Abstract
Pain control by means of local anesthesia is an intrinsic part of clinical practice in dentistry. Several studies evaluated intraligamental anesthesia using a computer-controlled anesthetic device in children. There is a need to provide a clinical guide for the use of computerized intraligamental anesthesia in children. Intraligamental anesthesia using a computer-controlled anesthetic device was found to cause significantly lower pain perception scores and lower pain-related behavior than traditional techniques. This device proven to be effective in restorative and pulp treatment in children; however, its effectiveness in primary teeth extraction is controversial. It is important to withdraw recommendations necessity of future studies concerning the side effects of computerized intraligamental anesthesia in children. The present study aims to review different clinical aspects of computerized intraligamental anesthesia in children along with the side-effects, type of local anesthesia and postoperative pain of this technique. This study provides dentists with a clinical guide for the use of computerized intraligamental anesthesia.
In dentistry, administering local anesthesia through the use of traditional syringe can cause pain and anxiety, which can also affect patient behavior. Fear and anxiety associated with local anesthesia injections can be a major impediment to dental care because they frequently cause patients to delay or even avoid treatment. For many years, a technique called intraligamental anesthesia (ILA) or periodontal ligament (PDL) injection (intraligamentary) has also been employed, primarily as a means of achieving complete anesthesia in a tooth wherein regional block anesthesia has previously failed to provide it. The technique was introduced by Fischer [1] using a standard dental syringe, wherein the dentist inserts the needle through the gingival sulcus, into the periodontal ligament, between the tooth and the alveolar bone. The needle is then directed along the long axis of the tooth as apically as possible. The operator slowly injects a small volume of anesthetic solution under pressure to control the pain in the associated tooth [2].
Recently, a Computer Controlled Anesthetic Device (CCLAD) has been introduced, in which the anesthetic solution is diffused to the tissue at a controlled rate. ILA using a CCLAD was able to diffuse around 1.2 ml per tooth through the slow rate of the machine [3]. Several studies have been conducted on the use of the CCLAD in upper molars [45678910]; however, limited studies have investigated ILA using a CCLAD as a method for single-tooth anesthesia [1112131415]. ILA, if delivered using a high-pressure syringe, can result in trauma to the periodontal tissue and prolonged postoperative pain that can last up to 4 weeks [1617]. In addition, developmental disturbances to the underlying permanent tooth buds are a potential risk of ILA in primary dentition. Therefore, the present review focuses on the studies that have evaluated ILA with the CCLAD in children, and it also aims to provide a clinical guide for ILA using the CCLAD in children. This study also presents unpublished data about pain-related behavior assessment of ILA with the CCLAD among 30 children who participated in a previous randomized clinical trial.
In the late 1970s, two new local anesthetic devices, the Peri-Press (Universal Dental Implements, P.O. Box 254, Fanwood, N. J.) and the Ligmajecti (I.M.A. Associates, U.S., Inc. 270 South Harvard Blvd., Los Angeles, Calif.), were introduced in the United States. The two devices claimed to enable the administrator to achieve profound pulpal anesthesia in a single mandibular tooth without the need for regional nerve block and without anesthetizing the lower lip and the tongue [18]. The PDL injection appeared to be a successful alternative to conventional nerve block techniques for mandibular anesthesia; however, several patients experienced slight discomfort several hours later, which was the only area of difficulty in achieving pain control using the pulp treatment [1819].
In 1997, a new concept of drug delivery through a CCLAD system known as The Wand (Milestone Scientific, Livingston, NJ) and later rebranded as CompuDent was introduced to the dental profession. The Wand consists of a disposable hand piece component and computer control unit. The anesthetic cartridge is placed in a disposable plastic sleeve that couples with the system. The anesthetic cartridge is linked with tubing to the hand piece, which is an ultra-light pen-like handle with an attached needle. The device is operated by a foot control that delivers local anesthesia with a precise volume and pressure ratio [20].
In 2006, a second device, Single Tooth Anesthesia System (STA System) (Single Tooth Anesthesia System, Milestone Scientific, Inc., Livingston, NJ), was combined with Dynamic Pressure Sensing (DPS) technology, and it was specifically engineered for dental applications [3]. The STA System also has further advantages compared with older devices, such as the ability to detect a loss of pressure from leakage during the injection and to limit the maximum pressure used. Moreover, the device is the only CCLAD to provide real-time DPS technology, enabling clinicians to perform a predictable and highly successful single-tooth anesthesia technique [3]. Additionally, the STA includes a training mode that verbally explains how to use the device, and multi-cartridge and auto-cartridge retraction features, unlike the earlier version [21].
Intraligamentary injections are typically performed using a 30-gauge or 27-gauge half-inch luer-lock needle. The drive unit operates in STA speed mode and, as the needle is introduced through the tissue, the system provides continuous audible and visual feedback to the clinician. The system has a visual pressure-sensing scale composed of a series of light-emitting diode (LED) lights (orange, yellow, and green). Hochman [3] stated that "the orange lights indicate minimal pressure, the yellow indicates mild to moderate pressure, and the green indicate moderate pressure indicative of the PDL tissue." Additionally, the auditory feedback comprises a series of sounds composed of ascending tones to guide the clinician [3].
Authors have conducted randomized trials [1113] evaluating pain perception and the effectiveness of ILA with CCLAD in children. A clinical guide for clinicians with some clinical photos showing the use of ILA in children follows:
1. ILA is carried out using a computer-regulated device with the STA System and the STA speed mode (0.005 mL/sec) selected. Fig. 1 shows the STA System.
2. A 30-gauge extra-short needle (0.5 inch) is inserted into the sulcus parallel to the long axis of the tooth with the bevel facing the tooth.
3. As the needle enters the sulcus (approximately 2 mm below the crest of the bone), the foot switch is activated at a slow rate and maintained at that rate throughout the injection process.
4. The technique described by the manufacturer [3] for each tooth recommends 2 insertion sites to be used. In children, 2% lidocaine hydrochloride containing a vasoconstrictor concentration of 1:100,000 parts is commonly used. In anterior teeth, a drug volume of 0.9 mL is recommended for single-rooted teeth. For multi-rooted teeth, pulpal anesthesia is provided by the administration of 1.2 mL of the drug (0.6 mL mesiolingual and 0.6 mL distolingual). It is recommended to always start on the distal side and then proceed to the mesial surface [14]. Fig. 2 and Fig. 3 show the technique of administration of ILA with CCLAD in primary molars.
5. If anesthetizing a mandibular tooth, you should shorten the device hand piece by pulling the micro-tubing out of the hand-piece channel, turning the tubing away, and snapping off the plastic hand piece to a length of about 1.5 inches. For better access, the needle can also be slightly bent toward the bevel, if necessary.
6. The technique for advancing the needle is to approach the tooth at about a 45° angle to the vertical plane, and place the needle in the gingival sulcus, with the bevel towards the tooth lingually.
7. It is then recommended to move the needle down the root of the tooth until there is resistance.
8. To signal the correct injection site, hold the needle in place without excessive pressure and wait for the sound and light prompts. When the light prompt arrives at the middle of the Yellow Zone, there is a good chance that the needle is in the correct site; if the light prompt arrives at the Green Zone, there is an excellent chance that the needle has reached the correct injection site.
Depending on the local anesthetic solution selected, the injection can take 1 to 2 minutes to administer for a single-rooted tooth, and 1 to 3 minutes for a molar [3]. The DPS in the STA machine allows you to know when you have arrived at the correct site (the periodontal ligament space) for a successful ILA; it also indicates if you have left the site and if the needle has been blocked by obstruction or pressure.
The literature review surrounding the use of the CCLAD has revealed that studies conducted to evaluate the CCLAD (The Wand) system in pediatric dentistry have shown variable results, imposing much controversy regarding its use in pediatric dentistry. Therefore, further investigations are required to provide scientific evidence on the use of CCLAD in children.
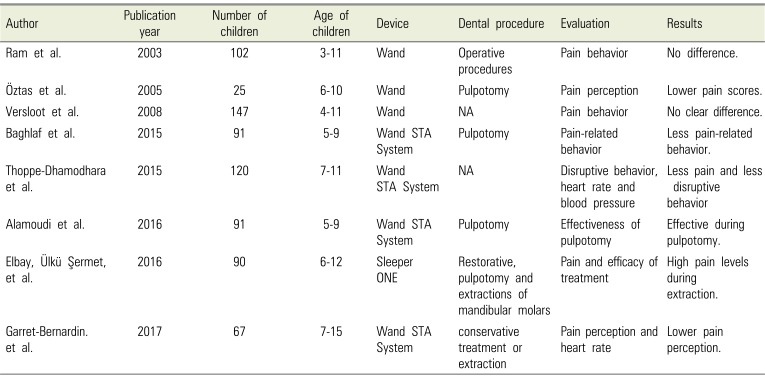
An increasing number of clinical trials have demonstrated measurable benefits of the ILA with CCLAD technology, mainly related to less pain behavior among children. Clinical trials have investigated the pain behavior of ILA with CCLAD in children; table 1 presents the findings of the studies. Five studies previously used the STA System, and all of them show lower levels of pain using ILA with CCLAD. ILA studies have shown that ILA with CCLAD results in a lesser increase in heart rate and blood pressure in comparison to the traditional technique [2223]. The effectiveness of ILA in different clinical procedures in children has resulted in with controversial outcomes. Studies have revealed that ILA with CCLAD is effective in pulpotomy and restorative procedures in children compared with an inferior alveolar nerve block (IANB) [12131423]. Researchers have explained that the presence of the DPS in the STA System makes the ILA more reliable with predictable and comfortable anesthesia. Recently, a randomized, controlled, crossover, blind clinical trial compared the effectiveness of ILA with a CCLAD in primary teeth extraction to that of supraperiosteal (SP) anesthesia with CCLAD in children [13]. It was also found in the studies that SP is more effective than ILA when used during extraction procedures. However, Garret-Bernardin et al. (2017) found that ILA using the STA System resulted in significantly lower pain ratings and a lower increase in heart rate than traditional anesthesia [23]. Nevertheless, the study did not evaluate the effectiveness of ILA in extraction.
Studies have shown that ILA using CCLAD has been effective for anesthetizing primary teeth [8121523]. ILA, if delivered by a high-pressure syringe, can result in trauma to the periodontal tissue and prolonged postoperative pain that can last up to 4 weeks [1617]. Furthermore, developmental disturbances to the underlying permanent tooth buds is another implication of ILA in primary dentition. A study previously examined the spread of the solutions injected in to the PDL and has shown no concerns with a slowly delivered injection using a special syringe [24]. According to the study by Ashkenazi in 2010 on the effect of computerized delivery ILA in primary molars on their corresponding permanent tooth buds, the CCLAD intraligamental injection does not increase the risk for any developmental disturbances to the underlying tooth buds [25].
The type of local anesthesia solution might have some influence on the effectiveness of ILA using a CCLAD. A study by Nusstein et al. (2004) compared the pain of injection, the increase in heart rate, and post-injection pain associated with intraligamentary injection of 4% articaine with 1:100,000 epinephrine and 2% lidocaine with 1: 100,000 epinephrine using a CCLAD system. The study showed similar results for the intraligamentary injection of 4% articaine with 1:100,000 epinephrine compared to 2% lidocaine with 1: 100,000 epinephrine for injection pain and post-injection pain in the mandibular first molar when administered with a CCLAD system [26]. Furthermore, for both anesthetic solutions using CCLAD, the heart rate did not significantly increase with the intraligamentary injection system. A meta-analysis of seven studies was conducted by Shabazfar et al. (2013) on periodontal intraligamental injection as an alternative to inferior alveolar nerve block; the results showed that cardiovascular disturbances were significantly more often associated with IANB, whereas ILA showed less pain during injection [27].
Hochman stated that the use of 2% local anesthesia containing a vasoconstrictor concentration of 1:50,000 parts is not recommended for administration of an intraligamentary injection. It is not also recommended to use 4% local anesthetics containing a vasoconstrictor concentration of 1:100,000 parts for administration of an intraligamentary injection [3].
A study by Baghlaf et al, (2016) showed more post-operative pain associated with ILA than with other techniques; however, this difference was not statistically significant [11]. It is known that ILA is applied under high pressure, which is responsible for the postoperative pain, but with the use of the STA System, slow-tomoderate pressures are used and the computer-controlled rate of flow during administration decreases postoperative discomfort [3]. In the study of ÖZTAS et al, (2005) no comparison was made between the postoperative pain associated with ILA and IANB; however, most patients stated that they preferred ILA to IANB.
Unpublished data from the previous clinical trial [11] describe the assessment of pain-related behavior during ILA with CCLAD using the established behavior code [28] in comparison to other traditional techniques (IANB). Pain-related behavior was recorded as present or absent for every 15-s interval of the entire injection period. The time of ILA injection (180 seconds) was longer than the IANB (90 seconds). At the first 15-second interval, the pain-related behavior of IANB was significantly higher (mean 1.40) (P-value=0.000) than ILA using CCLAD [11].
Fig. 4 illustrates the changes in the means of pain-related behavior scores [11] during ILA among 30 children. During the 180 seconds, an evaluation of pain-related behavior during the first 90 seconds correlates with the first injection on the distal side and then the second 90 seconds corresponds with the mesial injection. In the first 15 seconds, the mean of the pain-related behavior was at 0.45 (SD; 0.72), then the reaction decreased until the 105-second interval, which coincides with the second insertion of the needle (mesial) 0.33 (SD; 0.47). The pain-related behavior then decreased again to no pain reaction in the last 60 seconds, which indicated that pain-related behavior from ILA was higher only at the two insertions. However, this level is still considered less painful than that associated with the IANB technique.
This review has provided an objective assessment of ILA using CCLAD in children. There are limited studies investigating the long-term effects of ILA using CCLAD on the underlying developing tooth buds. Future studies should consider evaluation of the prevalence of developmental disturbances in permanent teeth in which buds have been exposed to ILA administrated by CCLAD. Further research could investigate the effectiveness of the ILA using different anesthetic solutions, with different dental procedures including extractions, and with different child behaviors.
Studies that have used CCLAD in administration of intraligamental anesthesia have shown lower pain perception scores and lower pain-related behavior. The effectiveness of intraligamental anesthesia using CCLAD has been proven for pulp treatment and restorative procedures in primary teeth; however, future studies need to consider evaluation of the effectiveness of CCLAD in extractions of primary molars. Longitudinal follow up studies are needed to assess the long-term effects of ILA using CCLAD on the underlying developing tooth buds.
ACKNOWLEDGEMENT
The authors are grateful to the Department of Pediatric Dentistry and the faculty of dentistry for their constant support and encouragement.
References
1. Fischer G, Riethmueller RH. Local Anesthesia in Dentistry. Lea & Febiger;1912.
2. Blanton PL, Jeske AH. Dental local anesthetics: alternative delivery methods. J Am Dent Assoc. 2003; 134:228–234. PMID: 12636129.
3. Hochman MN. Single-tooth anesthesia: pressure-sensing technology provides innovative advancement in the field of dental local anesthesia. Compend Contin Educ Dent. 2007; 28:186–188. 190192–193. PMID: 17487044.
4. Amoudi NA, Feda M, Sharaf A, Hanno A, Farsi N. Assessment of the anesthetic effectiveness of anterior and middle superior alveolar injection using a computerized device versus traditional technique in children. J Clin Pediatr Dent. 2008; 33:97–102. PMID: 19358373.

5. Feda M, Al Amoudi N, Sharaf A, Hanno A, Farsi N, Masoud I, et al. A comparative study of children's pain reactions and perceptions to AMSA injection using CCLAD versus traditional injections. J Clin Pediatr Dent. 2010; 34:217–222. PMID: 20578658.

6. Mittal M, Kumar A, Srivastava D, Sharma P, Sharma S. Pain perception: computerized versus traditional local anesthesia in pediatric patients. J Clin Pediatr Dent. 2015; 39:470–474. PMID: 26551372.

7. Versloot J, Veerkamp J, Hoogstraten J. Pain behaviour and distress in children during two sequential dental visits comparing a computerised anaesthesia delivery system and a traditional syringe. Br Dent J. 2008; 205:E2. PMID: 18493254.

8. Ram D, Peretz B. The assessment of pain sensation during local anesthesia using a computerized local anesthesia (Wand) and a conventional syringe. J Dent Child (Chic). 2003; 70:130–133. PMID: 14528773.
9. Klein U, Hunzeker C, Hutfless S, Galloway A. Quality of anesthesia for the maxillary primary anterior segment in pediatric patients: Comparison of the P-ASA nerve block using compumed delivery system vs traditional supraperiosteal injections. J Dent Child. 2005; 72:119–125.
10. Kandiah P, Tahmassebi JF. Comparing the onset of maxillary infiltration local anaesthesia and pain experience using the conventional technique vs. the Wand in children. Br Dent J. 2012; 213:E15. PMID: 23138830.

11. Baghlaf K, Alamoudi N, Elashiry E, Farsi N, El Derwi DA, Abdullah AM. The pain-related behavior and pain perception associated with computerized anesthesia in pulpotomies of mandibular primary molars: A randomized controlled trial. Quintessence Int. 2015; 46:799–806. PMID: 26287025.
12. Alamoudi NM, Baghlaf KK, Elashiry EA, Farsi NM, El Derwi DA, Bayoumi AM. The effectiveness of computerized anesthesia in primary mandibular molar pulpotomy: A randomized controlled trial. Quintessence Int. 2016; 47:217–224. PMID: 26504907.
13. Elbay ÜŞ, Elbay M, Kaya E, Cilasun Ü. Intraligamentary and supraperiosteal anesthesia efficacy using a computer controlled delivery system in mandibular molars. J Clin Pediatr Dent. 2016; 40:193–199. PMID: 27472565.

14. Öztaş N, Ulusu T, Bodur H, Doğan C. The Wand in pulp therapy: an alternative to inferior alveolar nerve block. Quintessence Int. 2005; 36:559–564. PMID: 15997937.
15. Ram D, Kassirer J. Assessment of a palatal approachanterior superior alveolar (P-ASA) nerve block with the Wand® in paediatric dental patients. Int J Paediatr Dent. 2006; 16:348–351. PMID: 16879332.
16. Kim S. Ligamental injection: A physiological explantation of its efficacy. J Endod. 1986; 12:486–491. PMID: 3465854.

17. Kaufman E, Weinstein P, Milgrom P. Difficulties in achieving local anesthesia. J Am Dent Assoc. 1984; 108:205–208. PMID: 6584494.

18. Malamed SF. The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol. 1982; 53:117–121. PMID: 6949113.

19. Davidson L, Craig S. The use of the periodontal ligament injection in children. J Dent. 1987; 15:204–208. PMID: 3479463.

20. Krochak M, Friedman N. Using a precision-metered injection system to minimize dental injection anxiety. Compend Contin Educ Dent. 1998; 19:137–140. 142–143. 146PMID: 9656861.
21. Saxena P, Gupta SK, Newaskar V, Chandra A. Advances in dental local anesthesia techniques and devices: An update. Natl J Maxillofac Surg. 2013; 4:19–24. PMID: 24163548.

22. Thoppe-Dhamodhara YK, Asokan S, John BJ, Pollachi-Ramakrishnan G, Ramachandran P, Vilvanathan P. Cartridge syringe vs computer controlled local anesthetic delivery system: Pain related behaviour over two sequential visits–a randomized controlled trial. J Clin Exp Dent. 2015; 7:e513–e518. PMID: 26535099.
23. Garret-Bernardin A, Cantile T, D'Antò V, Galanakis A, Fauxpoint G, Ferrazzano GF, et al. Pain Experience and Behavior Management in Pediatric Dentistry: A Comparison between Traditional Local Anesthesia and the Wand Computerized Delivery System. Pain Res Manag. 2017; 2017:7941238. PMID: 28293129.

24. Brännström M, Nordenvall K, Hedström K. Periodontal tissue changes after intraligamentary anesthesia. ASDC J Dent Child. 1982; 49:417. PMID: 6960028.
25. Ashkenazi M, Blumer S, Eli I. Effect of computerized delivery intraligamental injection in primary molars on their corresponding permanent tooth buds. Int J Paediatr Dent. 2010; 20:270–275. PMID: 20536588.

26. Nusstein JM, Reader A, Drum M. Local anesthesia strategies for the patient with a “hot” tooth. Dent Clin. 2010; 54:237–247.

27. Shabazfar N, Daubländer M, Al-Nawas B, Kämmerer P. Periodontal intraligament injection as alternative to inferior alveolar nerve block—meta-analysis of the literature from 1979 to 2012. Clin Oral Investig. 2014; 18:351–358.

28. Allard G, Stokes T. Continuous observation: a detailed record of children's behavior during dental treatment. ASDC J Dent Child. 1980; 47:246. PMID: 6938534.
Fig. 1
Single Tooth Anesthesia System (STA-System) and the extra-short needle used in administration of intraligamental anesthesia.
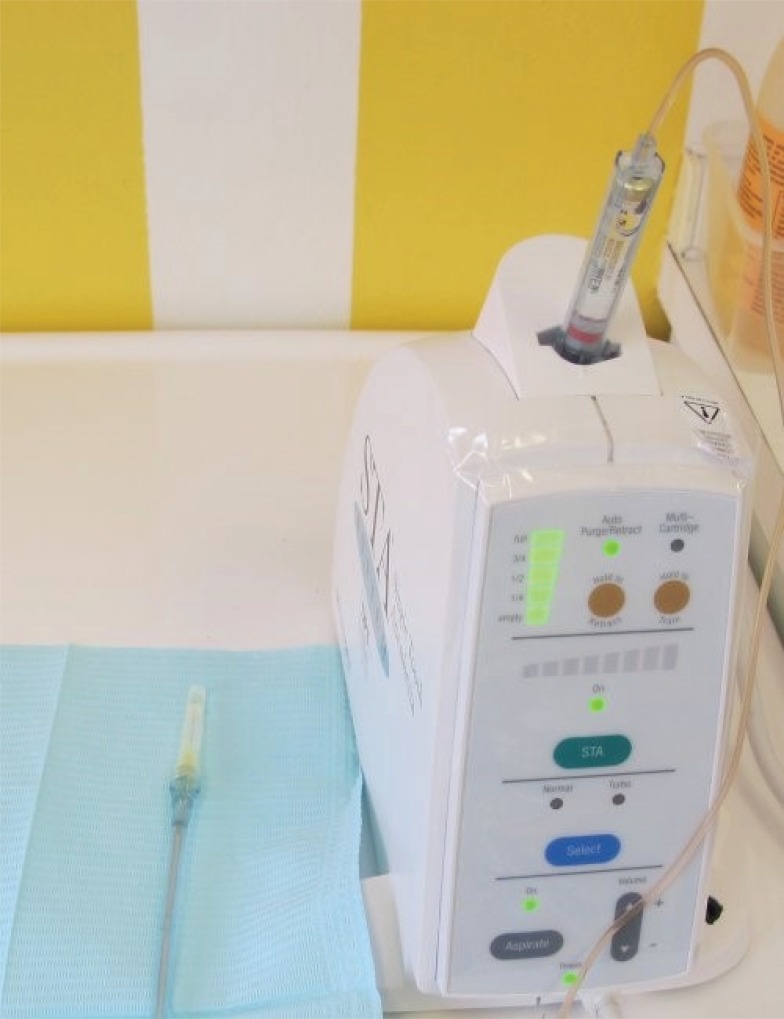
Fig. 2
Administration of intraligamental anesthesia in a multi-rooted teeth. The image presents the first insertion on the distolingual side of the tooth.

Fig. 3
Administration of intraligamental anesthesia in a multi-rooted teeth. The image shows the second insertion on the mesiolingual side of the tooth.

Fig. 4
Mean pain-related behavior during different intervals of intraligamental anesthesia administration using CCLAD (n = 30 children; age range: 5–9 years).
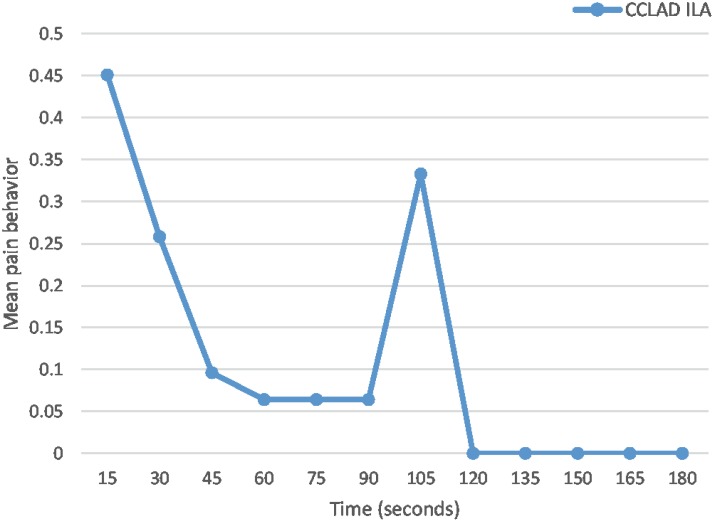
Table 1
Studies that have investigated intraligamental anesthesia using the computer-controlled anesthetic device in children




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download