Abstract
SAPHO syndrome is a rare disease comprising of synovitis, acne, pustulosis, hyperostosis, and osteitis and osteoarticular manifestations usually involve anterior chest wall, spine, or pelvis. Among these features, hyperostosis of long bone was rarely reported on the upper extremity. The present case is about a 49-year-old male with painful hyperostosis of his ulna, diagnosed with SAPHO syndrome. The diagnostic process and the progress after two years are described.
Figures and Tables
Fig. 1
Antero-posterior and lateral wrist radiographs show remained metal material. Three years after metal removal, the forearm radiographs show diffuse thickening and sclerosis of midshaft of the right ulna. Cortical thickening and sclerotic lesion of the ulna was enlarged two years after the bone biopsy.

Fig. 2
Axial T1- and fat-suppressed T2-weighted show diffuse cortical thickening and intramedullary sclerosis of midshaft of the right ulna without cortical nidus, bone marrow edema, periosteal reaction, lytic soft tissue lesion, or multiplicity. Technetium 99m-methyl diphosphonate bone scan shows intense uptake in bilateral sternoclavicular joints (bull's head sign) and right ulna.
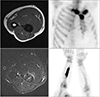
Fig. 3
The specimen composed of dense, compact bone and broad sclerotic trabeculae of mature bone containing rare inflammatory cells (H&E stain, ×40).
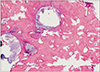
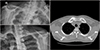
Fig. 4
Multiple deep-seated vesicles were shown on both palms and soles. Onycholysis of both fingernails was found.

ACKNOWLEDGEMENTS
This study was supported by a 2019 research grant from Pusan National University Yangsan Hospital.
The written informed consent for the patient's photograpies was obtained.
References
1. Takigawa T, Tanaka M, Nakanishi K, et al. SAPHO syndrome associated spondylitis. Eur Spine J. 2008; 17:1391–1397.

3. Zemann W, Pau M, Feichtinger M, Ferra-Matschy B, Kaercher H. SAPHO syndrome with affection of the mandible: diagnosis, treatment, and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 111:190–195.

4. Okuno H, Watanuki M, Kuwahara Y, et al. Clinical features and radiological findings of 67 patients with SAPHO syndrome. Mod Rheumatol. 2018; 28:703–708.

5. Reith JD, Bauer TW, Schils JP. Osseous manifestations of SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome. Am J Surg Pathol. 1996; 20:1368–1377.

6. Benhamou CL, Chamot AM, Kahn MF. Synovitis-acnepustulosis hyperostosis-osteomyelitis syndrome (SAPHO). A new syndrome among the spondyloarthropathies? Clin Exp Rheumatol. 1988; 6:109–112.
7. Ferguson PJ, Sandu M. Current understanding of the pathogenesis and management of chronic recurrent multifocal osteomyelitis. Curr Rheumatol Rep. 2012; 14:130–141.

8. Firinu D, Garcia-Larsen V, Manconi PE, Del Giacco SR. SAPHO syndrome: current developments and approaches to clinical treatment. Curr Rheumatol Rep. 2016; 18:35.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download