Abstract
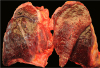
Sepsis-related deaths are occasionally encountered in forensic practice. However, forensic pathologists are reluctant to use the terminology “sepsis” or “septic shock” as a cause of death because of the lack of definite morphological evidence. When sepsis is considered a cause of death, pathologic assessment is essential to identify the foci of infection or consequences of sepsis, such as diffuse alveolar damage (DAD). Pneumonia is known to be a common source of sepsis and can develop into DAD with progression of sepsis. The histology of DAD varies according to the immunologic status. An autopsy of a 55-year-old man who died of septic shock with leukopenia revealed only abundant gram-negative bacilli in the alveoli without typical DAD pathology.
Figures and Tables
Acknowledgments
This work was supported by clinical research grant in 2018 from Pusan National University Hospital.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:801–810.


3. Morris JA, Harrison LM, Partridge SM. Postmortem bacteriology: a re-evaluation. J Clin Pathol. 2006; 59:1–9.



4. Laufe MD, Simon RH, Flint A, et al. Adult respiratory distress syndrome in neutropenic patients. Am J Med. 1986; 80:1022–1026.


5. Altaf E, Mitchel EK, Berry C, et al. Death due to pulmonary alveolar proteinosis. Am J Forensic Med Pathol. 2017; 38:11–13.


6. Warny M, Helby J, Nordestgaard BG, et al. Lymphopenia and risk of infection and infection-related death in 98,344 individuals from a prospective Danish population-based study. PLoS Med. 2018; 15:e1002685.

7. Schiel X, Hebart H, Kern WV, et al. Sepsis in neutropenia: guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol. 2003; 82 Suppl 2:S158–S166.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download