1. Sami Walid M, Heaton RL. The role of laparoscopic myomectomy in the management of uterine fibroids. Curr Opin Obstet Gynecol. 2011; 23:273–277. PMID:
21666469.

2. Wise LA, Laughlin-Tommaso SK. Epidemiology of uterine fibroids: from menarche to menopause. Clin Obstet Gynecol. 2016; 59:2–24. PMID:
26744813.
3. Semm K. New methods of pelviscopy (gynecologic laparoscopy) for myomectomy, ovariectomy, tubectomy and adnectomy. Endoscopy. 1979; 11:85–93. PMID:
156118.

4. Di Gregorio A, Maccario S, Raspollini M. The role of laparoscopic myomectomy in women of reproductive age. Reprod Biomed Online. 2002; 4(Suppl 3):55–58. PMID:
12470567.

5. Gutt CN, Oniu T, Schemmer P, Mehrabi A, Büchler MW. Fewer adhesions induced by laparoscopic surgery? Surg Endosc. 2004; 18:898–906. PMID:
15108105.

6. Jain N. Multiple layer closure of myoma bed in laparoscopic myomectomy. J Gynecol Endosc Surg. 2011; 2:43–46. PMID:
22442535.

7. Ramesh B, Vidyashankar M, Bharathi B. Single incision laparoscopic myomectomy. J Gynecol Endosc Surg. 2011; 2:61–63. PMID:
22442539.

8. Han CM, Lee CL, Su H, Wu PJ, Wang CJ, Yen CF. Single-port laparoscopic myomectomy: initial operative experience and comparative outcome. Arch Gynecol Obstet. 2013; 287:295–300. PMID:
22990477.

9. Kim SK, Lee JH, Lee JR, Suh CS, Kim SH. Laparoendoscopic single-site myomectomy versus conventional laparoscopic myomectomy: a comparison of surgical outcomes. J Minim Invasive Gynecol. 2014; 21:775–781. PMID:
24632396.

10. Song T, Kim TJ, Kim WY, Lee SH. Comparison of barbed suture versus traditional suture in laparoendoscopic single-site myomectomy. Eur J Obstet Gynecol Reprod Biol. 2015; 185:99–102. PMID:
25549572.

11. Lee D, Kim SK, Kim K, Lee JR, Suh CS, Kim SH. Advantages of single-port laparoscopic myomectomy compared with conventional laparoscopic myomectomy: a randomized controlled study. J Minim Invasive Gynecol. 2018; 25:124–132. PMID:
28826957.

12. Buchs NC, Ostermann S, Hauser J, Roche B, Iselin CE, Morel P. Intestinal obstruction following use of laparoscopic barbed suture: a new complication with new material? Minim Invasive Ther Allied Technol. 2012; 21:369–371. PMID:
22145693.

13. Lee ET, Wong FW. Small bowel obstruction from barbed suture following laparoscopic myomectomy-a case report. Int J Surg Case Rep. 2015; 16:146–149. PMID:
26454501.

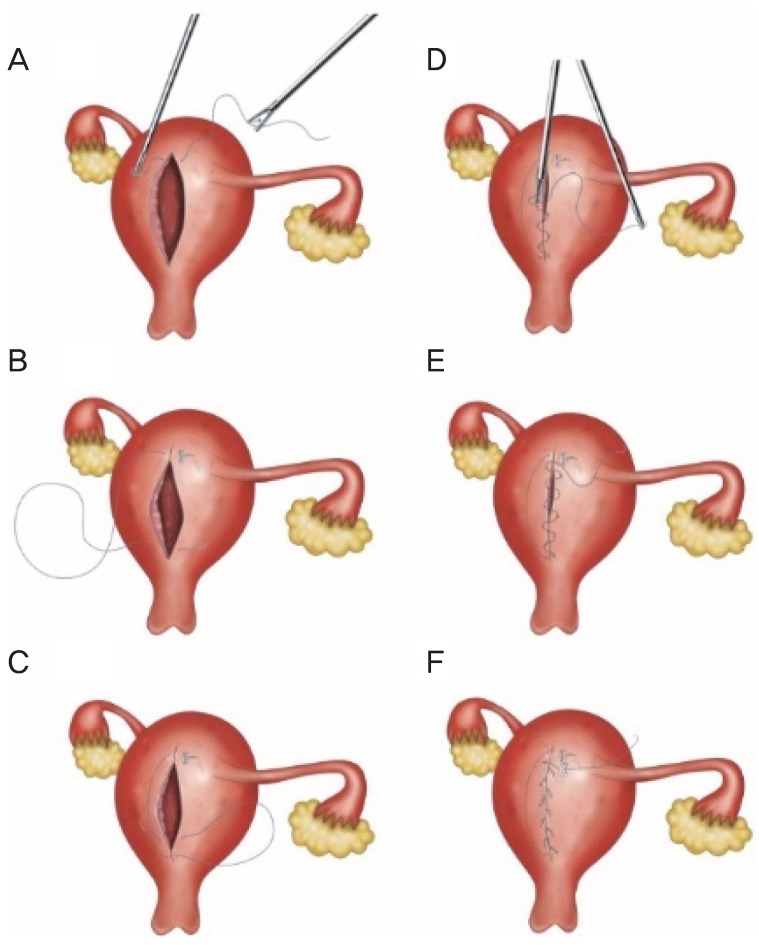
14. Choi CH, Kim TH, Kim SH, Choi JK, Park JY, Yoon A, et al. Surgical outcomes of a new approach to laparoscopic myomectomy: single-port and modified suture technique. J Minim Invasive Gynecol. 2014; 21:580–585. PMID:
24384072.

15. Kotani Y, Tobiume T, Fujishima R, Shigeta M, Takaya H, Nakai H, et al. Recurrence of uterine myoma after myomectomy: open myomectomy versus laparoscopic myomectomy. J Obstet Gynaecol Res. 2018; 44:298–302. PMID:
29227004.

16. Yoo EH, Lee PI, Huh CY, Kim DH, Lee BS, Lee JK, et al. Predictors of leiomyoma recurrence after laparoscopic myomectomy. J Minim Invasive Gynecol. 2007; 14:690–697. PMID:
17980328.

17. Bujold E, Bujold C, Hamilton EF, Harel F, Gauthier RJ. The impact of a single-layer or double-layer closure on uterine rupture. Am J Obstet Gynecol. 2002; 186:1326–1330. PMID:
12066117.

18. Song T, Kim TJ, Lee SH, Kim TH, Kim WY. Laparoendoscopic single-site myomectomy compared with conventional laparoscopic myomectomy: a multicenter, randomized, controlled trial. Fertil Steril. 2015; 104:1325–1331. PMID:
26263079.

19. Yuk JS, Ji HY, Kim KH, Lee JH. Single-port laparoscopically assisted-transumbilical ultraminilaparotomic myomectomy (SPLA-TUM) versus single port laparoscopic myomectomy: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2015; 188:83–87. PMID:
25796058.

20. Lee SW, Park EK, Lee SJ, Lee KH. Comparison study of consecutive 100 cases of single port vs. multiport laparoscopic myomectomy; technical point of view. J Obstet Gynaecol. 2017; 37:616–621. PMID:
28393585.

21. Doridot V, Dubuisson JB, Chapron C, Fauconnier A, Babaki-Fard K. Recurrence of leiomyomata after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2001; 8:495–500. PMID:
11677326.

22. Radosa MP, Owsianowski Z, Mothes A, Weisheit A, Vorwergk J, Asskaryar FA, et al. Long-term risk of fibroid recurrence after laparoscopic myomectomy. Eur J Obstet Gynecol Reprod Biol. 2014; 180:35–39. PMID:
25016181.

23. Greaves N, Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011; 93:437–440. PMID:
21929912.

24. Lee YY, Kim TJ, Kim CJ, Kang H, Choi CH, Lee JW, et al. Single-port access laparoscopic-assisted vaginal hysterectomy: a novel method with a wound retractor and a glove. J Minim Invasive Gynecol. 2009; 16:450–453. PMID:
19487164.

25. Kim YW, Park BJ, Ro DY, Kim TE. Single-port laparoscopic myomectomy using a new single-port transumbilical morcellation system: initial clinical study. J Minim Invasive Gynecol. 2010; 17:587–592. PMID:
20576473.

26. Rossetti A, Sizzi O, Chiarotti F, Florio G. Developments in techniques for laparoscopic myomectomy. JSLS. 2007; 11:34–40. PMID:
17651554.
27. Greenberg JA, Goldman RH. Barbed suture: a review of the technology and clinical uses in obstetrics and gynecology. Rev Obstet Gynecol. 2013; 6:107–115. PMID:
24920976.
28. Greenberg JA, Einarsson JI. The use of bidirectional barbed suture in laparoscopic myomectomy and total laparoscopic hysterectomy. J Minim Invasive Gynecol. 2008; 15:621–623. PMID:
18619922.

29. Ates M, Dirican A, Ince V, Ara C, Isik B, Yilmaz S. Comparison of intracorporeal knot-tying suture (polyglactin) and titanium endoclips in laparoscopic appendiceal stump closure: a prospective randomized study. Surg Laparosc Endosc Percutan Tech. 2012; 22:226–231. PMID:
22678318.
30. Delibegović S. The use of a single Hem-o-lok clip in securing the base of the appendix during laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2012; 22:85–87. PMID:
22145605.

31. Hanssen A, Plotnikov S, Dubois R. Laparoscopic appendectomy using a polymeric clip to close the appendicular stump. JSLS. 2007; 11:59–62. PMID:
17651557.
32. Janczak D, Merenda M, Litarski A, Wieraszko A, Rać J. Use of polymeric clips in laparoscopic appendectomy. Polim Med. 2011; 41:19–23. PMID:
22046823.
33. Izaki H, Fukumori T, Takahashi M, Nakatsuji H, Oka N, Taue R, et al. Clinical research of renal vein control using Hem-o-lok clips in laparoscopic nephrectomy. Int J Urol. 2006; 13:1147–1149. PMID:
16903952.

34. Kapoor R, Singh KJ, Suri A, Dubey D, Mandhani A, Srivastava A, et al. Hem-o-lok clips for vascular control during laparoscopic ablative nephrectomy: a single-center experience. J Endourol. 2006; 20:202–204. PMID:
16548730.

35. Ponsky L, Cherullo E, Moinzadeh A, Desai M, Kaouk J, Haber GP, et al. The Hem-o-lok clip is safe for laparoscopic nephrectomy: a multi-institutional review. Urology. 2008; 71:593–596. PMID:
18295866.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download