Abstract
Purpose
Materials and Methods
Results
Conclusions
Figures and Tables
 | Fig. 1Discrimination and calibration plots in the derivation cohort. (A) Discrimination. (B) Calibration. |
 | Fig. 2Discrimination and calibration plots in the validation cohort. (A) Discrimination. (B) Calibration. |
Table 1
Baseline characteristics of participants in the derivation and validation cohorts for nephrolithiasis (NPL)

Values are presented as mean±standard deviation or number (%). The sum of the percentages does not equal 100% because of rounding.
SBP, systolic blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; Tx., medical utilisation due to diabetes; HTN, hypertension; Rx., medication utilisation due to hypertension; IBD, inflammatory bowel disease; CKD, chronic kidney disease; IHD, ischemic heart disease.
Table 2
Hazard ratios (HRs) (95% confidence interval [CI]) and β-coefficients for risk predictors in the univariate, partially adjusted, and fully adjusted analyses

Tx., medical utilisation due to diabetes; Rx., medication utilisation due to hypertension; SE, standard error; SBP, systolic blood pressure; DBP, diastolic blood pressure.
a:Univariate analysis. b:Partially adjusted for age, sex and each variable added. c:Fully adjusted accounting for age, sex, income grade, physical activity, smoking status, alcohol consumption and each of the other risk factors (a:fasting blood glucose/diabetes, total cholesterol, blood pressure/HTN, prior history of [ischemic heart disease, chronic kidney disease, hyperparathyroidism, inflammatory bowel disease and gout])
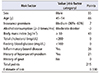
Table 3
Hazard ratios (HRs) (95% confidence interval [CI]) and β-coefficients for risk predictors in the parsimonious model of nephrolithiasis and the risk point scoring system

Table 4
Model validation and performance evaluation based on discrimination and calibration in derivation and validation cohorts

CI, confidence interval.
a:Measures both discrimination and calibration; range (0 to 1) and lower values indicate higher accuracy. b:A modification of Hosmer–Lemeshow test suited for survival data; measure of calibration that is specific to censored survival data (lower χ2 and higher p-values) indicate better calibration. c:A measure of discrimination for which higher values indicate better discrimination.
Notes
AUTHORS' CONTRIBUTIONS
Research conception and design: David Mukasa.
Data acquisition: Joohon Sung.
Statistical analysis: David Mukasa.
Data analysis and interpretation: David Mukasa and Joohon Sung.
Drafting of the manuscript: David Mukasa.
Critical revision of the manuscript: David Mukasa and Joohon Sung.
Supervision: Joohon Sung.
Approval of the final manuscript: all authors.




 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download