1. de Santis TO, Motta LJ, Biasotto-Gonzalez DA, Mesquita-Ferrari RA, Fernandes KP, de Godoy CH, et al. Accuracy study of the main screening tools for temporomandibular disorder in children and adolescents. J Bodyw Mov Ther. 2014; 18:87–91. PMID:
24411155.

2. Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e26–e50.

3. Goldstein BH. Temporomandibular disorders: a review of current understanding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:379–385. PMID:
10519741.

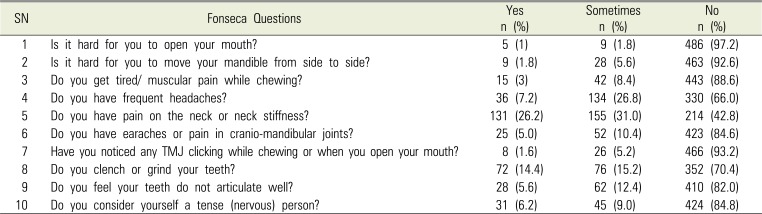
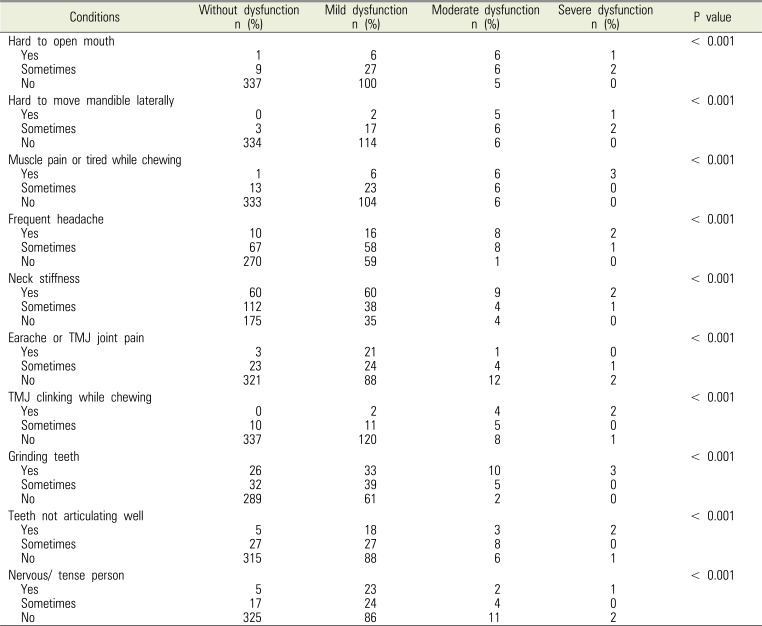
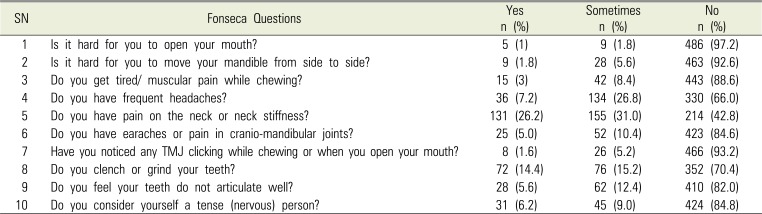
4. Da Fonseca DM, Bonfante G, Valle AL, de Freitas SFT. Diagnóstico pela anamnese da disfunção craniomandibular. Rev Gauch de Odontol. 1994; 4:23–32.
5. Bonjardim LR, Gavião MB, Pereira LJ, Castelo PM. Anxiety and depression in adolescents and their relationship with signs and symptoms of temporomandibular disorders. Int J Prosthodont. 2005; 18:347–352. PMID:
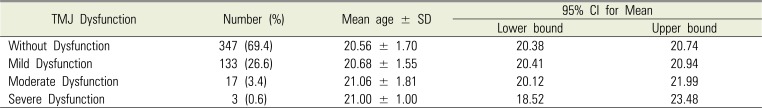
16052791.
6. Pesqueira AA, Zuim PR, Monteiro DR, Ribeiro Pdo P, Garcia AR. Relationship between psychological factors and symptoms of TMD in university undergraduate students. Acta Odontol Latinoam. 2010; 23:182–187. PMID:
21638957.
7. Habib SR, Al Rifaiy MQ, Awan KH, Alsaif A, Alshalan A, Altokais Y. Prevalence and severity of temporomandibular disorders among university students in Riyadh. Saudi Dent J. 2015; 27:125–130. PMID:
26236125.

8. Wahid A, Mian FI, Razzaq A, Bokhari SAH, Kaukab T, Iftikhar A, et al. Prevalence and severity of temporomandibular disorder (TMD) in undergraduate medical students using Fonseca's questionnaire. Pakistan Oral Dent J. 2014; 31:38–41.
9. Modi P, Shaikh SS, Munde A. A cross sectional study of prevalence of temporomandibular disorders in university students. Int J Sci Res Publ. 2012; 2:1–3.
10. Nomura K, Vitti M, Oliveira AS, Chaves TC, Semprini M, Siéssere S, et al. Use of the Fonseca's questionnaire to assess the prevalence and severity of temporomandibular disorders in Brazilian dental undergraduate. Braz Dent J. 2007; 18:163–167. PMID:
17982559.
11. Conti PC, Ferreira PM, Pegoraro LF, Conti JV, Salvador MC. A cross sectional study of prevalence and etiology of signs and symptoms of temporomandibular disorders in high school and university students. J Orofac Pain. 1996; 10:254–262. PMID:
9161230.
12. Shiau YY, Chang C. An epidemiological study of temporomandibular disorders in university students of Taiwan. Community Dent Oral Epidemiol. 1992; 20:43–47. PMID:
1547612.

13. Becker IM. Occlusion as a causative factor in TMD. Scientific basis to occlusal therapy. N Y State Dent J. 1995; 61:54–57.
14. Joo SJ, Kang DW, Lee HS, Jin SY, Lee GJ. Re-restoration of temporomandibular joint disorder acquired after implant prosthetic restoration using T-Scan: a case report. J Korean Acad Prosthodont. 2016; 54:431–437.

15. Park KS, Lee CH, Lee JW. Use of a botulinum toxin A in dentistry and oral and maxillofacial surgery. J Dent Anesth Pain Med. 2016; 16:151–157. PMID:
28884147.

16. Chi SI, Kim HJ, Seo KS, Lee JH, Chang J. Local anesthesia of the temporomandibular joint to reduce pain during mouth opening for dental treatment in a patient with spinal muscular atrophy. J Dent Anesth Pain Med. 2016; 16:137–140. PMID:
28879307.

17. Ebrahimi M, Dashti H, Mehrabkhani M, Arghavani M, Daneshvar-Mozafari A. Temporomandibular disorders and related factors in a group of Iranian adolescents: A cross-sectional survey. J Dent Res Dent Clin Dent Prospects. 2011; 5:123–127. PMID:
22991620.