Abstract
Purpose
Extensor tendon complications associated with dorsal screw penetration following volar plating of distal radius fracture have been reported widely. The aim of this study was to find the anatomical index to predict the appropriate length of screw.
Methods
Three-dimensional computed tomography (CT) scans of distal radius were performed after removal of volar plate. According to the extensor compartments and Lister tubercle, we divided the distal radius into four groups in axial view in CT. Through sagittal view, we measured volar cortex to dorsal cortex in parallel with the extension of screw trace and anatomical index (lunate depth, anterior-posterior diameter of radius shaft). Statistical analysis was performed with ANOVA and linear regression analysis.
Results
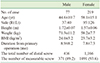
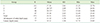
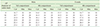
The measurable traces of screw were 371 in males and 1,091 in females. The average value was 17.59 mm, 20.72 mm, 20.31 mm, and 19.1 mm in each group for males, and 15.75 mm, 18.76 mm, 18.04 mm, and 17.22 mm for female patients. The anterior-posterior diameter of radius in which the screw was inserted to oblong hole moderately correlated with the extension of screw trace in the third and fourth compartments.
Figures and Tables
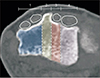 | Fig. 1The dorsal cortex of distal radius was divided into four groups by the extensor compartment and Lister's tubercle (1: second extensor compartment, 2: Lister's tubercle, 3: third extensor compartment, 4: fourth extensor compartment, A: extensor carpi radialis longus, B: extensor carpi radialis brevis, C: extensor pollics longus, D: extensor digitorum communis). |
 | Fig. 2The hole after removal of distal screws in three-dimensional reconstructed image defining dorsal cortical screw penetration. |
 | Fig. 3The length between volar cortex and dorsal cortex, which is the extension of screw traces of distal screw in sagittal image, were defined as the appropriate length of screw. |
 | Fig. 4The anatomical index for predicting appropriate length of screw. (A) The anteroposterior diameter of in shaft of radius at level of oblong hole. (B) The lunate depth in sagittal image. |
References
1. Smith DW, Henry MH. Volar fixed-angle plating of the distal radius. J Am Acad Orthop Surg. 2005; 13:28–36.

2. Al-Rashid M, Theivendran K, Craigen MA. Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg Br. 2006; 88:1610–1612.

3. De Maeseneer M, Marcelis S, Osteaux M, Jager T, Machiels F, Van Roy P. Sonography of a rupture of the tendon of the extensor pollicis longus muscle: initial clinical experience and correlation with findings at cadaveric dissection. AJR Am J Roentgenol. 2005; 184:175–179.

4. Kambouroglou GK, Axelrod TS. Complications of the AO/ASIF titanium distal radius plate system (pi plate) in internal fixation of the distal radius: a brief report. J Hand Surg Am. 1998; 23:737–741.
5. Bentohami A, de Burlet K, de Korte N, van den Bekerom MP, Goslings JC, Schep NW. Complications following volar locking plate fixation for distal radial fractures: a systematic review. J Hand Surg Eur Vol. 2014; 39:745–754.

6. Benson EC, DeCarvalho A, Mikola EA, Veitch JM, Moneim MS. Two potential causes of EPL rupture after distal radius volar plate fixation. Clin Orthop Relat Res. 2006; 451:218–222.

7. Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007; 21:316–322.

8. Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011; 93:2146–2153.

9. Brunner A, Siebert C, Stieger C, Kastius A, Link BC, Babst R. The dorsal tangential X-ray view to determine dorsal screw penetration during volar plating of distal radius fractures. J Hand Surg Am. 2015; 40:27–33.
10. Ozer K, Toker S. Dorsal tangential view of the wrist to detect screw penetration to the dorsal cortex of the distal radius after volar fixed-angle plating. Hand (N Y). 2011; 6:190–193.

11. Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am. 2012; 37:963–967.

12. Pichler W, Windisch G, Schaffler G, Rienmüller R, Grechenig W. Computer tomography aided 3D analysis of the distal dorsal radius surface and the effects on volar plate osteosynthesis. J Hand Surg Eur Vol. 2009; 34:598–602.

13. Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of lister's tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg Am. 2008; 33:1716–1719.

14. Ljungquist KL, Agnew SP, Huang JI. Predicting a safe screw length for volar plate fixation of distal radius fractures: lunate depth as a marker for distal radius depth. J Hand Surg Am. 2015; 40:940–944.

15. Beharrie AW, Beredjiklian PK, Bozentka DJ. Functional outcomes after open reduction and internal fixation for treatment of displaced distal radius fractures in patients over 60 years of age. J Orthop Trauma. 2004; 18:680–686.

16. Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function. A prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000; 82:340–344.
17. Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003; 27:1–6.

18. Berglund LM, Messer TM. Complications of volar plate fixation for managing distal radius fractures. J Am Acad Orthop Surg. 2009; 17:369–377.

19. Failla JM, Koniuch MP, Moed BR. Extensor pollicis longus rupture at the tip of a prominent fixation screw: report of three cases. J Hand Surg Am. 1993; 18:648–651.

20. Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am. 2006; 31:359–365.

21. Wall LB, Brodt MD, Silva MJ, Boyer MI, Calfee RP. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg Am. 2012; 37:446–453.

22. Baumbach SF, Synek A, Traxler H, Mutschler W, Pahr D, Chevalier Y. The influence of distal screw length on the primary stability of volar plate osteosynthesis--a biomechanical study. J Orthop Surg Res. 2015; 10:139.

23. Gasse N, Lepage D, Pem R, et al. Anatomical and radiological study applied to distal radius surgery. Surg Radiol Anat. 2011; 33:485–490.

24. Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y). 2007; 2:144–150.

25. Hill BW, Shakir I, Cannada LK. Dorsal screw penetration with the use of volar plating of distal radius fractures: how can you best detect? J Orthop Trauma. 2015; 29:e408–e413.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download