This article has been
cited by other articles in ScienceCentral.
Abstract
Drug-induced vasculitis is an inflammation of small-sized blood vessel caused by the use of drugs. It accounts for approximately 10% of acute cutaneous vasculitis. Propylthiouracil, hydralazine, and allopurinol have been widely known as causative agents. The most common clinical feature of drug-induced vasculitis is palpable purpura on lower extremities. A 66-year-old Korean female presented with erythematous nodules on upper chest and back. She had been on medication for multiple myeloma. Laboratory results showed neutropenia. After a single injection of filgrastim (recombinant granulocyte colony-stimulating factor), she developed cutaneous lesions with concurrent increase in absolute neutrophil count. A skin biopsy revealed leukocytoclastic vasculitis. After discontinuation of filgrastim injection, her skin lesions disappeared spontaneously.
Go to :

Keywords: Cutaneous, Cutaneous small vessel, Granulocyte colonystimulating factor, Skin, Vasculitis
INTRODUCTION
Granulocyte colony-stimulating factor (G-CSF) is a hematopoietic growth factor with many applications in cancer therapy. Various cutaneous adverse events associated with G-CSF have been reported, including Sweet's syndrome and pyoderma gangrenosum
1,
2. Herein, we present a case of G-CSF induced cutaneous vasculitis with unusual manifestation in a patient with multiple myeloma.
Go to :

CASE REPORT
A 66-year-old Korean female presented with erythematous nodules and plaques on upper chest and back. She had been treated with bortezomib (proteasome inhibitor) for multiple myeloma for the past three months. Laboratory investigations showed white blood cell (WBC) count of 2,710/µl and absolute neutrophil count (ANC) of 560/mm
3. Due to neutropenia, she had received 300 µg of filgrastim two weeks before her visit to our outpatient clinic. Three days after the injection, her laboratory results showed improvement in WBC and ANC count to 8,190/µl and 5,320/mm
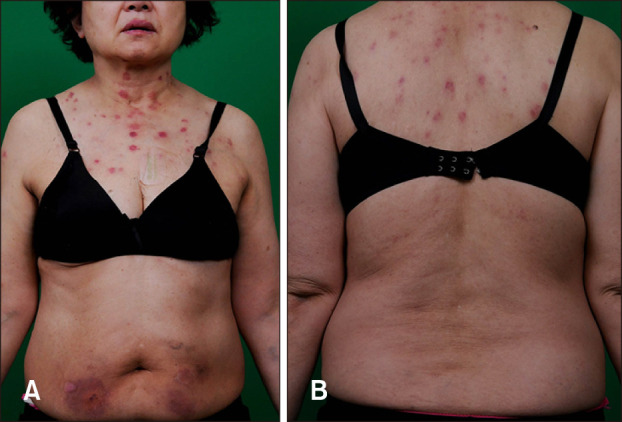
3 respectively; however, skin lesions started to develop. Multiple, tender, finger-tip to coin-sized red nodules were observed on her upper chest and back (
Fig. 1).
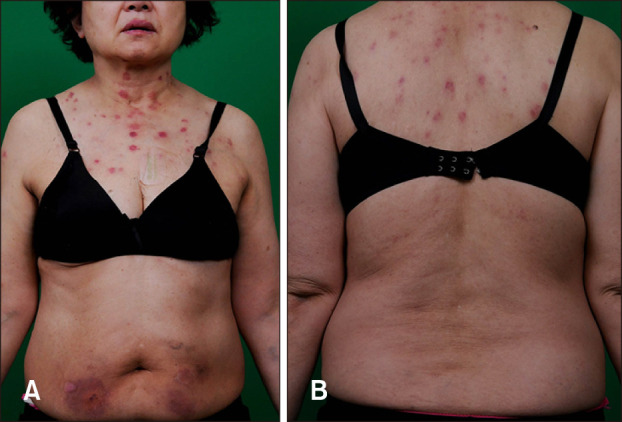 | Fig. 1Multiple tender finger-tip to coin sized red colored nodules on her upper chest (A) and back (B). We received the patient's consent form about publishing all photographic materials.
|
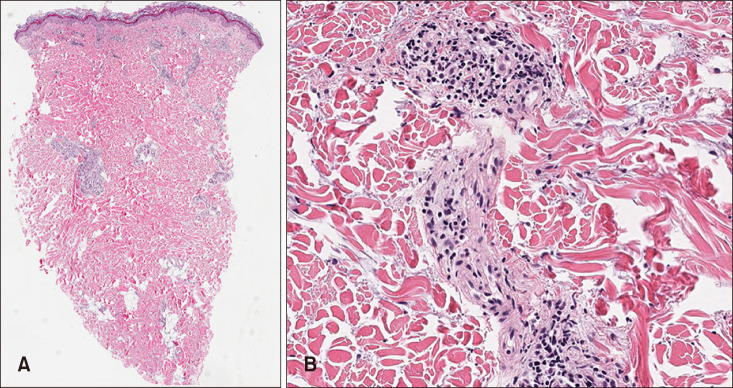
Skin biopsy on her back lesion showed vessel destruction, fibrinoid necrosis, and infiltration of neutrophils and lymphocytes with leukocytoclasia around small-sized vessels in the upper dermis, suggestive of leukocytoclastic vasculitis (
Fig. 2). After discontinuation of both bortezomib and filgrastim, the skin lesions subsided within two weeks.
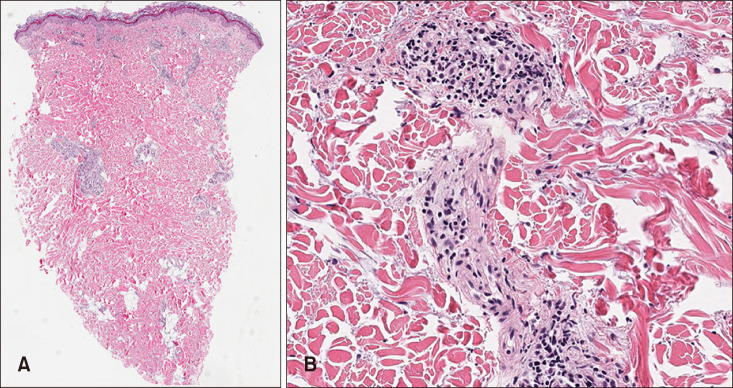 | Fig. 2Histopathological images of skin biopsy. (A) Perivascular inflammatory cells infiltration in the upper dermis (H&E, ×40). (B) Vessel destruction, fibrinoid necrosis, and neutrophils and lymphocytes infiltration (H&E, ×400).
|
Go to :

DISCUSSION
G-CSF regulates the production of neutrophils within the bone marrow. Recombinant G-CSF (filgrastim) is clinically used for the treatment of neutropenia associated with chemotherapy. Reported adverse events include bone pain, splenomegaly, hepatomegaly, thrombocytopenia, osteopenia/osteoporosis, glomerulonephritis, growth and development, and subfertility
3. Cutaneous manifestations associated with recombinant human G-CSF include Sweet's syndrome and bullous pyoderma ganrenosum
1,
2.
The biopsy result and the fact that our patient developed the skin lesion after the injection of G-CSF raised the possibility of drug-induced leukocytoclastic vasculitis. However, because this histologic findings of vasculitis can also occur as a secondary phenomenon, it was necessary for us to exclude other possibilities.
Sweet's syndrome is one of the most possible causes of neutrophilic dermatoses in cutaneous vascular diseases. Histologic findings include perivascular infiltration of neutrophils in the papillary dermis and various extent of vascular damage can be seen. Histologically, Sweet's syndrome was not favored because prominent edema of upper dermis, one of the characteristic features of Sweet's syndrome, was not seen on our specimen. Moreover, our patient did not have fever or involvement of noncutaneous sites, such as eyes, joints, oral mucosa, and visceral organs. Together with the histologic findings and clinical manifestations, we were able to diagnose our patient's skin lesions as leukocytoclastic vasculitis.
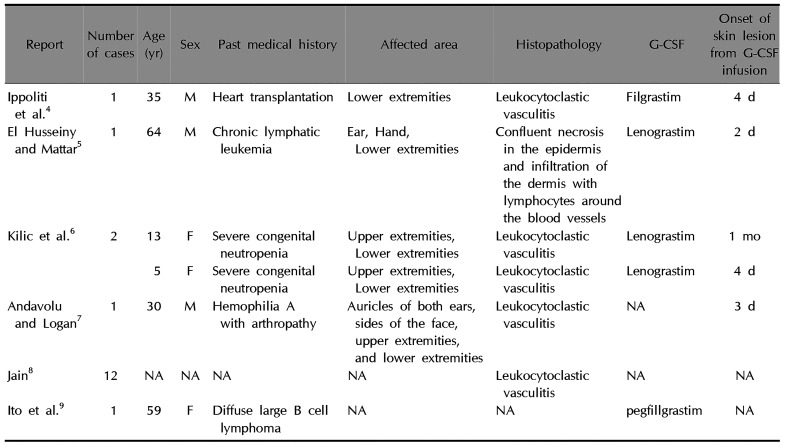
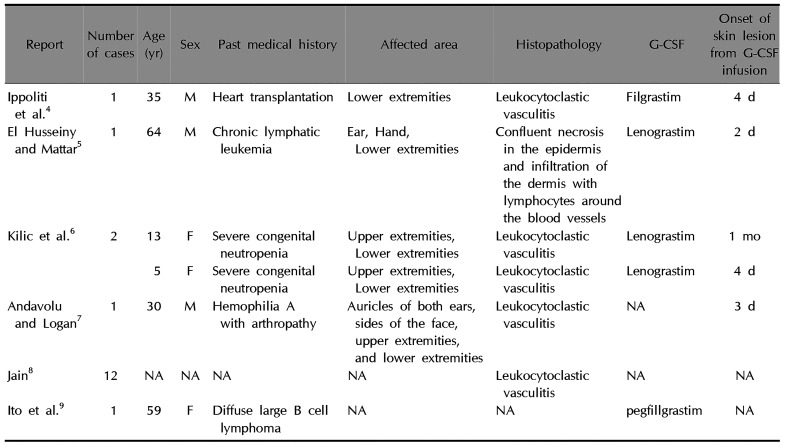
PubMed search of literature was made to retrieve publications about cutaneous vasculitis in association with infusion of G-CSF. G-CSF, cutaneous, adverse events, and vasculitis were terms used for the search. We found 18 cases of vasculitis after infusion of G-CSF. However, one study of 12 patients gave limited information (
Table 1)
4,
5,
6,
7,
8,
9. Skin lesions developed within two days to one month after receiving G-CSF. Skin biopsy was performed for 17 cases. Of them, 16 cases showed leukocytoclastic vasculitis while the other case showed vasculitis with dermal infiltration of lymphocytes around blood vessel. Affected areas of the skin were described in five cases. All cases involved lower extremities. Three cases affected upper extremities while two cases showed acral lesion concurrently. Similar to the previous case reports described above, skin lesions in the current case developed three days after the injection of G-CSF. In our case, they subsided after stopping the drug. Although drug-induced vasculitis with palpable purpura usually developed on lower extremities in other literatures, tender multiple erythematous nodules showed up on the chest and upper back of our patient.
Table 1
Summary of G-CSF induced vasculitis reported previously in literature
|
Report |
Number of cases |
Age (yr) |
Sex |
Past medical history |
Affected area |
Histopathology |
G-CSF |
Onset of skin lesion from G-CSF infusion |
|
Ippoliti et al.4
|
1 |
35 |
M |
Heart transplantation |
Lower extremities |
Leukocytoclastic vasculitis |
Filgrastim |
4 d |
|
El Husseiny and Mattar5
|
1 |
64 |
M |
Chronic lymphatic leukemia |
Ear, Hand, Lower extremities |
Confluent necrosis in the epidermis and infiltration of the dermis with lymphocytes around the blood vessels |
Lenograstim |
2 d |
|
Kilic et al.6
|
2 |
13 |
F |
Severe congenital neutropenia |
Upper extremities, Lower extremities |
Leukocytoclastic vasculitis |
Lenograstim |
1 mo |
|
5 |
F |
Severe congenital neutropenia |
Upper extremities, Lower extremities |
Leukocytoclastic vasculitis |
Lenograstim |
4 d |
|
Andavolu and Logan7
|
1 |
30 |
M |
Hemophilia A with arthropathy |
Auricles of both ears, sides of the face, upper extremities, and lower extremities |
Leukocytoclastic vasculitis |
NA |
3 d |
|
Jain8
|
12 |
NA |
NA |
NA |
NA |
Leukocytoclastic vasculitis |
NA |
NA |
|
Ito et al.9
|
1 |
59 |
F |
Diffuse large B cell lymphoma |
NA |
NA |
pegfillgrastim |
NA |

The mechanism of G-CSF-induced vasculitis is currently unclear, although some possible hypotheses have been proposed. Elsner et al.
10 who studied neutrophils in patients with congenital neutropenia suggested the involvement of altered fragment constant (FCr) receptor expression in the pathogenesis of G-CSF-induced vasculitis. Their data showed that patterns of FCr receptor expression of neutrophils from patients with severe congenital neutropenia on G-CSF therapy were signs of
in vivo activation of these cells. Because interaction between FCr receptors and immune complexes can cause release of lysosomal enzymes, altered FCr receptor expression might be associated with cutaneous vasculitis. Elsner et al.
10 demonstrated that interleukin 1α and tumor necrosis factor-α could stimulate smooth muscle cells of blood vessel walls to synthesize G-CSF by enhancing antibody-mediated toxicity of polymorphonuclear cell.
Cutaneous leukocytoclastic vasculitis is a rare adverse reaction of G-CSF treatment. Because drug-induced vasculitis is indistinguishable clinically from other causes of small vessel vasculitis, it is easy to be misdiagnosed. Patients might be treated improperly, especially when clinical presentation is unusual as described in the present case
11,
12. When the association between G-CSF and leukocytoclastic vasculitis is recognized, the drug should be immediately withdrawn. The eruption may resolve completely without the need of any further treatment. In severe cases, high-dose prednisone treatment may be required
11.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download