Abstract
Background
This study aimed to compare the pain levels during anesthesia and the efficacy of the QuickSleeper intraosseous (IO) injection system and conventional inferior alveolar nerve block (IANB) in impacted mandibular third molar surgery.
Methods
This prospective randomized clinical trial included 30 patients (16 women, 14 men) with bilateral symmetrical impacted mandibular third molars. Thirty subjects randomly received either the IO injection or conventional IANB at two successive appointments. A split-mouth design was used in which each patient underwent treatment of a tooth with one of the techniques and treatment of the homologous contralateral tooth with the other technique. The subjects received 1.8 mL of 2% articaine. Subjects' demographic data, pain levels during anesthesia induction, tooth extractions, and mouth opening on postoperative first, third, and seventh days were recorded. Pain assessment ratings were recorded using the 100-mm visual analog scale. The latency and duration of the anesthetic effect, complications, and operation duration were also analyzed in this study. The duration of anesthetic effect was considered using an electric pulp test and by probing the soft tissue with an explorer.
Results
Thirty patients aged between 18 and 47 years (mean age, 25 years) were included in this study. The IO injection was significantly less painful with lesser soft tissue numbness and quicker onset of anesthesia and lingual mucosa anesthesia with single needle penetration than conventional IANB. Moreover, 19 out of 30 patients (63%) preferred transcortical anesthesia. Mouth opening on postoperative first day was significantly better with intraosseous injection than with conventional IANB (P = 0.013).
One of the most important goals of surgery is to obtain effective anesthesia before performing various surgical interventions. The inferior alveolar nerve block (IANB) is the most common anesthetic technique used when performing various surgical interventions involving the mandible.
Previous studies regarding local anesthesia describe alternative techniques for blocking the inferior alveolar nerve such as the Gow-Gates [1] and Vazirani-Akinosi [2] anesthetic techniques or transcortical anesthesia [3]. The sharp probe test and electric pulp testers were widely used in comparative studies of anesthetic methods [14].
Intraosseous (IO) anesthesia or transcortical anesthesia is a type of anesthesia where the local anesthetic solution is deposited in the cancellous bone adjacent to the tooth to be anesthetized. The medullary bone allows fast diffusion of the anesthetic solution and immediate onset of anesthesia [5]. IO anesthesia is used specifically for endodontic treatments of teeth with acute inflammation that cannot be anesthetized using conventional techniques [36789]. Furthermore, 86%–93% of anesthetic success was reported in teeth with irreversible pulpitis [38].
Surgical removal of impacted lower third molars is widely performed in general practice. Despite well-established indications for the removal of impacted lower third molar such as recurrent pericoronitis, cyst development, unrestorable caries, or periodontal breakdown distal to the lower second molar [10], the prophylactic removal of these teeth is still universally practiced [11]. Anesthesia prior to the most common oral surgeries has been achieved with IANB, which has several complications [1213] and a high failure rate [14]. Therefore, IO injection was proposed as an alternative anesthesia technique for impacted third molar surgeries [1516]. Although IANB has a higher success rate than IO anesthesia for impacted third molar surgery [16], IO anesthesia has several advantages, such as enabling painless anesthesia with less soft tissue numbness, a shorter latent period, and lingual and palatal anesthesia with single needle penetration [15]. IO anesthesia is induced in the jaw bone using devices performing the following two actions: perforation of the bone and deposition of solution [17]. QuickSleeper (Dental Hi Tec, Cholet, France) is the most commonly used IO anesthesia device as it perforates the bone and delivers the anesthetic solution with a single penetration [15].
This study aimed to compare the pain levels during anesthesia and the efficacy of the QuickSleeper IO injection system and conventional IANB in impacted mandibular third molar surgery.
Thirty adult subjects who were treated at the University of Selçuk, Department of Oral and Maxillofacial Surgery between December 2015 and March 2016 participated in this prospective randomized clinical study. All patients were thoroughly informed about the study. All patients provided informed consent before the interventions. Blinding of the study was not possible considering that QuickSleeper is different from a conventional syringe and has a rotary component that can be felt by patients during the anesthesia phase. Therefore, the patients could discriminate the unusual anesthetic procedure. The subjects had bilaterally impacted mandibular third molars in a symmetric position without an acute infection, and all impacted third molar teeth were indicated for extraction.
Patients aged between 18 and 47 years who were healthy without systemic diseases, graduated at least from high school, and were not taking any medications (such as analgesics and anti-inflammatory drugs) that affect pain perception were included in the study. Patients with mandibular premolar teeth and molar teeth with root canal treatment, orthodontic braces fillings, crowns, and hypoplasia that could not be accurately tested using the pulp tester test and female patients on their menstrual period or who were pregnant were excluded. Menstrual cycle was a determinant risk factor in the frequency of complications such as alveolar osteitis [18]. Patients who did not cooperate with appointments were excluded from the study. Anesthetic failure was not observed in both groups. Needle tip obstruction was observed in one patient, who was subsequently excluded in the study.
After obtaining a detailed anamnesis, clinical examination and panoramic radiography were performed. The ethical committee of the University of Selçuk Faculty of Medicine and Republic of Turkey Ministry of Health Committee of Medical Devices and Drug Administration approved the study (December 17, 2015) (No. 93189304-000-47784). Each patient provided written informed consent.
Two appointments 3 weeks apart were scheduled for each of the 30 subjects. All types of anesthetic techniques, surgical procedures, and tests were performed by the same researcher. A split-mouth design was used in which each patient underwent treatment of a tooth with one of the techniques and treatment of the homologous contralateral tooth with the other technique. Groups were divided into the transcortical anesthesia group I (30 patients) and conventional anesthesia group II (30 patients). A power analysis suggested that a sample size of 30 patients provided an 86% chance of determining the efficacy of transcortical anesthesia.
All anesthetic and surgical operations were performed in the operation theaters of the Department of Oral and Maxillofacial Surgery under asepsis and antisepsis conditions by the same researcher. Patients were instructed to complete the questionnaire about pain assessment during anesthesia induction and surgery at their first appointment and pain during mouth opening at appointments on postoperative first, third, and seventh days. Maximal mouth opening was measured on the postoperative first, third, and seventh days. Before anesthesia induction, pulp tester measurements were recorded for the adjacent two molars and two premolars to compare the pulpal anesthesia duration. After isolation with cotton rolls and drying with a gauze, a toothpaste was applied to the probe tip, which was placed midway between the gingival margin on the buccal surface The current rate of the pulp tester ranged from no output (0) to the maximum output of 64. The numbers at initial sensation and during postinjection tests were recorded.
We used the QuickSleeper S4 anesthetic system (Dental Hi Tec, Cholet, France) for IO anesthesia induction (Fig. 1a). A total of 1.8 ml of 2% articaine solution with 1/100,000 epinephrine (Ultracaine® DS Forte carpule, Sanofi Aventis) was injected using a 27-gauge (0.40-mm-diameter) needle. The injection was administered in two phases. First, the alveolar mucosal soft tissue, adjacent to the determined perforation site, was anesthetized with a supraperiosteal infiltration injection of 0.3 ml of 2% articaine. Second, the direction of the needle was adjusted parallel to the sagittal plane, and after contacting the cortical bone, the rotation pedal was pushed until the needle moved in the cancellous bone with a “breakthrough” feeling. The injection pedal was pushed to deposit the remaining 1.5-ml solution (Fig. 1b). The buccal soft tissue surface was examined using a sharp explorer, and the anesthesia latent period was noted.
The standard IANB and buccal nerve anesthesia was induced using a dental injector with a 1.8 ml of 2% articaine solution with 1/100000 epinephrine (Ultracaine® DS Forte ampule, Sanofi Aventis). First, IANB was performed. The direction of the needle was adjusted from the contralateral commissura and penetrated 1 cm behind the anterior margin of the ramus and 1 cm superior to the occlusion. The needle was moved to the ipsilateral commissura following bone contact and pushed forward parallel to the ramus until the mandibular foramen was contacted. The needle was moved to the contralateral commissure and moved 2 mm and subsequently aspirated and injected. All patients were anesthetized by the same experienced researcher paying careful attention to all patients to avoid anesthetic failures or traumatic anesthesia procedure that could affect the results of the study. After the patient reported lip numbness, buccal anesthesia was induced. The latent period was reported according to lip numbness using the sharp explorer test on the operation site.
After the anesthesia was successfully induced, the surgical procedure was performed. Following the surgical extraction of the impacted mandibular third molars using a standard technique, the operation period was noted. Since pulpal anesthesia was considered, pulp tester measurements were recorded every 15 min for the two molars and premolars adjacent to the extracted third molar until the teeth responded to the highest limitation of pulp tester. The sharp explorer test was also performed every 15 min until the patient felt pain; subsequently, soft tissue anesthesia duration was considered. This test was applied to soft tissue adjacent to the extraction socket in both groups.
The data were statistically analyzed using the Statistical Package for the Social Sciences version 15.0. To compare the two anesthetic techniques, paired sample t-test was used. Correlation tests for numerical data and chi-squared tests for grouped variables were used.
Thirty (16 women and 14 men) medically healthy adult patients aged between 18 and 47 years (mean, 25; standard deviation, 2,3) participated in the study. According to age distribution, 63.3% of patients referred to our department for third molar surgery were aged between 20 and 30 years.
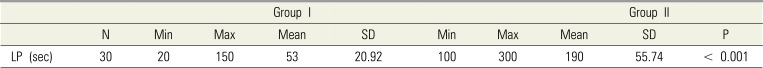
Although the duration of injection for transcortical anesthesia takes longer time than IANB, the latent period for group I was significantly shorter than that in group II (P < 0.05) (Table 1).
The pain ratings for injections and operations are presented in Table 2. The visual analog scale levels during anesthesia induction in group II were higher than those in group I, and the difference was statistically significant (P < 0.05). The mean operation durations were 11.3 min and 12.3 min in group I and Group II, respectively (P > 0.05). Patients reported pain levels that were felt during surgery. There was no statistically significant difference between the two groups in terms of pain levels during surgical procedure (P > 0.05). There was no statistically significant difference between the two groups according to postoperative pain levels on the first, third, and seventh days with maximum mouth opening (P > 0.05) (Table 2).
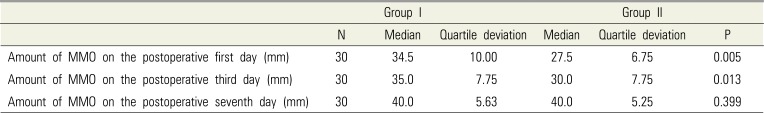
The postoperative amounts of maximum mouth opening are presented in Table 3. The first and third day postoperative amounts of maximum mouth opening were higher in group I than in group II, and the difference was statistically significant (P < 0.05). The maximum mouth opening on the seventh postoperative day did not show any difference (Table 3).
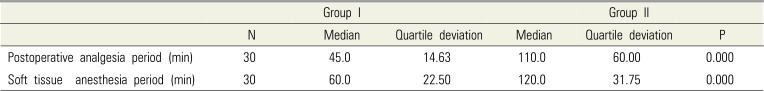
The postoperative durations of postoperative analgesia, pulpal anesthesia, and soft tissue anesthesia were considered. The duration of postoperative analgesia was shorter in group I (range, 15–120 min; mean, 45 min) than in group II (range, 35–300 min; mean, 120 min) (P < 0.05) (Table 4). The duration of postoperative soft tissue anesthesia was shorter in group I (range, 15–160 min; mean, 62.5 min) than in group II (range, 60–240 min; mean, 129 min) (P < 0.05) (Table 4). The ratings of postoperative pulpal anesthesia were statistically significantly lower in group I than in group II for two molars and two premolars on 15, 30, 45, and 60 min postoperatively (P < 0.05). On 75 and 90 min postoperatively, although there was no statistically significant difference between the ratings of pulpal anesthesia on the first molar and two premolars, pulpal anesthesia for the second molar was still significantly higher in group II than in group I.
Sex was considered if it has effect on pain perception. Female patients reported significantly higher level of pain scores during anesthesia procedure (P = 0.024) and surgical procedure (P = 0.039) than male patients.
Patients were asked which anesthesia technique they would prefer if they would have one more extraction. Nineteen out of 30 patients (63.3%) preferred transcortical anesthesia.
In this study, we applied either conventional mandibular anesthesia routinely used in the clinic or transcortical anesthesia with the QuickSleeper before the extraction of impacted mandibular third molars. We aimed to statistically determine the pain levels during surgery and anesthesia, postoperative analgesia and anesthesia durations, postoperative mouth opening and pain levels, and patient preferences.
The split-mouth technique is used by several researchers to increase standardization [131920]. Our study is designed with the same method. Therefore, both anesthetic techniques were performed in the study subjects.
Conventional IANB in third molar surgical interventions may result in lingual nerve injury [21], inferior alveolar nerve injury [22], facial paralyses [12], high failure rate (range, 15%–20%) [14], soft tissue injury in pediatric population related with deep anesthesia [13], toxicity reactions related with intravascular injection [2], and medial pterygoid trismus (myospasm) [23].
Considering the disadvantages and complications of IANB, researchers are in search of an alternative anesthesia technique for impacted molar surgery. We aim to evaluate the efficacy of IO anesthesia as an alternative to IANB.
The efficacy of IO anesthesia technique was widely investigated in painless endodontic treatment that cannot be provided with conventional anesthesia techniques [359]. Although transcortical anesthesia is considered as an effective technique for various interventions [1516], recently, investigations on the side effects of IO anesthesia are still limited. Woodmansey et al. described a case of osteonecrosis subsequent to IO anesthesia, which may be related with patient's human immunodeficiency virus infection [24]. Coggins et al. have reported a 3% incidence of postinjection exudate and 1% bruising at the IO site [25]. The IO system has several drawbacks including possible needle tip obstruction and inadequate duration of anesthetic effect [15]. A significantly lower torque of the advancing needle was further noted for the QuickSleeper system, lowering its root damaging indentation potential. Moreover, the computer-controlled QuickSleeper system uses lower syringe diameters without a potential risk of syringe breakage [26].
Horalek and Liewehr compared the IO anesthesia devices such as Stabident (Fairfax Dental, Wimbledon, UK), X-Tip (X-tip technologies, Lakewood, NJ), and Intraflow (Pro-Dex/Micro Motors, Santa Ana, CA). Perforation and injection are performed in different steps in Stabident and X-Tip devices. The Intraflow Anesthesia System enters into the penetration zone; hence, injection and withdrawal are performed as one continuous step [17]. We used QuickSleeper, where bone perforation and IO injection are performed in one step in our study.
The latencies were 7.1 ± 2.23 min and 0.48 ± 0.32 min for the conventional technique and IO anesthesia, respectively, with the difference being statistically significant [27]. Sovatdy et al. reported that IO anesthesia provides significantly faster objective onset (90.6 ± 45.21 sec) than IANB (136.00 ± 66.99 sec) [16]. In our study, the latencies were 190 ± 55.74 sec and 53 ± 20.9 sec for the conventional technique and IO anesthesia, respectively. The difference between the two groups was statistically significant.
The depth of the anesthetic effect was sufficient with both techniques; hence, patients were able to tolerate the impacted third molar surgery in our study. In a study involving 30 patients subjected to conventional anesthesia and IO anesthesia with 4% articaine, the duration of the anesthetic effect was 199.3 min, versus 1.6 min [27]. In another study, Sovatdy et al. reported that the complete loss of numbness was shorter in IO anesthesia (243.56 ± 38.02 min) than in IANB (291.6 ± 40.28 min) [16]. Average duration of IO anesthesia for normal mandibular teeth is 60 min [28], whereas the IANB has a longer duration (192 min) than IO anesthesia [29]. In our series, the duration of postoperative soft tissue anesthesia was shorter in transcortical anesthesia (range, 15–160 min; mean, 62.5 min) than in IANB (range, 60–240 min; mean, 129 min). Differences in the durations of the anesthetic effect could be associated with measurement techniques and anesthetic solutions and dosages. We used the sharp explorer test to measure the duration of anesthesia rather than the subjective expression of patients.
In two patients, temporary lingual nerve paresthesia was reported following IO anesthesia in our study. However, we were not able to identify if lingual paresthesia was associated with the anesthesia technique or the surgical procedure. To determine the incidence of tissue injury related with IO anesthesia, noninvasive dental procedures should be performed in future studies.
In our study, the amount of maximum mouth opening and pain levels was analyzed on the postoperative first, third, and seventh days to determine if muscle injury was associated with IANB procedure affecting the amount of maximum mouth opening or pain level. Although the same surgical procedure was applied to both sides of patients with bilateral impacted third molars with the same difficulty index, the surgical procedure itself can influence the maximum mouth opening and pain while opening. To better understand the effect of anesthetic method on mouth opening, a split-mouth study should be used.
The success rate of pulpal anesthesia in the first molars by IANB at 60 min was reported to be 92% [1]. IO anesthesia provided successful pulpal anesthesia in 87% of patients, while IANB provided 60% success rate in 20 min [30]. Fernandez et al. reported 154, 152, 138, and 148 min of pulpal anesthesia in the mandibular first premolar, mandibular second premolar, mandibular first molar, and mandibular second molar, respectively, following IANB with lidocaine [29]. In our study, the ratings of postoperative pulpal anesthesia were statistically significantly lower in group I than in group II for two molars and two premolars on 15, 30, 45, and 60 min postoperatively. On 75 and 90 min postoperatively, pulpal anesthesia for the second molar is still significantly higher in group II than in group I. This result is consistent with the duration of soft tissue anesthesia adjacent to the extraction socket in our study. However, pulpal anesthesia of the premolars and first molar disappeared earlier compared with the other studies.
In a study that similarly used the QuickSleeper system, 69.7% of the included 30 patients preferred IO anesthesia to IANB [27]. Sixou et al. reported that 58.9% of the 50 included patients preferred IO anesthesia with QuickSleeper to IANB [31]. In our study 63.3% of the patients preferred IO anesthesia to IANB as IO anesthesia has significant anesthetic effect with less pain during injection and less numbness in the cheek and lip tissues.
The described IO anesthetic system is effective, with a significantly shorter latency, more sufficient duration and depth when performing impacted third molar surgery, significantly lesser soft tissue anesthetic effect considering that IO anesthesia does not anesthetize the lips, and less numbness in the gingiva than the conventional technique. Although IO anesthesia has several advantages, IANB is still widely used by dental practitioners and oral surgeons as this conventional technique does not require extra equipment. Practitioners can immediately apply the IO anesthesia in cases of failures or insufficiencies of the conventional technique.
ACKNOWLEDGMENTS
This study has been presented as poster presentation in BAOMS Annual Scientific Meeting 2016 with the following title: “Clinical evaluation of efficacy of transcortical anesthesia for the extraction of impacted mandibular third molars”.
References
1. Hung PC, Chang HH, Yang PJ, Kuo YS, Lan WH, Lin CP. Comparison of the Gow-Gates mandibular block and inferior alveolar nerve block using a standardized protocol. J Formos Med Assoc. 2006; 105:139–146. PMID: 16477334.

2. Goldberg S, Reader A, Drum M, Nusstein J, Beck M. Comparison of the anesthetic efficacy of the conventional inferior alveolar, Gow-Gates, and Vazirani-Akinosi techniques. J Endod. 2008; 34:1306–1311. PMID: 18928837.

3. Verma PK, Srivastava R, Ramesh KM. Anesthetic efficacy of X-tip intraosseous injection using 2% lidocaine with 1:80,000 epinephrine in patients with irreversible pulpitis after inferior alveolar nerve block: a clinical study. J Conserv Dent. 2013; 16:162–166. PMID: 23716971.

4. Boonsiriseth K, Sirintawat N, Arunakul K, Wongsirichat N. Comparative study of the novel and conventional injection approach for inferior alveolar nerve block. Int J Oral Maxillofac Surg. 2013; 42:852–856. PMID: 23265758.

5. Razavian H, Kazemi S, Khazaei S, Jahromi MZ. X-tip intraosseous injection system as a primary anesthesia for irreversible pulpitis of posterior mandibular teeth: a randomized clinical trail. Dent Res J (Isfahan). 2013; 10:210–213. PMID: 23946738.
6. Cohen HP, Cha BY, Spångberg LS. Endodontic anesthesia in mandibular molars: a clinical study. J Endod. 1993; 19:370–373. PMID: 8245762.

7. Reisman D, Reader A, Nist R, Beck M, Weaver J. Anesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:S132–S139. PMID: 23063389.

8. Bigby J, Reader A, Nusstein J, Beck M, Weaver J. Articaine for supplemental intraosseous anesthesia in patients with irreversible pulpitis. J Endod. 2006; 32:1044–1047. PMID: 17055903.

9. Idris M, Sakkir N, Naik KG, Jayaram NK. Intraosseous injection as an adjunct to conventional local anesthetic techniques: a clinical study. J Conserv Dent. 2014; 17:432–435. PMID: 25298642.

10. NIH consensus development conference for removal of third molars. J Oral Surg. 1980; 38:235–236. PMID: 6101618.
11. Werkmeister R, Fillies T, Joos U, Smolka K. Relationship between lower wisdom tooth position and cyst development, deep abscess formation and mandibular angle fracture. J Craniomaxillofac Surg. 2005; 33:164–168. PMID: 15878516.

12. Chevalier V, Arbab-Chirani R, Tea SH, Roux M. Facial palsy after inferior alveolar nerve block: case report and review of the literature. Int J Oral Maxillofac Surg. 2010; 39:1139–1142. PMID: 20605412.

13. Smail-Faugeron V, Muller-Bolla M, Sixou JL, Courson F. Split-mouth and parallel-arm trials to compare pain with intraosseous anaesthesia delivered by the computerised Quicksleeper system and conventional infiltration anaesthesia in paediatric oral healthcare: protocol for a randomised controlled trial. BMJ open. 2015; 5:e007724.

14. Madan GA, Madan SG, Madan AD. Failure of inferior alveolar nerve block: exploring the alternatives. J Am Dent Assoc. 2002; 133:843–846. PMID: 12148677.
15. Özer S, Yaltirik M, Kirli I, Yargic I. A comparative evaluation of pain and anxiety levels in 2 different anesthesia techniques: locoregional anesthesia using conventional syringe versus intraosseous anesthesia using a computer-controlled system (Quicksleeper). Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:S132–S139. PMID: 23063389.

16. Sovatdy S, Vorakulpipat C, Kiattavorncharoen S, Saengsirinavin C, Wongsirichat N. Inferior alveolar nerve block by intraosseous injection with Quicksleeper® at the retromolar area in mandibular third molar surgery. J Dent Anesth Pain Med. 2018; 18:339–347. PMID: 30637344.

17. Horalek AA. A new approach to intraosseous anesthesia: the Intraflow™ HTP Anesthesia System. Dent Trib Russ. 2008; (6):
18. Eshghpour M, Rezaei NM, Nejat A. Effect of menstrual cycle on frequency of alveolar osteitis in women undergoing surgical removal of mandibular third molar: a single-blind randomized clinical trial. J Oral Maxillofac Surg. 2013; 71:1484–1489. PMID: 23866782.
19. Xue P, Wang J, Wu B, Ma Y, Wu F, Hou R. Efficacy of antibiotic prophylaxis on postoperative inflammatory complications in Chinese patients having impacted mandibular third molars removed: a split-mouth, double-blind, self-controlled, clinical trial. Br J Oral Maxillofac Surg. 2015; 53:416–420. PMID: 25794779.

20. Zandi M, Amini P, Keshavarz A. Effectiveness of cold therapy in reducing pain, trismus, and oedema after impacted mandibular third molar surgery: a randomized, self-controlled, observer-blind, split-mouth clinical trial. Int J Oral Maxillofac Surg. 2016; 45:118–123. PMID: 26597577.

21. Smyth J, Marley J. An unusual delayed complication of inferior alveolar nerve block. Br J Oral Maxillofac Surg. 2010; 48:51–52. PMID: 19297060.

22. Pogrel MA. What is the effect of timing of removal on the incidence and severity of complications? J Oral Maxillofac Surg. 2012; 70:S37–S40. PMID: 22705212.

23. Wright EF. Medial pterygoid trismus (myospasm) following inferior alveolar nerve block: case report and literature review. Gen Dent. 2011; 59:64–67. PMID: 21613042.
24. Woodmansey KF, White RK, He J. Osteonecrosis related to intraosseous anesthesia: report of a case. J Endod. 2009; 35:288–291. PMID: 19166792.

25. Coggins R, Reader A, Nist R, Beck M, Meyers WJ. Anesthetic efficacy of the intraosseous injection in maxillary and mandibular teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996; 81:634–641. PMID: 8784893.

26. Graetz C, Fawzy-El-Sayed KM, Graetz N, Dörfer CE. Root damage induced by intraosseous anesthesia. An in vitro investigation. Med Oral Patol Oral Cir Bucal. 2013; 18:e130–e134. PMID: 23229260.
27. Beneito-Brotons R, Peñarrocha-Oltra D, Ata-Ali J, Peñarrocha M. Intraosseous anesthesia with solution injection controlled by a computerized system versus conventional oral anesthesia: a preliminary study. Med Oral Patol Oral Cir Bucal. 2012; 17:e426–e429. PMID: 22143722.

28. Replogle K, Reader A, Nist R, Beck M, Weaver J, Meyers WJ. Anesthetic efficacy of the intraosseous injection of 2% lidocaine (1:100,000 epinephrine) and 3% mepivacaine in mandibular first molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 83:30–37. PMID: 9007920.

29. Fernandez C, Reader A, Beck M, Nusstein J. A prospective, randomized, double-blind comparison of bupivacaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005; 31:499–503. PMID: 15980707.

30. Remmers T, Glickman G, Spears R, He J. The efficacy of IntraFlow intraosseous injection as a primary anesthesia technique. J Endod. 2008; 34:280–283. PMID: 18291275.

31. Sixou JL, Barbosa-Rogier ME. Efficacy of intraosseous injections of anesthetic in children and adolescents. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:173–178. PMID: 18424118.

Fig. 1
QuickSleeper device has been set up (a) Anesthetic solution is deposited in the distal cancellous bone adjacent to the mandibular third molar tooth to be anesthetized (b)
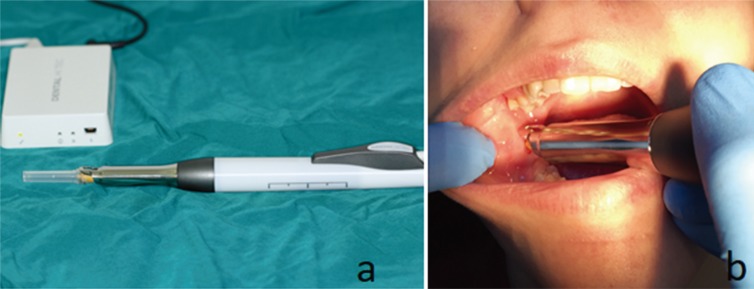
Table 1
Latent period of two anesthesia techniques
| Group I | Group II | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Min | Max | Mean | SD | Min | Max | Mean | SD | P | |
| LP (sec) | 30 | 20 | 150 | 53 | 20.92 | 100 | 300 | 190 | 55.74 | < 0.001 |
Table 2
The pain ratings for injections and operations of two anesthesia techniques
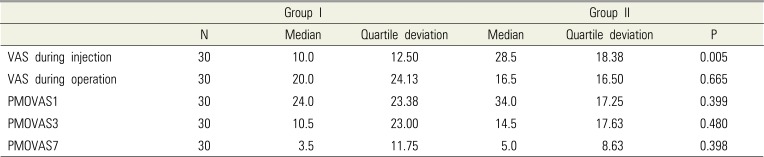
Table 3
The maximum mouth opening after operation




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download