This article has been
cited by other articles in ScienceCentral.
Abstract
Traumatic intramural duodenal hematoma (IMDH) is a rare disease occurring usually in children. The treatment modality of traumatic IMDH varies according to clinical manifestations. We had a case of a young man who had traumatic IMDH and treated nonoperatively. He had 3 weeks of conservative care and has been discharged, with follow up abdominal CT scan showing complete resolution of the hematoma. In conclusion, patient with traumatic acute intramural hematoma of duodenal 2nd and 3rd portion have excellent clinical outcomes with conservative therapy.
Go to :

Keywords: Hematoma, Duodenum, Trauma, Conservative management
INTRODUCTION
Traumatic intramural duodenal hematoma (IMDH) is a rare disease occurring usually in childhood. However, cases of IMDH has steadily been reported in many institutions worldwide. The treatment modality varies according to the symptoms, clinical manifestations and complications presented by patients. Here we introduce a case of a young man with a IMDH caused by traumatic event, who has been treated nonoperatively for 3 weeks and has been discharged with no specific complications.
Go to :

CASE
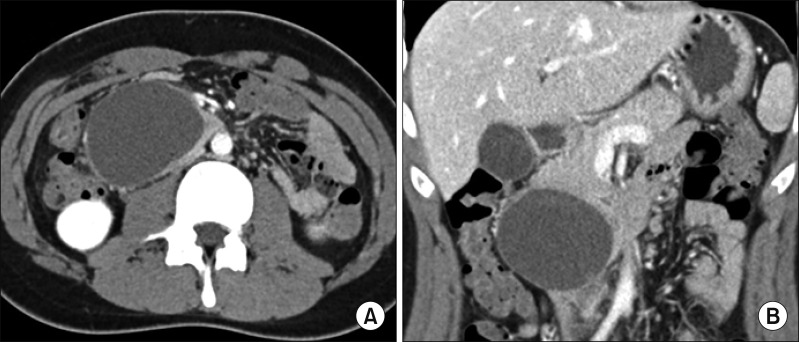
A 17-year-old male patient who had been vomiting and had poor oral intake for 4 days was admitted to our institution, after visiting another hospital. There he underwent an upper gastric endoscopy for further evaluation of any cause of gastric outlet obstruction symptoms. Upper endoscopy revealed the erosion with hyperemic mucosa in the duodenal bulb and complete obstruction of the second duodenal portion caused by external compression. Following abdominal CT scan revealed a large mass (about 8.7×4.5×5 cm) with an internal hemorrhage abutting and compressing the lumen of the duodenal second and third portion (
Fig. 1A, B). With the diagnosis of enteric cyst of duodenum 2nd–3rd, he was sent to our hospital for surgical management. And esophagogastroduodenoscopy (EGD) showing extrinsic compression and ulcerative mass like lesion of duodenum 2nd and 3rd portion (
Fig. 1C, D).
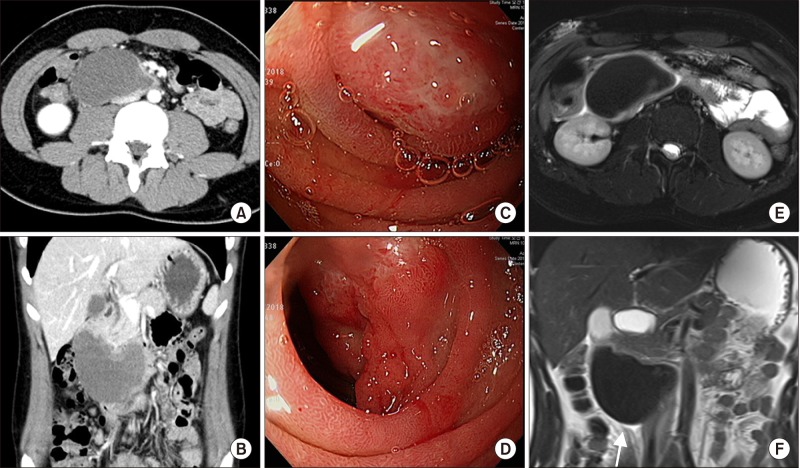 | Fig. 1(A), (B) are axial and coronal view of abdominopelvic CT, showing intramural hematoma of duodenum 2nd and 3rd portion. (C), (D) are endoscopic finding, showing extrinsic compression and ulcerative mass like lesion of duodenum 2nd and 3rd portion. (E), (F) are axial and coronal view of MRI, showing about 8.5×5.5×4.5 cm, acute intramural hematoma of duodenal 2nd and third portion.
|
On his arrival to our hospital, there was no mention of any traumatic events written on referral from the other hospital, so we neglected the possibility of traumatic causes. We decided to take MRI scan to further distinguish the structural relationship of the cyst from other adjacent organs. The source of the GI symptoms revealed in MRI scan was found to be the acute intramural hematoma of duodenal 2nd and 3rd portion, and localized geographic infiltrative lesion of subcutaneous fat tissue of right anterior abdominal wall (
Fig. 1E, F). At the same time, we found out that the patient had the traumatic event the day before the symptoms developed, where he tripped on the threshold and hit his upper stomach hard on the metal doorknob which caused him significant pain. Excluding any hereditary coagulopathy or hemorrhage disease history, we diagnosed him with traumatic intramural duodenal hematoma.
Since there is no standard treatment for traumatic intramural duodenal hematoma, and considering the fact that the patient had to take a national evaluation of educational achievement test in few weeks, we decided to take on conservative management rather than an invasive surgical treatment. Total parenteral nutritional therapy with adequate fluid replacement and nil per os (NPO) was applied. Levin tube insertion was not necessary since there was no significant gastro stasis. The patient was administered 2nd generation cephalosporin antibiotics. Blood tests were taken approximately twice a week to examine abnormalities of hemoglobin decreases or electrolytes imbalance caused with NPO. Soon after, the patient was able to take some sips of water or small bites of fruits with no abdominal discomfort or vomiting.
On the 14th day of admission, which also showed rare decrease in size of IMDH (
Fig. 2). And the patient was able to eat small amounts of soft diets tolerably. Nevertheless, the patient was able to eat tolerable amount of food with no IV fluid replacement. After the patient took the national evaluation of educational achievement test, as the patient resolved in symptoms of vomiting and poor oral intake, we decided to further follow up the CT scan after 1 month of discharge.
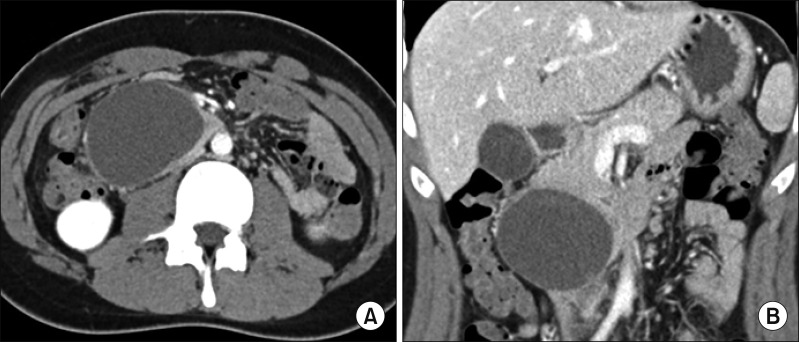 | Fig. 2Abdominopelvic CT follow up taken on 14th day of admission showed minimal decrease in size of intramural hematoma of duodenum. (A) is axial view and (B) is coronal view.
|
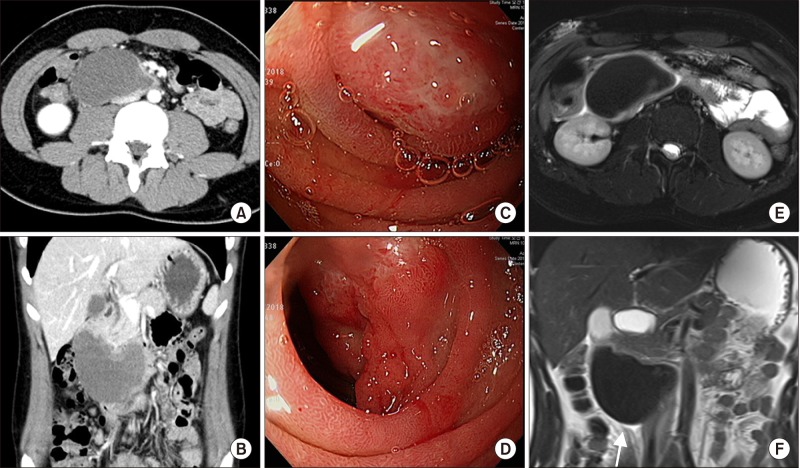
7 weeks after the diagnosis of IMDH, the patient revisited the outpatient clinic with 3rd follow up CT scan. On the CT scan, the intramural hematoma located in 2nd to 3rd portion of duodenum has completely resolved with very minimal periduodenal fluid left (
Fig. 3). The patient had no limitations to consuming foods. We decided not to further follow up the patient.
 | Fig. 3Abdominopelvic CT follow up taken on 7th week after diagnosis of IMDH showed completely resolved with very minimal periduodenal fluid left. (A) is axial view and (B) is coronal view.
|
Go to :

DISCUSSION
The traumatic duodenal injuries occur in the 3–5% of blunt abdominal traumas.
12 The examples of blunt traumatic duodenal injuries include traffic accidents, fall down injuries, assaulting injuries and handlebar injury. The duodenal injury is caused by compression of duodenum against the spine, which results in duodenal hematoma, laceration and perforation.
3
Intramural hematoma of the duodenum (IMDH) was first described in 1838 by McLauchlan, who described “false aneurysmal tumor occupying nearly the whole of the duodenum” in the autopsy note of the man died of dehydration duodenal obstruction.
4 The etiologies of IMDH are categorized into external injury, internal injury and spontaneous. IMDH is caused by external injuries and trauma has been largely reported in the pediatric patients.
356 Internal injury of IMDH is characterized as endoscopic injury; endoscopy itself or endoscopic biopsy.
7 Approximately one out of 2000 patients who receives EGD develops duodenal hematoma. pancreatitis is often thought to irritate the bowel to develop hematoma.
89 Some patients develop spontaneous hematoma due to their bleeding risks, such as anticoagulant agent intake.
10 Some patients have no significant cause for the spontaneous duodenal hematoma.
11 Duodenal hematoma frequently causes gastric obstruction represented as abdominal pain and vomiting. Furthermore upper gastrointestinal bleeding, jaundice, and acute pancreatitis may also be present.
12
There are few cases that treated duodenal hematoma with invasive procedures. In the past, surgical treatment such as evacuation of hematoma or bypass surgery was performed.
13 The lack of radiologic diagnosis had surgeons perform exploratory laparotomy after blunt trauma of the abdomen. Today, surgical procedures are often needed in intra-abdominal complications such as uncontrolled bleeding or panperitonitis.
14 Delayed bowel obstruction and jaundice often led to laparotomy cases.
15 Endoscopic drainage with mucosal puncture or fistula formation has also been performed without significant complications.
16 If accessible through the skin, percutaneous catheter insertion was also performed for decompression of IMDH.
17
However, several case reviews and retrospective studies revealed the effectiveness of conservative care in traumatic IMDH.
678918 The median resolution of the IMDH is 7.69 days and the length of stay in hospital was longer in grade II duodenal injury of AAST duodenal injury scale (involving more than one portion) than in grade I duodenal injury (involving single portion). No apparent limitation of nonoperative treatments was noted, with little complications. Moreover, not only in traumatic but also IMDH caused by other etiologies are now treated with less invasive methods.
7
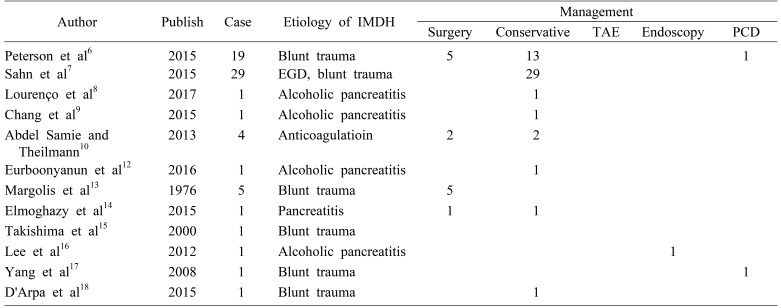
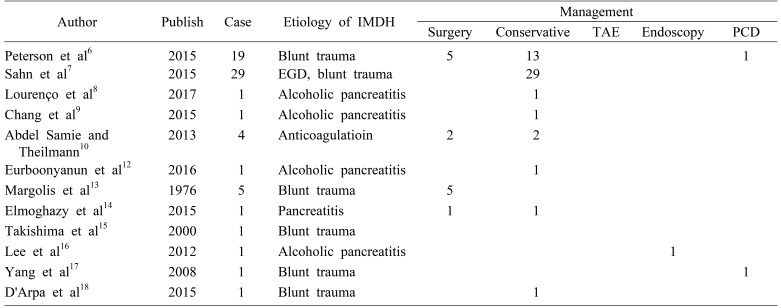
Table 1 summarizes the previously reported treatment cases of intramural duodenal hematoma. Of the 65 patient, conservative treatment was performed in 49 patient. And thirteen patients underwent surgical treatment, percutaneous drainage in two patient, and endoscopic drainage in one patient.
Table 1
Previously reported treatment cases of intramural duodenal hematoma (IMDH)

Traumatic acute intramural hematoma of duodenum is rare. A thorough history taking and adequate radiologic exams are essential for diagnosis of traumatic intramural hematoma of duodenum. Patient with traumatic acute intramural hematoma of duodenal 2nd and 3rd portion have excellent clinical outcomes with conservative therapy.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download