This article has been
cited by other articles in ScienceCentral.
Abstract
Background
This study aimed to evaluate the anti-inflammatory efficacy of preemptive intravenous ibuprofen on inflammatory complications such as edema and trismus in patients undergoing impacted mandibular third molar surgery.
Methods
Sixty patients were included and divided into three groups (800 mg IV ibuprofen + 50 mg dexketoprofen, 800 mg IV ibuprofen, and control). In all patients, preoperative hemodynamic values were recorded before the infusions. The operation was started at 15-min post-infusion. Evaluation of edema size on the face and mouth opening (trismus) was conducted in the preoperative period, and at postoperative 48 h and 1 week.
Results
No difference was determined among the groups in trismus and edema size in postoperative measurements (P > 0.05). There was a difference between group 2 and group 3 only in measurement value of tragus-corner of the mouth on the postoperative day 2 (P < 0.05). A difference was found between the measurement values of trismus preoperatively and at preoperative day 2, and between postoperative day 2 and 1 week in group 3 based on time (P < 0.05). In group 3, edema on the face on postoperative day 2 increased significantly compared to that in the preoperative period (P < 0.001); in addition, edema increased significantly in groups 1 and 2 in the postoperative period but was less than that in group 3 (P < 0.001).
Conclusions
In this study, intravenous ibuprofen was determined to be more effective alone or in combination in alleviating trismus and to better limit the postoperative edema.
Go to :

Keywords: Edema, Postoperative, Preemptive Intravenous Ibuprofen, Third Molar, Tooth Extraction, Trismus
INTRODUCTION
Tooth extraction is indicated for prophylactic and therapeutic purpose in patients with problems caused by impacted teeth. Therefore, the impacted third molar surgery is one of the most common procedures in oral surgery [
1]. Inflammatory response of tissue caused by trauma can cause complications such as pain, edema, and trismus after impacted tooth surgery in patients [
234]. Postoperative edema reaches the highest level between 12–48 h after surgery and its complete alleviation takes 5–7 d. Currently, the most important objective is to increase the patient's comfort by minimizing all complications in the postoperative period [
5].
In order to prevent postoperative edema, medical treatment options and various supportive treatments such as cold application, enzymes, drainage, and low-level laser therapies can be used [
678].
Natural metabolites of arachidonic acid, such as prostaglandins and leukotrienes, play an important role in the inflammatory process by causing vascular dilation, increasing capillary permeability, and increasing the spread of hyperalgesia and migration of leukocytes and macrophages to the inflammatory region. Non-steroidal anti-inflammatory drugs such as ibuprofen inhibit cyclooxygenase, decreasing production of prostaglandins; and thus, pain, trismus and edema are controlled [
9]. This study aimed to evaluate the anti-inflammatory efficacy of preemptive intravenous ibuprofen on inflammatory complications such as edema and trismus developing after the impacted mandibular third molar surgery. Primary objective was to investigate the effect of preemptive intravenous ibuprofen on edema in the postoperative period; and secondary objective was to investigate the effect of preemptive intravenous ibuprofen on trismus in the postoperative period.
Go to :

METHODS
This randomized controlled study was conducted for a duration of three months in Erzincan University Hospital. The Erzincan University ethics committee approved the study (no: 6/03) and written informed consent was obtained from all patients. Sixty patients, aged between 20–35 years, undergoing elective extraction of the third molar tooth and whose third molar tooth was located angularly or horizontally and was symptomatic, were included in the study. The study was registered at ClinicalTrials.gov (ID: NCT03170713).
Patients who did not agree to participate in the study, were younger than 20 years and older than 35 years, had known allergies to nonsteroidal anti-inflammatory drugs, were pregnant, had severe liver failure and/or severe renal failure were excluded from the study.
The patients were divided randomly into three groups during the preoperative period. Randomization was done by MedCalc 11.5 (MedCalc Software bvba, Ostend, Belgium) using the one packet program and permutation method.
Group 1 (800 mg IV ibuprofen + dexketoprofen): 800 mg ibuprofen and 50 mg dexketoprofen were preoperatively administered for 30 min in 150 cc normal saline; and in the postoperative period, dexketoprofen + methylprednisolone (40 mg) + sultamicillin tosylate infusion was administered in 150 cc normal saline.
Group 2 (800 mg IV ibuprofen): 800 mg ibuprofen was preoperatively administered for 30 min in 150 cc normal saline. In the postoperative period, dexketoprofen + methylprednisolone (40 mg) + sultamicillin tosylate infusion was administered in 150 cc normal saline.
Group 3 (control group): 150 cc normal saline was preoperatively administered for 30 min. In the postoperative period, dexketoprofen + methylprednisolone (40 mg) + sultamicillin tosylate infusion was administered in 150 cc normal saline.
Based on previous reports that 800 mg ibuprofen can safely be used in postoperative analgesia in the form of a 30 min infusion, we used 800 mg ibuprofen in our study [
1011].
For the double-blind study, drugs to be administered to the patients were prepared by the anesthesia technician before starting the infusion, and the researchers were not aware of the medications administered to the patients. Since dexketoprofen + methylprednisolone (40 mg) + sultamicillin tosylate infusion in 150 cc normal saline was used in the postoperative period in routine practice of our hospital, it was considered as the control group. All dexketoprofen and methylprednisolone treatments were performed at 2 d postoperatively so as not to affect the study.
In all patients, edema size and mouth openings (trismus) were evaluated in the preoperative period, and postoperative period, at 48-h and 1-week postoperatively. Trismus was defined as the maximum mouth opening between the incisal edges of the upper and lower central incisors using Vernier calipers before surgery. Patients were re-examined and mouth openings were recorded at 0-min, 48-h, and 7-d post-operatively [
9].
For evaluation of edema, in the preoperative period, values obtained from patients using the extraoral band measurement method were utilized and the data were recorded on the forms. The measured points included distances between the tragus-corner of the mouth, tragus-gonion, and angulus-corner of the eye. The evaluation was repeated at 48 h and 7 d in the postoperative period [
9].
All extractions were performed by the same surgeon.
1. Statistical analysis
The power of the study was calculated by considering 10 mm as a reference based on previous study [
12]. In this study, the difference between the face edema measured in the preoperative period and postoperative day 2 was 16 mm. In contrast, in the present study, it was estimated that the difference between the face edema measured in the preoperative period and postoperative day 2 was 10 mm. Thus, the total number of patients was calculated as 60 with the power of 90% and the alpha value of 0.05.
Data obtained from the present study were analyzed using the SPSS version 22.0 program (IBM Corp., Armonk, USA). The parametric test assumptions were fulfilled; hence, Kolmogorov-Smirnov variance analysis, the Tukey test, repeated measures analysis of variance, the Bonferroni test, and the chi-square test were used; the significance level was set as 0.05.
Go to :

RESULTS
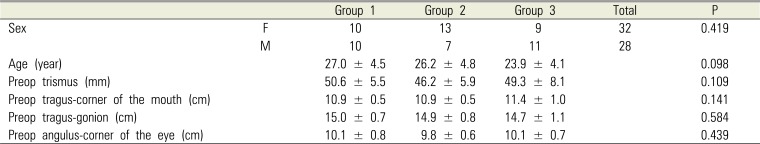
1. Demographic data
In total, 32 female patients and 28 male patients were included. There was no statistically significant difference among the groups in terms of age, sex, and preoperative measurements (P > 0.05) (
Table 1).
Table 1
Descriptive data
|
|
Group 1 |
Group 2 |
Group 3 |
Total |
P |
|
Sex |
F |
10 |
13 |
9 |
32 |
0.419 |
|
M |
10 |
7 |
11 |
28 |
|
|
Age (year) |
|
27.0 ± 4.5 |
26.2 ± 4.8 |
23.9 ± 4.1 |
|
0.098 |
|
Preop trismus (mm) |
|
50.6 ± 5.5 |
46.2 ± 5.9 |
49.3 ± 8.1 |
|
0.109 |
|
Preop tragus-corner of the mouth (cm) |
|
10.9 ± 0.5 |
10.9 ± 0.5 |
11.4 ± 1.0 |
|
0.141 |
|
Preop tragus-gonion (cm) |
|
15.0 ± 0.7 |
14.9 ± 0.8 |
14.7 ± 1.1 |
|
0.584 |
|
Preop angulus-corner of the eye (cm) |
|
10.1 ± 0.8 |
9.8 ± 0.6 |
10.1 ± 0.7 |
|
0.439 |

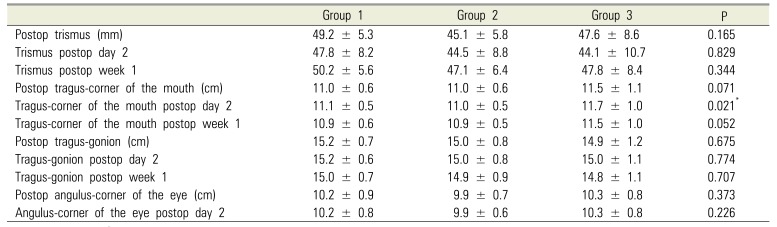
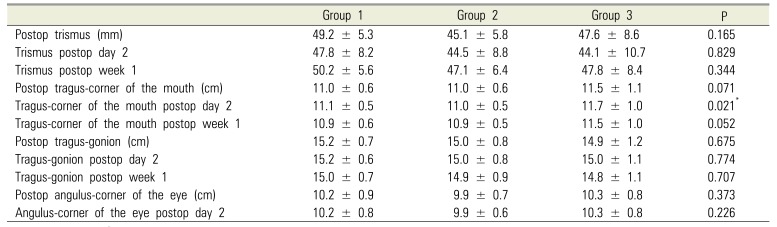
2. Postoperative measurements
Comparison of postoperative measurements among the groups indicated no significant difference in terms of trismus and edema (P > 0.05). There was a difference only between group 2 and group 3 in the measurement value of tragus-corner of the mouth on postoperative day 2 (P < 0.05) (
Table 2).
Table 2
Postoperative data
|
Group 1 |
Group 2 |
Group 3 |
P |
|
Postop trismus (mm) |
49.2 ± 5.3 |
45.1 ± 5.8 |
47.6 ± 8.6 |
0.165 |
|
Trismus postop day 2 |
47.8 ± 8.2 |
44.5 ± 8.8 |
44.1 ± 10.7 |
0.829 |
|
Trismus postop week 1 |
50.2 ± 5.6 |
47.1 ± 6.4 |
47.8 ± 8.4 |
0.344 |
|
Postop tragus-corner of the mouth (cm) |
11.0 ± 0.6 |
11.0 ± 0.6 |
11.5 ± 1.1 |
0.071 |
|
Tragus-corner of the mouth postop day 2 |
11.1 ± 0.5 |
11.0 ± 0.5 |
11.7 ± 1.0 |
0.021*
|
|
Tragus-corner of the mouth postop week 1 |
10.9 ± 0.6 |
10.9 ± 0.5 |
11.5 ± 1.0 |
0.052 |
|
Postop tragus-gonion (cm) |
15.2 ± 0.7 |
15.0 ± 0.8 |
14.9 ± 1.2 |
0.675 |
|
Tragus-gonion postop day 2 |
15.2 ± 0.6 |
15.0 ± 0.8 |
15.0 ± 1.1 |
0.774 |
|
Tragus-gonion postop week 1 |
15.0 ± 0.7 |
14.9 ± 0.9 |
14.8 ± 1.1 |
0.707 |
|
Postop angulus-corner of the eye (cm) |
10.2 ± 0.9 |
9.9 ± 0.7 |
10.3 ± 0.8 |
0.373 |
|
Angulus-corner of the eye postop day 2 |
10.2 ± 0.8 |
9.9 ± 0.6 |
10.3 ± 0 |
0.226 |

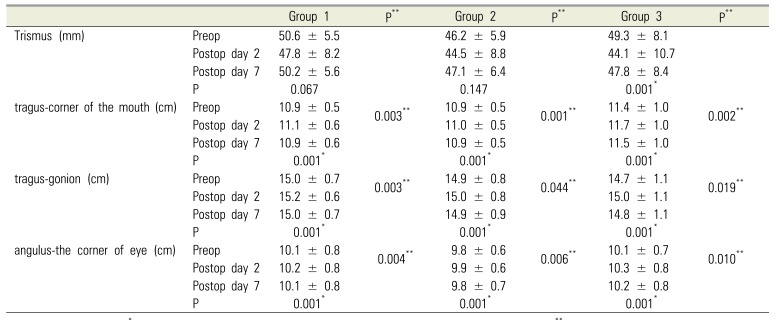
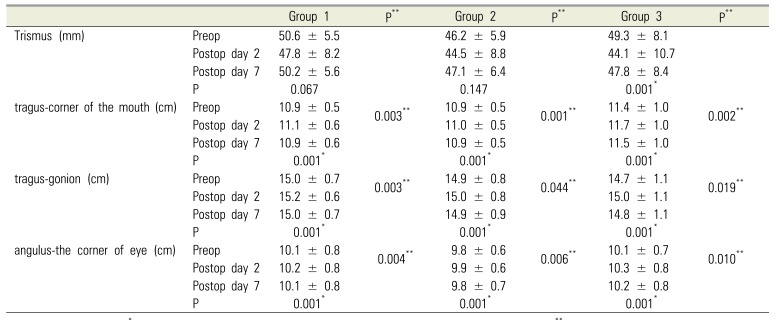
3. Within-group changes based on time
Comparison of the trismus values at different time-points revealed that the difference between the measurement values in group 3 were significant (P < 0.05). Pair-wise comparison indicated a difference between trismus during the preoperative period and on postoperative day 2, and between postoperative day 2 and 1 week (P < 0.05); however, no difference was determined between the other measurements (P > 0.05). In corroboration, in group 3, a limitation was seen in the mouth opening at postoperative day 2, whereas mouth opening at 1-week postoperatively was close to normal in value. In addition, mouth opening was limited at postoperative day 2 in groups 1 and 2, without significance, and less limitation was determined compared to the other groups (P = 0.147) (
Table 3).
Table 3
Change rates of the within-group measurements based on time
|
|
Group 1 |
P**
|
Group 2 |
P**
|
Group 3 |
P**
|
|
Trismus (mm) |
Preop |
50.6 ± 5.5 |
|
46.2 ± 5.9 |
|
49.3 ± 8.1 |
|
|
Postop day 2 |
47.8 ± 8.2 |
44.5 ± 8.8 |
44.1 ± 10.7 |
|
Postop day 7 |
50.2 ± 5.6 |
47.1 ± 6.4 |
47.8 ± 8.4 |
|
P |
0.067 |
0.147 |
0.001*
|
|
tragus-corner of the mouth (cm) |
Preop |
10.9 ± 0.5 |
0.003**
|
10.9 ± 0.5 |
0.001**
|
11.4 ± 1.0 |
0.002**
|
|
Postop day 2 |
11.1 ± 0.6 |
11.0 ± 0.5 |
11.7 ± 1.0 |
|
Postop day 7 |
10.9 ± 0.6 |
10.9 ± 0.5 |
11.5 ± 1.0 |
|
P |
0.001*
|
0.001*
|
0.001*
|
|
tragus-gonion (cm) |
Preop |
15.0 ± 0.7 |
0.003**
|
14.9 ± 0.8 |
0.044**
|
14.7 ± 1.1 |
0.019**
|
|
Postop day 2 |
15.2 ± 0.6 |
15.0 ± 0.8 |
15.0 ± 1.1 |
|
Postop day 7 |
15.0 ± 0.7 |
14.9 ± 0.9 |
14.8 ± 1.1 |
|
P |
0.001*
|
0.001*
|
0.001*
|
|
angulus-the corner of eye (cm) |
Preop |
10.1 ± 0.8 |
0.004**
|
9.8 ± 0.6 |
0.006**
|
10.1 ± 0.7 |
0.010**
|
|
Postop day 2 |
10.2 ± 0.8 |
9.9 ± 0.6 |
10.3 ± 0.8 |
|
Postop day 7 |
10.1 ± 0.8 |
9.8 ± 0.7 |
10.2 ± 0.8 |
|
P |
0.001*
|
0.001*
|
0.001*
|

The within-group changes in edema based on time revealed that edema on the face at 2 d postoperatively in all measurement areas in groups 1 and 3 were significantly increased compared to that in the preoperative period and returned to normal values at 1-week postoperatively (P < 0.001) (
Table 3). In group 2, it was determined that the edema increased significantly in the postoperative period but was less than that in the other groups (P < 0.001) (
Table 3).
Go to :

DISCUSSION
In this study investigating the effect of preemptive intravenous ibuprofen on edema and trismus in the postoperative period, it was determined that intravenous ibuprofen provided better recovery in all postoperative periods and was more effective especially on postoperative day 2.
Third molar surgery is one of the most common oral surgical procedures [
13], which causes trauma to the soft tissue and bone that directly results in acute postoperative inflammation, distinct pain, swelling, and dysfunction.
Trismus, or limited mouth opening, is another undesirable effect commonly reported after oral surgeries. Trismus prevents eating and talking and impairs the quality of life of patients; thus, decreased trismus translates to patients' reduced discomfort and increased quality of life. Osunde et al. [
14] observed that age, sex, and surgical difficulty level had no effect on the limitation of mouth opening, which was in agreement with the findings of the present study. Agarwal et al. [
12] reported that the use of ibuprofen 400 mg resulted in better relief of trismus compared to aceclofenac. Similarly, Jain et al. [
9] stated that the general recovery was better in patients treated with ibuprofen. In corroboration with the literature, it was determined in the present study that intravenous ibuprofen administered in the preoperative period was more effective either alone or in combination with steroid for alleviating trismus in patients undergoing impacted mandibular third molar surgery.
Edema on the face increases progressively in response to the tissue trauma in the third molar region and attains peak level at 48 h post-surgery [
15]. It is difficult to accurately measure face edema after surgery because it requires three-dimensional measurement of an irregular and convex surface and can manifest internally and externally. Over the years, various techniques have used in an attempt to measure the edema objectively. The measurement tools mentioned in the literature include standardized stereo radiography or photography measurements, computed tomography, linear measurement, use of Vernier calipers for measuring the cheek circumference, modified face-holding devices, ultrasonography, facial plethysmographs, or various direct face-taking methods [
12]. The comparative superiority or accuracy of any techniques used in edema analysis have not been proven. In this study, different facial markings were measured by using 3-0 silk which is an applicable, low-cost and reliable technique for evaluating swelling on the face.
Postoperative swelling or edema is the result of inflammatory exudates. Inflammation is a normal immune response that initiates the healing process. Arachidonic acid metabolites, such as prostaglandins and leukotrienes, play an important role in the inflammation process by mediating vasodilation, increased capillary permeability, and increased migration of leukocytes and macrophages to the inflammatory sites [
9]. To minimize the clinical findings of surgical injury, pharmacological strategies are designed to block the formation of mediators of acute inflammation or inhibit their effects [
15]. The concept of using NSAIDs to control post-operative pain, facial swelling, and trismus as a single agent or in combination with other agents is becoming increasingly attractive since its mechanisms are better understood [
16].
Ibuprofen is a propionic acid derivative with analgesic, anti-inflammatory, and antipyretic properties. The efficacy of ibuprofen in postoperative toothache has been well established [
1718192021]. However, while this is valid for oral ibuprofen, the effect of preemptive intravenous ibuprofen on trismus and edema has not been investigated. In the study by Agarwal et al. [
12], ibuprofen and aceclofenac were effective in controlling edema on the face. Similarly, Troullos et al. [
15] reported that ibuprofen improved the patients' recovery by limiting the edema when administered in both preoperative and postoperative periods. In the present study, the results indicated that postoperative edema increased less and was limited better in the groups receiving IV ibuprofen compared to controls. In order to demonstrate the antiinflammatory effect of ibuprofen, the combination of NSAID and steroids was administered after postoperative day 2; significant differences between the groups before administration of the drugs were attributed to the antiinflammatory effect of ibuprofen.
The present study has some limitations. First, the postoperative pain of the patients was not evaluated. The fact that pain limits the mouth opening should be taken into consideration. Second, the size of facial edema was not evaluated by means of another sophisticated method owing to feasibility issues. In this study, we sought to exploit the preemptive analgesic effect of dexketoprofen, and the antiinflammatory effect of treatment group 1 may have produced a synergistic effect with ibuprofen. Miranda et al. [
22] emphasized that dexketoprofen combined with NSAIDs produced a synergistic antinociceptive activity and that this type of combination could improve the therapeutic effect. In the same study, it was noted that there were no side effects of the components at low doses and these combinations could be used especially for long-term pain treatment.
In conclusion, preemptive intravenous ibuprofen was effective in alleviating trismus alone or in combination and limited postoperative edema in patients undergoing impacted mandibular third molar surgery. Intravenous ibuprofen administered during the preoperative period provided good recovery in all postoperative periods and was more effective on postoperative day 2.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download