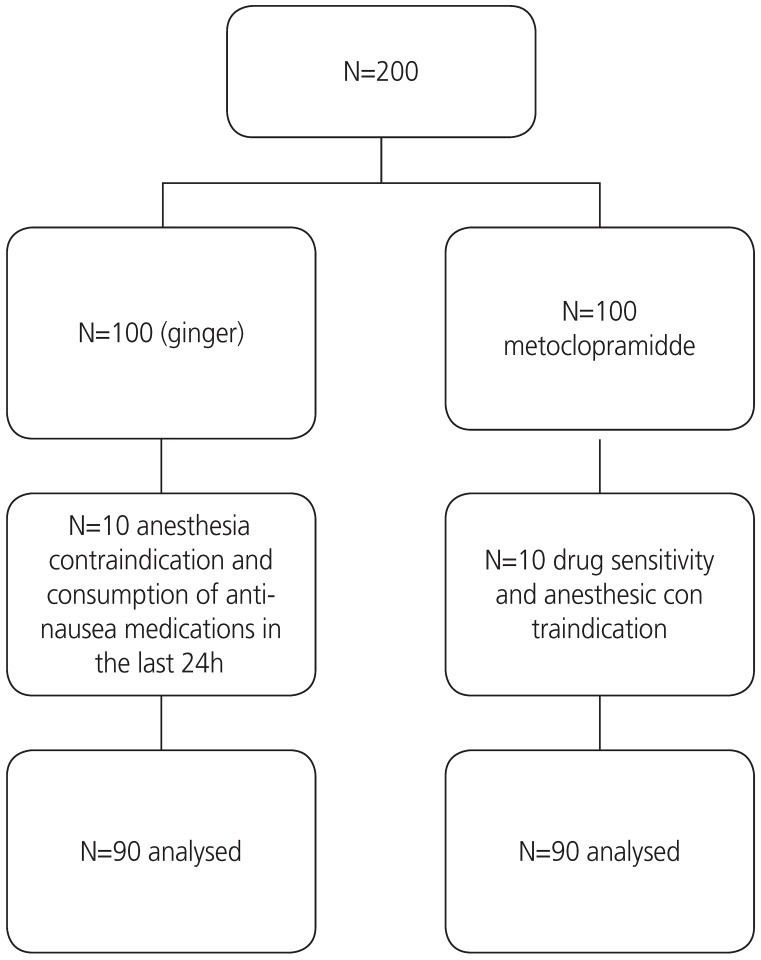
This study was registered at the Iranian Center for Clinical Trials (IRCT201611028611N3) after receiving approval from the local ethics committee of Qazvin University of Medical Sciences. A total of 200 pregnant women were recruited; 20 were excluded from the study (10 in each group), and 90 subjects in each group were finally included in the study (
Fig. 1).
Fig. 1
CONSORT diagram.
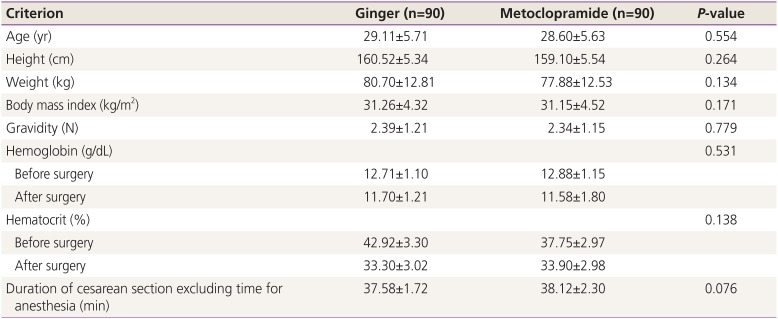
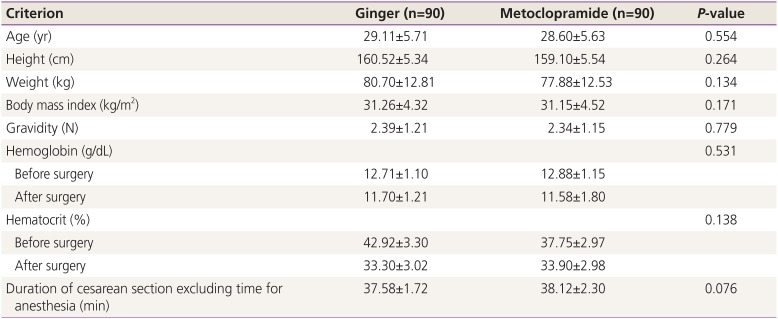
The demographic data of the study population were not significantly different (
Table 1).
Table 1
Demographic data of the study population divided into 2 groups
|
Criterion |
Ginger (n=90) |
Metoclopramide (n=90) |
P-value |
|
Age (yr) |
29.11±5.71 |
28.60±5.63 |
0.554 |
|
Height (cm) |
160.52±5.34 |
159.10±5.54 |
0.264 |
|
Weight (kg) |
80.70±12.81 |
77.88±12.53 |
0.134 |
|
Body mass index (kg/m2) |
31.26±4.32 |
31.15±4.52 |
0.171 |
|
Gravidity (N) |
2.39±1.21 |
2.34±1.15 |
0.779 |
|
Hemoglobin (g/dL) |
|
|
0.531 |
|
Before surgery |
12.71±1.10 |
12.88±1.15 |
|
|
After surgery |
11.70±1.21 |
11.58±1.80 |
|
|
Hematocrit (%) |
|
|
0.138 |
|
Before surgery |
42.92±3.30 |
37.75±2.97 |
|
|
After surgery |
33.30±3.02 |
33.90±2.98 |
|
|
Duration of cesarean section excluding time for anesthesia (min) |
37.58±1.72 |
38.12±2.30 |
0.076 |
The history of nausea and vomiting at the beginning of pregnancy was evaluated. There were 23 patients (25.5%) in the ginger group and 20 patients (22.2%) in the metoclopramide group (P=0.185); however, there was no significant difference between them.
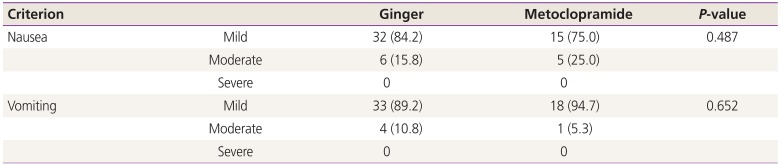
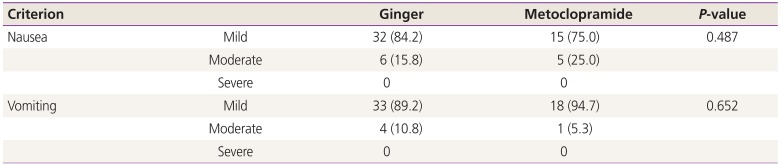
The severity of nausea in the first 6 postoperative hours was investigated (
Table 2). As shown in
Table 2, there was no significant difference in the severity of nausea and vomiting between the 2 groups (
P=0.487 and 0.652, respectively).
Table 2
Relative severity of nausea and vomiting in the first 6 postoperative hours in the 2 groups
|
Criterion |
Ginger |
Metoclopramide |
P-value |
|
Nausea |
Mild |
32 (84.2) |
15 (75.0) |
0.487 |
|
Moderate |
6 (15.8) |
5 (25.0) |
|
|
Severe |
0 |
0 |
|
|
Vomiting |
Mild |
33 (89.2) |
18 (94.7) |
0.652 |
|
Moderate |
4 (10.8) |
1 (5.3) |
|
|
Severe |
0 |
0 |
|
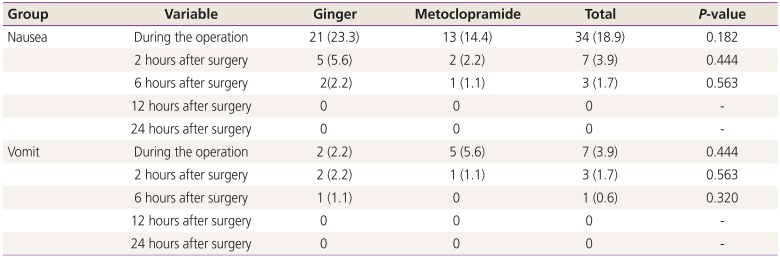
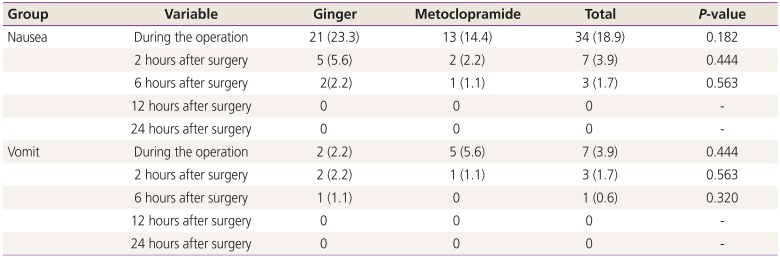
The frequency of nausea and vomiting during and after cesarean section between the 2 groups was not significantly different (
Table 3).
Table 3
Comparison of the mean frequency of nausea and vomiting during and after surgery between the 2 groups
|
Group |
Variable |
Ginger |
Metoclopramide |
Total |
P-value |
|
Nausea |
During the operation |
21 (23.3) |
13 (14.4) |
34 (18.9) |
0.182 |
|
|
2 hours after surgery |
5 (5.6) |
2 (2.2) |
7 (3.9) |
0.444 |
|
|
6 hours after surgery |
2 (2.2) |
1 (1.1) |
3 (1.7) |
0.563 |
|
|
12 hours after surgery |
0 |
0 |
0 |
- |
|
|
24 hours after surgery |
0 |
0 |
0 |
- |
|
Vomit |
During the operation |
2 (2.2) |
5 (5.6) |
7 (3.9) |
0.444 |
|
|
2 hours after surgery |
2 (2.2) |
1 (1.1) |
3 (1.7) |
0.563 |
|
|
6 hours after surgery |
1 (1.1) |
0 |
1 (0.6) |
0.320 |
|
|
12 hours after surgery |
0 |
0 |
0 |
- |
|
|
24 hours after surgery |
0 |
0 |
0 |
- |
The use of ondansetron for breakthrough vomiting during and after surgery was also not significantly different between them (P=0.12).
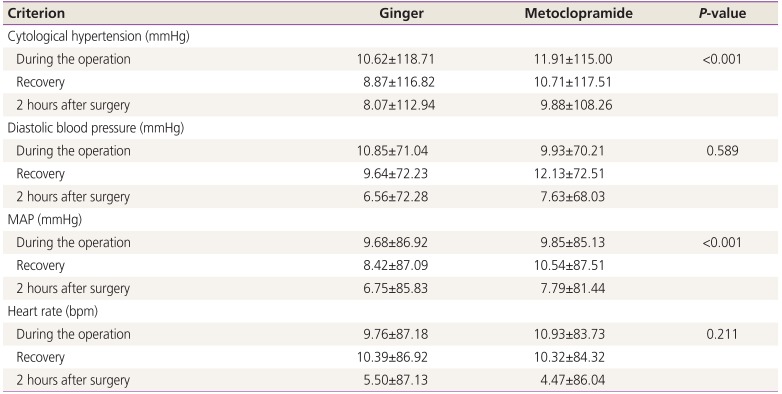
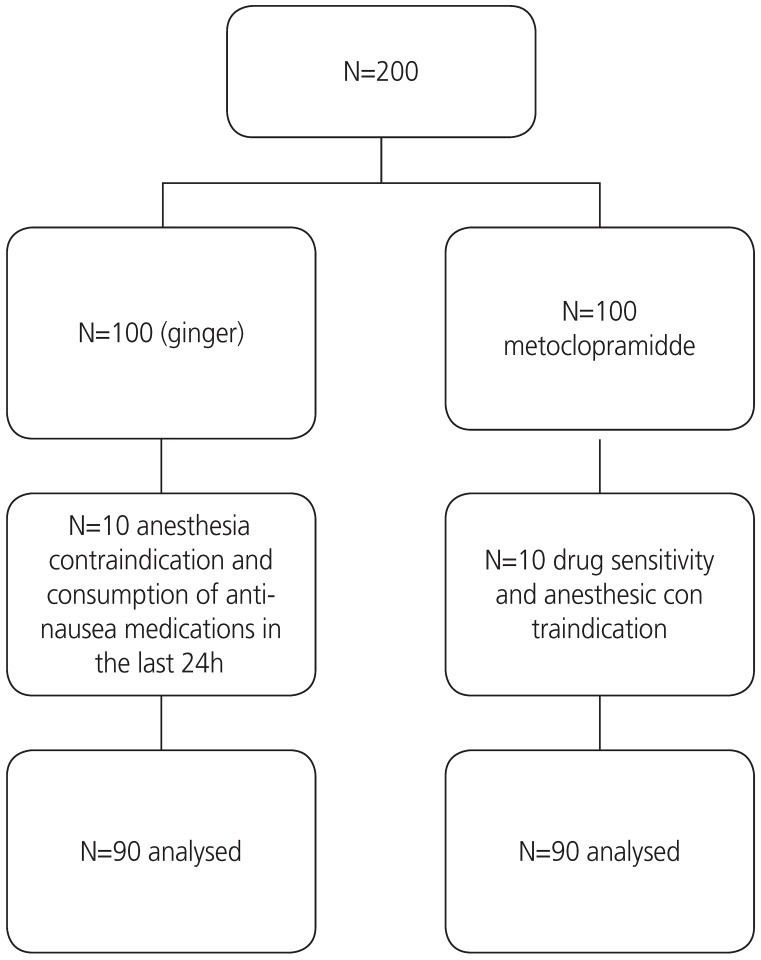
However, as shown in
Table 4, the metoclopramide group had a lower systolic blood pressure (
P<0.001; df=2.176; f=18.66) and mean arterial pressure (
P<0.001; df=2.176; f=6.36) than the ginger group.
Table 4
Comparison of the mean systolic and diastolic blood pressures, MAP, and heart rate during pregnancy in the 2 groups
|
Criterion |
Ginger |
Metoclopramide |
P-value |
|
Cytological hypertension (mmHg) |
|
|
|
|
During the operation |
118.71±10.62 |
115.00±11.91 |
<0.001 |
|
Recovery |
116.82±8.87 |
117.51±10.71 |
|
|
2 hours after surgery |
112.94±8.07 |
108.26±9.88 |
|
|
Diastolic blood pressure (mmHg) |
|
|
|
|
During the operation |
71.04±10.85 |
70.21±9.93 |
0.589 |
|
Recovery |
72.23±9.64 |
72.51±12.13 |
|
|
2 hours after surgery |
72.28±6.56 |
68.03±7.63 |
|
|
MAP (mmHg) |
|
|
|
|
During the operation |
86.92±9.68 |
85.13±9.85 |
<0.001 |
|
Recovery |
87.09±8.42 |
87.51±10.54 |
|
|
2 hours after surgery |
85.83±6.75 |
81.44±7.79 |
|
|
Heart rate (bpm) |
|
|
|
|
During the operation |
87.18±9.76 |
83.73±10.93 |
0.211 |
|
Recovery |
86.92±10.39 |
84.32±10.32 |
|
|
2 hours after surgery |
87.13±5.50 |
86.04±4.47 |
|
The analysis showed that there was no side effect of the medication according to the dose in either group, including heart burn in the ginger group and extrapyramidal side effect in the metoclopramide group.
Discussion
This study showed that there was no significant difference in the frequency and severity of nausea and vomiting between the 2 study groups. Furthermore, metoclopramide reduced the blood pressure more than did ginger, although this difference may be not clinically meaningful.
The results of the present study demonstrate that both ginger and metoclopramide decrease the frequency and severity of nausea and vomiting in all stages of cesarean section; however, ginger demonstrates superior hemodynamic stability compared with metoclopramide. The results contradict those of Kalava et al. [
8] in terms of the effect of ginger; this difference may be attributed to the changes in the medication doses. Conversely, our results agree with those of Montazeri et al. [
4] who conducted a study on 160 patients undergoing various surgical procedures using general anesthesia as well as spinal and epidural anesthesia and showed that the rate of nausea in the first 2 postoperative hours was significantly lower in their low ginger-receiving group.
Amouee et al. [
9] compared between the effects of ginger and placebo on the severity of PONV; they found that the mean score of nausea at 2, 4, and 6 postoperative hours in the ginger group was lower than that in the placebo group. Finally, they showed that the use of ginger in preventing postoperative nausea has been effective and that ginger can be used as an anti-nausea medicine after surgery. The results are consistent with those of our study [
9].
Lee and Shin [
10] performed a study in South Korea and investigated the effect of ginger anesthesia oil on reducing nausea and vomiting after abdominal surgery. Their analysis showed that the scores of nausea and vomiting were significantly lower in the ginger-receiving group than in the control group. Although their results are consistent with those of the present study, the type of medication used for the intervention groups was different.
In terms of the confirmation of an effective dose of metoclopramide in preventing PONV, De Oliveira et al. [
11] conducted a meta-analysis of 30 clinical trials involving 3,328 individuals to investigate the efficacy of administration of 10 mg of metoclopramide before induction of anesthesia. They showed that this dose more effectively prevented PONV in cases of general anesthesia and local anesthesia [
11].
Mishriky and Habib [
1] conducted a meta-analysis in the United States on pregnant women undergoing cesarean section. They showed that metoclopramide at a dose of 10 mg administered half an hour before induction of anesthesia reduced the rate of nausea and vomiting during and after surgery [
1]. Their results are consistent with those of the present study.
Our study showed that ginger significantly reduced the severity of nausea and vomiting, similar to metoclopramide. Although many studies have compared the effects of each of these 2 medications with those of various medications on nausea and vomiting during and after surgery [
1], only 1 study has investigated the effect of ginger and metoclopramide on nausea and vomiting during and after surgery [
12].
Our study showed that ginger and metoclopramide had the same effect in reducing nausea and vomiting during and after surgery, which is in contrast with the results of Moslem et al. [
12]. There are many differences between their study and the present study, including the type of sampling, type of anesthesia, age and sex of the subjects, sample size, dose of the medications, and method of prescribing the medications. In their study, patients aged 18–80 years undergoing cholecystectomy under general anesthesia were included; further, both male and female patients were recruited. The dose of metoclopramide was different, and it was administered orally. In our study, patients aged 18–40 years undergoing cesarean section under spinal anesthesia were included, and a sample size of 180 patients was selected; the patients received metoclopramide at a dose of 10 mg through intravenous injection. The factor that may have caused the same effect between ginger and metoclopramide in our study was the oral administration of ginger and intravenous administration of metoclopramide within half an hour before the surgery; owing to the faster effect of intravenous administration of metoclopramide compared with that of oral administration of ginger, the 2 medications were identical in reducing nausea and vomiting during and after surgery.
According to previous studies, a dose of 1 g of ginger and 10 mg of metoclopramide does not affect the fetus and the Apgar score. The effect of these medications on the gastrointestinal tract is attributed to their direct effect without affecting the strength and resistance of the sphincter and on the central nervous system [
8].
The present study also indicated that the systolic and diastolic blood pressures and mean arterial pressure (MAP) in the metoclopramide group after surgery were significantly lower than those in the ginger group, although these differences may not be clinically meaningful. Previous studies have reported no association of the systolic and diastolic blood pressures or MAP with metoclopramide intake.
The cause of decreased systolic and diastolic blood pressures and MAP in the metoclopramide group can be attributed to the antagonistic effects of dopamine on blood pressure. Given that dopamine is a medication used to increase blood pressure, it is possible that the antagonistic effects of metoclopramide have an additive effect of reducing blood pressure in patients who are simultaneously under spinal anesthesia. Therefore, ginger appears to be safer in this respect than metoclopramide in pregnant women who need to undergo cesarean section under spinal anesthesia.
Prior to this study, no study has compared between traditional pharmaceutical medications and herbal supplements to reduce nausea and vomiting; thus, this is one of the strengths of the present study.
In this study, both groups were the same, and the confounding factors were reduced as much as possible. Considering the results of this study and other studies that report the effects of the use of ginger in reducing PONV, ginger is then recommended in controlling nausea and vomiting in pregnant women undergoing cesarean section under local anesthesia compared with metoclopramide owing to its hemodynamic instability.
It is also recommended that similar studies be conducted on the use of different doses of ginger to identify the ideal dose and compare the effect with that of other commonly used medications. Therefore, the results of this study can be used as a basis for conducting a more comprehensive research with a larger sample size.
In future, similar studies on patients undergoing cesarean section under general anesthesia are needed to achieve more comprehensive results.
In conclusion, the results showed that both ginger and metoclopramide reduce nausea and vomiting in patients undergoing cesarean section to a similar extent; however, metoclopramide has more potential for hemodynamic instability. It can be concluded that ginger is a simple, low-cost, and safe supplementary anti-emetic medication for controlling PONV in patients undergoing cesarean section under spinal anesthesia.
Acknowledgements
This study was based on the doctoral dissertation by Dr. Aynaz Bostan. We sincerely appreciate the cooperation of the Health Deputy of Qazvin University of Medical Sciences and the Center for Clinical Research and Development of Kowsar Hospital. We would also like to thank Zahra Mohammadi for her help with the statistical data analysis and Dr. Maryam Palizdar for her cooperation.
References
1. Mishriky BM, Habib AS. Metoclopramide for nausea and vomiting prophylaxis during and after caesarean delivery: a systematic review and meta-analysis. Br J Anaesth. 2012; 108:374–383. PMID:
22307240.

2. Tobi KU, Imarengiaye CO, Amadasun FE. The effects of dexamethasone and metoclopramide on early and late postoperative nausea and vomiting in women undergoing myomectomy under spinal anaesthesia. Niger J Clin Pract. 2014; 17:449–455. PMID:
24909468.

3. Arslan M, Ozdemir L. Oral intake of ginger for chemotherapy-induced nausea and vomiting among women with breast cancer. Clin J Oncol Nurs. 2015; 19:E92–E97. PMID:
26414587.

4. Montazeri AS, Hamidzadeh A, Raei M, Mohammadiun M, Montazeri AS, Mirshahi R, et al. Evaluation of oral ginger efficacy against postoperative nausea and vomiting: a randomized, double-blinded clinical trial. Iran Red Crescent Med J. 2013; 15:e12268. PMID:
24693389.

5. Panahi Y, Saadat A, Sahebkar A, Hashemian F, Taghikhani M, Abolhasani E. Effect of ginger on acute and delayed chemotherapy-induced nausea and vomiting: a pilot, randomized, open-label clinical trial. Integr Cancer Ther. 2012; 11:204–211. PMID:
22313739.
6. Mohamed F, Firas D, Riadh B, Walid D, Lasaad S, Abdelhamid K. Combined use of metoclopramide and dexamethasone as a prophylactic antiemetic in elective cesarean section under spinal anesthesia. Middle East J Anaesthesiol. 2012; 21:829–834. PMID:
23634564.
7. Beck JV, Arnold KJ. Parameter estimation in engineering and science. New York (NY): Wiley;1977.
8. Kalava A, Darji SJ, Kalstein A, Yarmush JM, SchianodiCola J, Weinberg J. Efficacy of ginger on intraoperative and postoperative nausea and vomiting in elective cesarean section patients. Eur J Obstet Gynecol Reprod Biol. 2013; 169:184–188. PMID:
23510951.

9. Amouee M, Montazeri S, Zadeh RA, Ghorbani M. The effect of ginger capsule on nausea and vomiting during and after caesarean section under spinal anesthesia. Int J Clin Med. 2016; 7:106–112.

10. Lee YR, Shin HS. Effectiveness of ginger essential oil on postoperative nausea and vomiting in abdominal surgery patients. J Altern Complement Med. 2017; 23:196–200. PMID:
27841938.

11. De Oliveira GS Jr, Castro-Alves LJ, Chang R, Yaghmour E, McCarthy RJ. Systemic metoclopramide to prevent postoperative nausea and vomiting: a meta-analysis without Fujii's studies. Br J Anaesth. 2012; 109:688–697. PMID:
23015617.

12. Moslem A, Nemat-Shahi M, Asadi A, Keikhosravi A, Azhdari-Zarmehri H. Comparison of the effect of ginger and metoclopramide in prevention of nausea and vomiting after cholecystectomy. Majallahi Danishkadahi Pizishkii Isfahan. 2016; 34:1121–1127.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download