This article has been
cited by other articles in ScienceCentral.
Abstract
Cri-du-chat syndrome (CdCS) is caused by the deletion of the short arm of chromosome 5. Most patients with CdCS develop intellectual disabilities. Therefore, they have poor oral hygiene and a high caries index. However, treating such patients is not an easy task, because of the difficulty in communication. General anesthesia may be a useful option in adult patients with CdCS and intellectual disability. General anesthesia should be administered very carefully, owing to the presence of comorbid diseases, which may need airway management. Infants with CdCS need general anesthesia if they have a concomitant cardiac anomaly. Intubation is reportedly difficult for such patients was, owing to the structural and functional abnormalities in the larynx and vocal cords. The purpose of this study was to report a case of difficult intubation while inducing general anesthesia in a patient with CdCS during dental treatment, due to a narrow larynx and trachea.
Go to :

Keywords: Airway Management, Anesthesia, Congenital Abnormalities, Cri-du-Chat Syndrome, Outpatients
INTRODUCTION
Cri-du-chat syndrome (CdCS) is caused by deletion of the short arm of chromosome 5, which results in cardiac, cerebral, renal, and facial malformations, depending on the location and extent of the defect. Abnormalities in the structure and function of the larynx and vocal cords are the most common phenotype [
12]. The prevalence of CdCS is estimated to be 1 in 50,000 live births and most patients with CdCS have intellectual disability [
13].
Maintaining oral hygiene is extremely difficult in patients with intellectual disability. Thus, all patients with intellectual disability may have periodontal disease, and several patients have dental caries [
4]. General anesthesia is essential for dental treatment in non-cooperative adults with intellectual disabilities [
5].
However, patients with intellectual disabilities have difficulties with preoperative examination, often have systemic diseases or concomitant malformations, and in some cases, anesthesia may be inevitable even for evaluating the patient's general condition [
6].
In this study, we reported the experience of performing nasotracheal intubation and measurement of vocal cord length in an adult patient with CdCS.
Go to :

CASE REPORT
The patient was a 24-year-old woman, who was diagnosed with CdCS in infancy. She had grade 1 intellectual disability and abnormal gait due to neuromotor malfunction. General anesthesia was advised, because oral examination was not possible owing to the intellectual disability.
The caregiver stated that internal organ malformations were absent. She was 150 cm tall and weighed 42 kg. Only partial airway evaluation and parental interviews were performed, since preoperative examinations including blood tests were not possible because of poor coordination. Although the American Society of Anesthesiologists (ASA) physical status classification could not be made accurately, it was estimated to be ASA 2, because the patient appeared physically was healthy and had no other medical condition disease. No abnormalities were noted in with the aperture and cervical spine; However, she had a difficult airway, which was caused by class 2 malocclusion and micrognathia, with a broad nasal bridge and epicanthal folds, which are characteristic of CdCS.
Dental examinations and treatments were planned under outpatient general anesthesia, and the following procedure was used for inducing general anesthesia.
The patient refused to sit on the dental chair, but her parents managed to soothe her and mask induction was started with inhalation of 50% nitrous oxide and oxygen and sevoflurane (4 vol%), followed by sedation. Airway obstruction occurred as the patient calmed down. Thus, positive pressure ventilation was performed using the oropharyngeal airway. Patient monitors for evaluating blood pressure in a noninvasive manner, temperature, pulse oximetry, and electrocardiography were attached simultaneously. An intravenous line was obtained and rocuronium 20 mg was injected. A cotton swab soaked with epinephrine (Bosmin®R) (1 mg/1 cc) was applied to both nasal cavities to facilitate smooth nasotracheal intubation.
Nasotracheal intubation was performed after sufficient neuromuscular blockade. First, the endotracheal tube (ETT) was passed through the left nostril, using a laryngoscope with a size 3 Macintosh curved blade. However, intubation was impossible due to a Cormack-Lehane grade of 4, i.e., the vocal cord was not exposed (
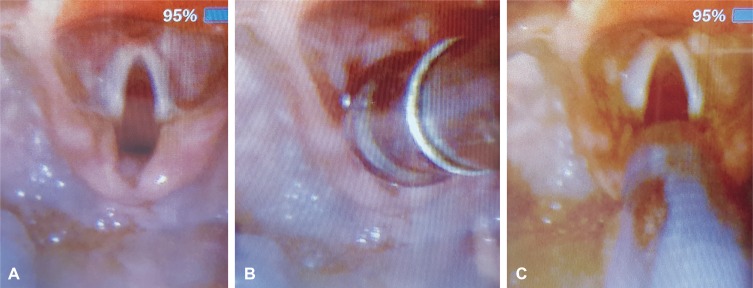
Fig. 1). After immediate removal of the instrument, oxygen supply and anesthesia depth were maintained using 100% oxygen and 4 vol% of sevoflurane. Subsequently, video laryngoscopes (AceScope, Acemedical Co., Korea) were prepared, and the vocal cord was easily exposed using the same laryngoscope blade (
Fig. 2A).
 | Fig. 1Laryngoscopic field of view (in the stable condition) after successful intubation using a size 3 Macintosh curved blade. The Cormack-Lehane Grade was 4 before intubation, but intubation could not be delayed to take a photograph.
|
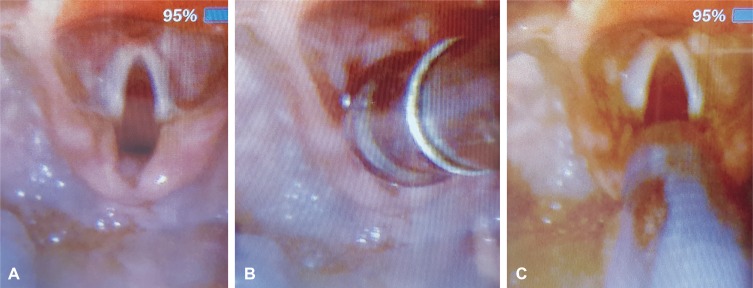 | Fig. 2A: Field of view using video laryngoscopy. A small epiglottis and vocal cord are visible. Vocal cord is fully relaxed. B: The vocal cord is completely covered by Yankauer's suction with an outer diameter of 9.4 mm. C: Intubation with endotracheal tube with an outer diameter of 8.0 mm and an inner diameter of 5.5 mm with a balloon.
|
The ETT was too thick to pass through the vocal cord but could pass through the nostrils, even though an ETT with an inner diameter (ID) of 6.0 mm and outer diameter (OD) of 8.6 mm was selected after considering patient's age, sex, and height. Intubation was possible with an ETT with an ID of 5.5 mm, although it was difficult due to the wider OD of the anterior part of the balloon (
Fig. 2B and C). An inflation pressure of 30 cmH
2O was applied without inflating the balloon after intubation. Thus, we decided to replace the ETT with one with a smaller OD because absolutely no air leaked was observed. Nonetheless, we proceeded with the intubated tube, since the expected treatment time was short and repeated intubation attempts were considered to be detrimental to the patient. Dexamethasone 10 mg was administered to prevent post-intubation stridor. Desaturation or bleeding were not observed during the induction process.
The ETT was placed at a depth of 23 cm from thenares. Anesthesia was maintained with 50% nitrous oxide, oxygen, and 2 vol% of sevoflurane. The peak airway pressure was between 15 and 17 cmH2O when the partial pressure of end tidal carbon dioxide was maintained at approximately 30 mmHg using the volume control mode. A dentist from the department of preventive dentistry performed the oral examination. The patient's oral hygiene was very poor: extensive calculus deposition was observed. Oral prophylaxis was performed with an ultrasonic scaler. The follow-up visit was planned after 18 months.
A neuromuscular-blocking reversal agent was administered after the procedure. Extubation was performed with a positive pressure of 30 cmH2O, following recovery from anesthesia and confirmation of spontaneous breathing and eye opening. Vital signs were observed within approximately 3 min while providing 100% oxygen, and the patient was shifted to the recovery room. For the dental treatment procedure required 95 min and 130 min for anesthesia. No complications were observed during recovery and the patient was discharged.
Go to :

DISCUSSION
CdCS is a genetic disease caused by the deletion of the short arm of chromosome 5, which may be accompanied by facial deformities and cardiac and renal anomalies, in addition to the characteristic cat-crying; therefore, careful preoperative examination is necessary [
1], which is difficult in patients with poor coordination [
6]. In such cases, a complete medical history and written consent (after thorough explanation) must be obtained from the caregiver. Preoperative examination could not be performed at all, since the patient (an adult woman with intellectual disability) was uncooperative. No specific findings were observed after auscultation and on the electrocardiogram after the induction of general anesthesia.
Physical examination is also very important in addition to the patient's medical history. Since the evaluation of the Mallampati score depends on verbal commands, the amount of mouth opening and movement of the neck could not be confirmed; airway evaluation was conducted by carefully observation of the patient's movements. No abnormalities were observed but a difficult airway was expected considering the thyromental distance between the lower jaw and thyroid gland and protrusion of the anterior teeth [
7].
Acquiring an intravenous line is one of the essential steps for general anesthesia. Unfortunately, most patients with intellectual disabilities are afraid of needles [
6]. Using physical restraints during this process can injure medical personnel, assistants, and patients. If the patient is not very cooperative, benzodiazepine-based sedatives can be used as pre-anesthetic drugs to limit the use of body restraint, secure the intravenous line, and subsequently, induce anesthesia [
7]. However, this method cannot be used if short treatment is planned or if the patient refuses to take the drug; thus, a noninvasive method of inducing anesthesia is needed., We used nitrous oxide and sevoflurane as alternatives, to soothe the patient and secure the intravenous line, which can be used effectively in several patients [
8]. Initially, the patient responded negatively to the mask. Soon after, she relieved with no stimulation other than mask breathing. Nevertheless, assisted breathing was initiated using the oropharyngeal airway to treat respiratory distress caused by the patient's airway structure [
8].
The ideal ID of the ETT is controversial, although it depends on the purpose of intubation. A thicker ETT is preferred for ease of sputum discharge and reduction of respiratory work in patients requiring spontaneous breathing and assisted ventilation in the intensive care unit [
9]. A thinner ETT is preferred, as it reduces tracheal damage. Intubation may be easy with a thin ETT. However, according to the well-known Hagen-Poiseuille equation for laminar flow, the flow reduces 16-fold if the ID is reduced by half, thereby increasing the peak airway pressure during anesthesia, which increases breathing work at the end of anesthesia (while inducing spontaneous breathing) [
10].
The factor affecting the ETT thickness are gender, height, age and race. Chinese studies have found that the appropriate thickness of the ETT for Asian children, is thinner than that reported by previous Western studies and the height of the patient is the most relevant factor during selection [
11], since height affects larynx size, vocal fold length, and trachea thickness [
12].
The larynx is funnel-shaped in children and the narrowest cricoid cartilage is the narrowest point; however, it is cylindrical in adults. The width of the trachea can be greater than the inner diameter of the larynx (11–15 mm) in adult women [
13]. We assumed that the ID of the trachea was similar to the OD of the ETT in this case, since it was difficult to pass a tube of 8.0 mm diameter without air leakage. Although this size is used in children younger than 10 years, our patient was 24 years old, and her height and weight corresponded to adult standards. Therefore, we can infer that an immature upper airway specific to CdCS was identified in this adult patient. Previous studies in patients with CdCS, primarily reported cardiac surgery in infancy or after local anesthesia in childhood and mainly discussed respiratory distress after inducing sedation and difficulty in mask ventilation caused by micrognathia and protruding anterior teeth of pediatric patients [
14]. There were no reports on the difficulties caused by an immature upper airway during the induction of general anesthesia.
Although it was regrettable that no additional information about the patient's airway was obtained, additional sedation could not be performed for research purposes. General anesthesia or sedation are inevitable for dental treatment for adults with disabilities, including those with CdCS. Further epidemiological studies of immature upper airways in such patients with active case collection are needed.
In conclusion, the oropharyngeal airway must be prepared in patients with CdCS as they are generally expected to have difficult airways. Furthermore, emergency airway maintenance equipment should be prepared, including smaller ETTs than expected, since the immature upper airway might be a problem.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download