Abstract
Methods
We enrolled 110 patients scheduled to undergo oral and maxillofacial surgery, requiring nasotracheal intubation. After intubation, the depth of tube insertion was measured. The neck circumference and distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch were measured. To estimate optimal tube depth, correlation and regression analyses were performed using clinical and anthropometric parameters.
Results
The mean tube depth was 28.9 ± 1.3 cm in men (n = 62), and 26.6 ± 1.5 cm in women (n = 48). Tube depth significantly correlated with height (r = 0.735, P < 0.001). Distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch correlated with depth of the endotracheal tube (r = 0.363, r = 0.362, and r = 0.546, P < 0.05). The tube depth also correlated with the sum of these distances (r = 0.646, P < 0.001). We devised the following formula for estimating tube depth: 19.856 + 0.267 × sum of the three distances (R2 = 0.432, P < 0.001).
Conclusion
The optimal tube depth for nasotracheally intubated adult patients correlated with height and sum of the distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch. The proposed equation would be a useful guide to determine optimal nasotracheal tube placement.
Nasotracheal intubation (NTI) is a common method of securing the airway in patients undergoing oral and maxillofacial surgery [1]. Appropriate positioning of the endotracheal tube (ETT) is an important aspect of airway management. Inappropriate position is hazardous; if the tip of the tube is positioned too high, accidental extubation or vocal cord trauma may occur [23]. On the other hand, if positioned too deep, endobronchial intubation may occur, leading to hypoxemia, atelectasis, or tension pneumothorax, with increased mortality [4]. Therefore, precise positioning of the tube in the trachea is crucial.
For orotracheal intubation, several methods have been proposed to estimate the optimal depth of ETT insertion [567]. Calculation of depth of insertion using physical indices such as height, weight, or estimation based on preoperative chest radiograph has been suggested [58]. Fiberoptic bronchoscopy or palpation of the cuff in sternal notch can also be used to confirm adequate placement. However, none of these methods are consistently useful. Most studies are based on anatomical indices of western adults [8], and hence, of limited value in our clinical practice. In addition, because of anatomical differences, estimates for orotracheal intubation are not applicable for nasotracheal intubation. Therefore, in the present study, we aimed to determine appropriate depth of nasal ETT placement; besides, we examined the utility of easily measurable anthropometric parameters that may guide appropriate depth of nasal ETT placement.
After obtaining approval from the Institutional Review Board of Dankook University Hospital (registered number: DKUH 2016-07-007), this study was conducted from Jul 2016 to Jul 2017. Written informed consent for inclusion in this study was obtained from patients aged between 17–80 years, with American Society of Anesthesiologists physical status 1 or 2, who were scheduled for elective oral and maxillofacial surgery requiring nasotracheal intubation.
Patients with craniofacial anomalies or any abnormalities of the upper airway such as inflammation, abscess, trauma, or tumor; and those with a previous history of difficult intubation, were excluded. Patients with a history of cervical spine and temporomandibular joint disorders, or radiotherapy for head and neck cancer were also excluded because of possible difficulty with airway management.
Anesthesia was standardized; no premedication was administered. In the operating room, patients were monitored for bispectral index, non-invasive blood pressure, peripheral oxygen saturation (SpO2), and electrocardiogram. After preoxygenation with 100% oxygen via a facemask, anesthesia was induced with propofol 2 mg/kg and fentanyl 2 µg/kg intravenously. When bispectral index was < 60 and the patient stopped responding to verbal commands, rocuronium 0.6 mg/kg was administered intravenously. After performing mask ventilation with 4 vol% sevolurane for 3–5 minutes, nasotracheal intubation was performed.
All intubations were performed by appropriately trained residents or staff of the department of anesthesiology. Ring-Adair-Elwyn (RAE) preformed nasal endotracheal tubes (PORTEX® Polar Preformed Tracheal Tube, Smith Medical International Ltd., Hythe, Kent, UK) were used, with internal diameter (ID) 7.0 mm in males and 6.5 mm in females. The initial ETT placement and positioning were confirmed on clinical assessment by cuff palpation at the sternal notch. The position of the tip of the ETT was confirmed by fiberoptic bronchoscopy and placed 3 cm above the carina. After confirming position, the depth of tube placement was measured using the centimeter markings printed on the tube. We measured the neck circumference and distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to the sternal notch. All measurements were carried out with the head in the neutral position.
Anesthesia was maintained using a target-controlled infusion of propofol and remifentanil with bispectral index between 40–60. Ventilation was carried out with a tidal volume of 8 ml/kg and respiratory rate of 10–12 breaths/minute, maintaining end-tidal carbon dioxide concentration at 35–40 mm Hg. At the end of surgery, propofol and remifentanil were discontinued, and the neuromuscular block was reversed. After extubation, patients were transferred to the post-anesthesia care unit (PACU).
All statistical analyses were performed using SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA). Data are presented as number, mean ± standard deviation (SD), or mean (min, max) as appropriate. Continuous variables were compared using the Student's t-test or Mann-Whitney U-test; categorical variables were compared using the chi-square test or Fisher's exact test. Regression and correlation analyses were performed to evaluate the impact of parameters and demographic data on the estimation of the depth of ETT placement. A p-value less than 0.05 was considered to indicate statistical significance.
We enrolled 110 patients between 18-80 years in this study. Demographic data are presented in Table 1. Males were significantly taller (171.8 ± 7.9 cm vs 157.4 ± 7.1 cm, p < 0.05) and heavier (70.4 ± 12.1 kg vs 60.2 ± 11.0 kg, p < 0.05); age, BMI and ASA status were not significantly different.
The mean distance from tip of the ETT to the nares, defined as tube depth was 28.0 ± 1.8 cm with the head in the neutral position (Table 2). Tube depth in males was 28.9 ± 1.3 cm, while that in females was 26.6 ± 1.5 cm. There was no malposition with either bronchial intubation or too proximal placement, as the tube tip was adjusted and confirmed by fiberoptic bronchoscopy in all patients. Anthropometric measurements are shown in Table 2. The distances between nares to tragus, tragus to angle of the mandible, angle of the mandible angle to sternal notch, and the sum of these distances were significantly different between males and females (P < 0.05).
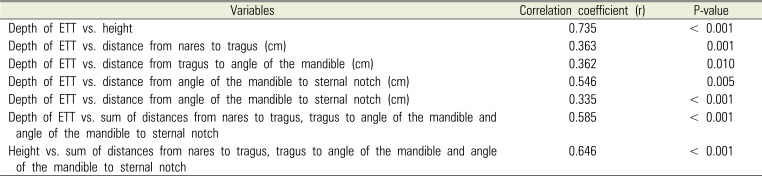
Correlations between measured data are presented in Table 3. Tube depth significantly correlated with height (r = 0.735, P < 0.001). The distances between nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch also correlated with tube depth (r = 0.363, r = 0.362, and r = 0.546, P < 0.05 respectively). In addition, tube depth correlated with the sum of these distances (r = 0.646, P < 0.001). Figure 1 shows the linear regression plot between tube depth and sum of the three distances; the estimated tube depth was 19.856 + 0.267 × sum of the three distances (R2 = 0.432, P < 0.001)
We confirmed appropriate positioning and predicted optimal tube depth of nasotracheal tubes by correlation with anthropometric measurements. We demonstrated that the sum of distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch correlated with the depth of nasal ETT placement. Based on these values, the appropriate tube depth may be estimated.
Proper positioning of the nasal ETT after intubation is crucial to safe airway management; however, optimal positioning remains a concern. Auscultation of breath sounds for detection of bronchial intubation is not always reliable [9]. Although there are several methods to confirm positioning, they may not always be feasible. Besides, a correctly positioned ETT might migrate later with change of patient position [1011], flexion or extension of the head [12], or peritoneal insufflation [1013]. This may lead to complications, such as bronchial intubation or accidental extubation. It may be difficult to ascertain tube position by clinical findings. Moreover, since radiography may not always be practicable in the operating room, an estimate of appropriate tube depth may be useful. Based on easily measured values in clinical practice, we performed regression analysis to estimate appropriate tube depth.
In the present study, the mean distance from nares to tip of ETT were 28.9 ± 1.3 cm in male patients and 26.6 ± 1.5 cm in female patients. The difference in tube depth between males and females was about 2 cm; this is consistent with previously recommended depths of 21 cm for females and 23 cm for males with orotracheal intubation [514]. According to a previous report, the mean depth of nasal ETT placement was 27.8 ± 1.5 cm in males, and 27.5 ± 1.0 cm in females [15]. In another study, tube depths were 31.3 cm in males and 29.1 cm in females [12]. Our results are different from these reports; this is probably because we estimated tube depth based on anthropometric data, which vary between races and individuals.
Furthermore, tube depth correlated with patient height and the sum of the distances between nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch (Table 3). Using our estimation, the equation that depth of nasal ETT = 19.856 + 0.267 × sum of the three values (R2 = 0.432, P < 0.001) (Fig. 1). We were able to device a formula based on the sum of the three distances to estimate optimal depth of nasal ETT placement, without the need for confirmation by chest radiography or fiberoptic bronchoscopy.
Although the correlation between tube depth and height was stronger, we estimated tube depth using the sum of anthropometric measurements. In a previous study, a significant correlation was found between the nares-vocal cord distance and height with nasotracheal intubation [16]. Our results are consistent with this study. On the other hand, according to other studies [581718], though prediction of airway length using age, height, weight, or arbitrarily determined length maybe be useful, it may not always be possible to individualize measurements [8]. Evron et al. [19] reported that positioning of endotracheal tubes may be individualized using topographic landmarks. Although patient height strongly correlated with tube depth, we estimated tube depth based on anthropometric measurements.
Tube depth did not correlate with age; we assumed that as all patients in our study were over 18 years, it was unlikely that increase in age would affect physical measurements significantly. This is consistent with a previous study that showed no correlation between height and tube depth [8].
We used nasal RAE tubes in our study. These tubes are marked at the point of the preformed curvature to help positioning [20]. Hence, RAE tubes may be an effective alternative to nasotracheal intubation in patients undergoing oral and maxillofacial surgery required. Although the preformed curvature of the RAE tube assures airway patency, the ability to adjust the intubation depth is limited. Moreover, since the length from the tip of the tube to the mark is constant, we feel it is difficult to individualize tube depth.
Our study has several limitations. First, this study was based on anthropometric measurements of, adult, Korean patients. A larger sample size would be necessary to apply it in different populations. Second, we used portex RAE nasal ETT for nasotracheal intubation in our study. This tube is made of silicone and has an opaque surface; besides, depth measurements are not marked, which may have affected the accuracy of our measurements. Third, all measurements were made with the head in neutral position. If the head position changes during surgery, the tube depth should be adjusted accordingly.
In conclusion, the optimal ETT depth of nasotracheally intubated adult patients with the head placed in neutral position is correlated with height and the sum of the distances from nares to tragus, tragus to angle of the mandible, and angle of the mandible to sternal notch. The formula we propose would be a useful guide in determining the optimal tube placement in the patients who require nasotracheal intubation.
Notes
References
1. Prasanna D, Bhat S. Nasotracheal intubation: An overview. J Maxillofac Oral Surg. 2014; 13:366–372. PMID: 26224998.

2. Sugiyama K, Yokoyama K. Displacement of the endotracheal tube caused by change of head position in pediatric anesthesia: Evaluation by fiberoptic bronchoscopy. Anesth Analg. 1996; 82:251–253. PMID: 8561322.
3. Cavo JW Jr. True vocal cord paralysis following intubation. Laryngoscope. 1985; 95:1352–1359. PMID: 4058215.

4. Zwillich CW, Pierson DJ, Creagh CE, Sutton FD, Schatz E, Petty TL. Complications of assisted ventilation. A prospective study of 354 consecutive episodes. Am J Med. 1974; 57:161–170. PMID: 4843890.
5. Owen RL, Cheney FW. Endobronchial intubation: a preventable complication. Anesthesiology. 1987; 67:255–257. PMID: 3605754.
6. Mehta S. Intubation guide marks for correct tube placement. A clinical study. Anaesthesia. 1991; 46:306–308. PMID: 2024752.

7. Patel N, Mahajan RP, Ellis FR. Estimation of the correct length of tracheal tubes in adults. Anaesthesia. 1993; 48:74–75. PMID: 8434755.

8. Eagle CC. The relationship between a person's height and appropriate endotracheal tube length. Anaesth Intensive Care. 1992; 20:156–160. PMID: 1595848.

9. Grmec S, Mally S. Prehospital determination of tracheal tube placement in severe head injury. Emerg Med J. 2004; 21:518–520. PMID: 15208251.
10. Ezri T, Hazin V, Warters D, Szmuk P, Weinbroum AA. The endotracheal tube moves more often in obese patients undergoing laparoscopy compared with open abdominal surgery. Anesth Analg. 2003; 96:278–282. PMID: 12505966.

11. Jordi Ritz EM, Von Ungern-Sternberg BS, Keller K, Frei FJ, Erb TO. The impact of head position on the cuff and tube tip position of preformed oral tracheal tubes in young children. Anaesthesia. 2008; 63:604–609. PMID: 18477271.

12. Hartrey R, Kestin IG. Movement of oral and nasal tracheal tubes as a result of changes in head and neck position. Anaesthesia. 1995; 50:682–687. PMID: 7645696.

13. Lobato EB, Paige GB, Brown MM, Bennett B, Davis JD. Pneumoperitoneum as a risk factor for endobronchial intubation during laparoscopic gynecologic surgery. Anesth Analg. 1998; 86:301–303. PMID: 9459238.

14. Roberts JR, Spadafora M, Cone DC. Proper depth placement of oral endotracheal tubes in adults prior to radiographic confirmation. Acad Emerg Med. 1995; 2:20–24. PMID: 7606606.
15. Reed DB, Clinton JE. Proper depth of placement of nasotracheal tubes in adults prior to radiographic confirmation. Acad Emerg Med. 1997; 4:1111–1114. PMID: 9408424.

16. Han DW, Shim YH, Shin CS, Lee YW, Lee JS, Ahn SW. Estimation of the length of the nares-vocal cord. Anesth Analg. 2005; 100:1533–1535. PMID: 15845720.

17. Weiss M, Gerber AC, Dullenkopf A. Appropriate placement of intubation depth marks in a new cuffed paediatric tracheal tube. Br J Anaesth. 2005; 94:80–87. PMID: 15486002.
18. Cherng CH, Wong CS, Hsu CH, Ho ST. Airway length in adults: Estimation of the optimal endotracheal tube length for orotracheal intubation. J Clin Anesth. 2002; 14:271–274. PMID: 12088810.

19. Evron S, Weisenberg M, Harow E, Khazin V, Szmuk P, Gavish D, et al. Proper insertion depth of endotracheal tubes in adults by topographic landmarks measurements. J Clin Anesth. 2007; 19:15–19. PMID: 17321921.

20. Raajesh JI, Debendra TK, Shanmugam D, Bhat RR. Modification of submental intubation using oral ring-adair-elwyn tubes in faciomaxillary surgeries: A novel approach. Indian J Anaesth. 2013; 57:418–419. PMID: 24163465.

Fig. 1
Linear regression between tube depth and the sum of the distances between nares to tragus, tragus to angle of the mandible and angle of the mandible to sternal notch. Estimated tube depth = 19.856 + 0.267 × sum of the three values. R2 = 0.432, P < 0.001.

Table 1
Demographic data
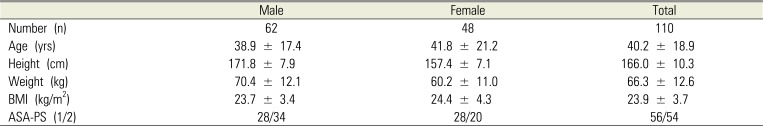
Table 2
Comparison of anthropometric parameters between male and female patients
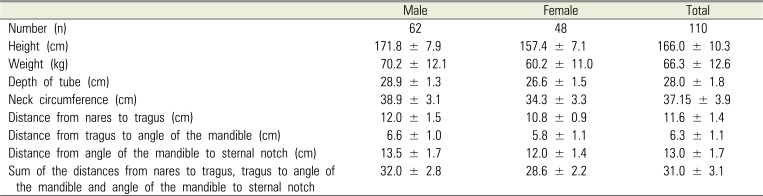
Table 3
Correlation between tube depth and measured values




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download