This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
To compare outcomes (i.e., clinical and radiological findings, postoperative complication) in the fixation of intertrochanteric fractures with U-blade Gamma3 and Gamma3 nails.
Materials and Methods
A review of 162 patients (both male and female) treated for intertrochanteric fractures between December 2012 and December 2018 was conducted. All patients were older than 65 years of age and treated with U-blade Gamma3 (n=90) or Gamma3 (n=72) nails. Evaluations included: (i) screw-head position, (ii) fracture-reduction status, (iii) time to union, (iv) cases of cut-out, (v) tip-apex distance, and (vi) lag screw sliding distance. Differences in pre- and postoperative ambulatory ability was also investigated.
Results
There were no significant differences in baseline demographics between the two groups. While the lag-screw sliding distance was significantly shorter in U-blade Gamma3 nail group (4.7 mm vs. 3.6 mm; P=0.025), the mean time to union was similar between the groups (P=0.053). Three and six cases of cut-out were noted in the U-blade Gamma3 and Gamma3 nail groups, respectively (P=0.18), however no other postoperative complications were noted in either group. Lastly, there was no difference between the change from pre- to postoperative activity level between the groups (P=0.753).
Conclusion
Of all the clinical and radiological outcomes assessed, the only significant improvement between those treated with U-Blade Gamma and Gamma3 nails was a shorter lag-screw sliding distance. These findings should benefit clinicians when deciding between the use of U-Blade Gamma or Gamma3 nails.
Go to :

Keywords: Femur, Intertrochanteric fractures, Gamma3 nail, U-blade
INTRODUCTION
The majority of intertrochanteric fractures, which commonly occur in the elderly, require surgical intervention for reduction, maintenance and prevention of complications
1). Previous studies on the surgical treatment of intertrochanteric fractures have demonstrated superiority of dynamic hip screws (DHS) vs. other approaches to achieve surgical fixation
23). However, interlocking intramedullary (IM) nailing has become the primary treatment approach, largely because they are easier to use and their insertion is less invasive compared with fixation using extramedullary sliding screws
4). IM nailing for the management of intertrochanteric fractures also has other advantages compared with fixation using DHS, including shorter operation time, less intraoperative blood loss and prevention of internal fixation breakage
56). The Gamma nail (trochanteric gamma locking nail; Stryker® Trauma GmbH, Schoenkirchen, Germany), the leading IM nail, was developed to treat unstable intertrochanteric fractures and first used clinically in 1988
7). In recent years, a variety of IM nails have been used for the treatment of intertrochanteric femur fractures, but IM nail systems with ideal mechanical performance have not yet been introduced as they still experience rotational deformity, screw cut-out and other problems
2). Updates to Gamma nails have been made over the years to improve performance; the Gamma3 locking nail system (Stryker®), a third-generation IM nailing system
8), is the newest and most commonly used.
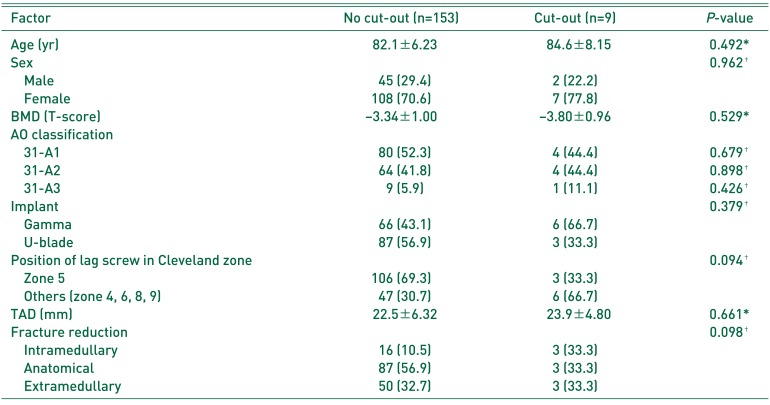
In addition, there are Gamma nails designed with U-blades, the most current being the U-blade Gamma3 nail. This device, designed with a U-blade lag screw, was developed to provide improved outcomes when treating unstable intertrochanteric femur fractures (Gamma3 U-blade lag screw; Stryker® Trauma GmbH (
Fig. 1)
9). The U-blade lag screw for the Gamma3 nail was introduced to better withstand rotational deformity between the femoral head and neck in intertrochanteric fractures
10). The U-blade lag screw has a spreading effect that increases resistance and the surface area of the femoral head where the lag screw is placed
11).
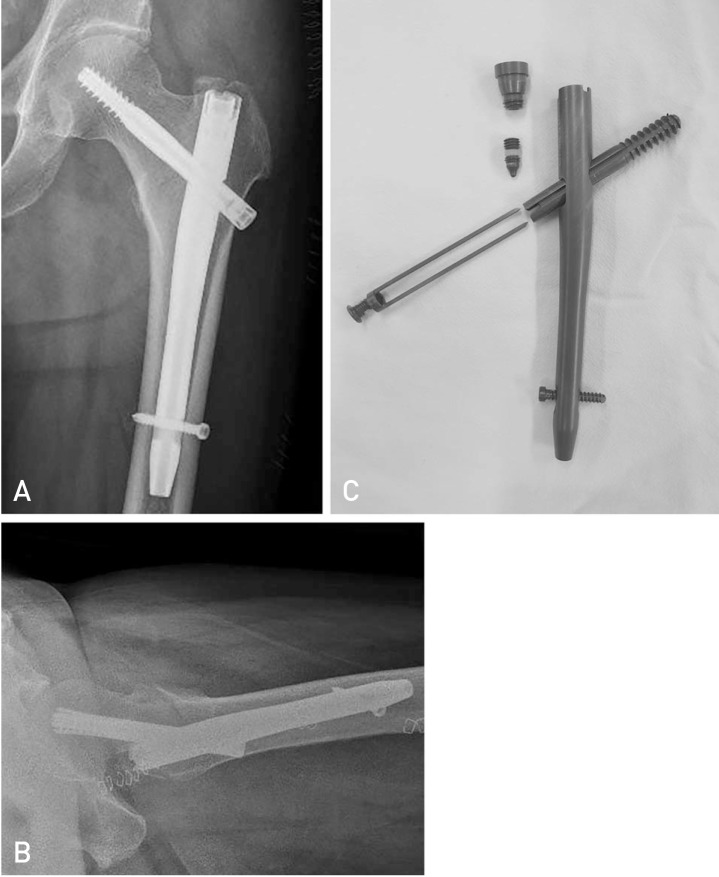 | Fig. 1
(A) Anteroposterior view of intertrochanteric fracture treated with U-blade Gamma3 nail. (B) Trans-lateral view of intertrochanteric fracture treated with U-blade Gamma3 nail. (C) Photograph of U-blade Gamma3 nail.
|
This study was performed to compare surgical outcomes between individuals with intertrochanteric fractures treated with U-blade Gamma3 and Gamma3 nails using clinical and radiological assessments of potential complications and pre- and post-surgical status.
Go to :

MATERIALS AND METHODS
1. Materials
A total of 162 patients who underwent surgery in our hospital for treatment of intertrochanteric fractures between December 2012 and December 2018 and had a minimum follow-up of six months were included in this analysis. Patients were excluded if they: (i) were younger than 65 years of age, (ii) had preoperative Koval grade of 7, (iii) were diagnosed with a high-energy or pathologic fracture, or (iv) died. All operations were performed by three orthopedic surgeons specialized in hip surgery during the study period. Gamma3 nails were used from December 2012 to July 2015, and U-blade Gamma3 nails were used from August 2015 to December 2018. This retrospective analysis included 90 and 72 patients treated with U-blade Gamma3 and Gamma3 nails, respectively.
2. Surgical Methods
All operations were conducted under general anesthesia or spinal anesthesia with patients in the supine position on a fracture-reduction table. Closed reduction was initially attempted under C-arm fluoroscopy with the leg retracted and internally rotated and adducted on the affected side. All operations were performed according to standard operating procedures including reaming in both groups. Wheelchair ambulation was allowed from the day following surgery. Weight-bearing and gait training were initiated based on fracture and reduction status and partial weight-bearing walking ability.
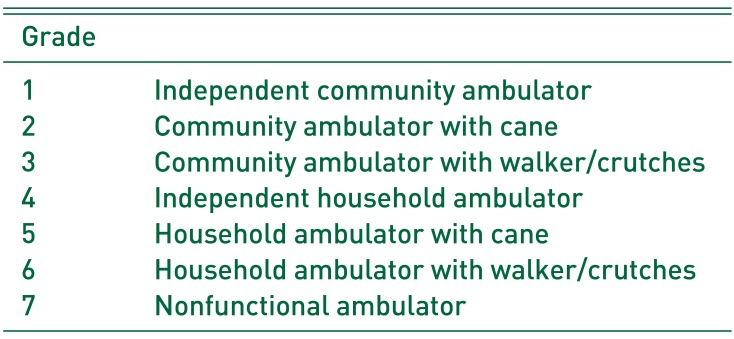
3. Evaluation and Statistical Analysis
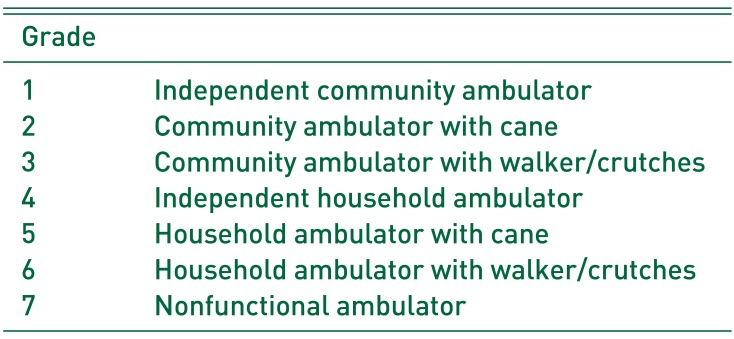
Clinical results were analyzed by comparing comorbidities and surgical and medical complications by reviewing operation records, anesthesia records and medical records. Preoperative ambulatory ability was determined at time of admission; final ambulatory ability was assessed using Harris hip score (HHS) and Koval grade (
Table 1) via telephone survey.
Table 1
Categories of Walking Ability by Koval
|
Grade |
|
|
1 |
Independent community ambulator |
|
2 |
Community ambulator with cane |
|
3 |
Community ambulator with walker/crutches |
|
4 |
Independent household ambulator |
|
5 |
Household ambulator with cane |
|
6 |
Household ambulator with walker/crutches |
|
7 |
Nonfunctional ambulator |

Radiological results were evaluated to assess the stability of fracture reduction according to the contact degree of the inner layer of the cortex on anteroposterior (AP) and lateral hip radiographs obtained immediately after surgery, and at 2, 3, 6, and 12 months postoperatively. The reduction quality was categorized as good, acceptable or poor based on the Baumgartner classification (
Table 2)
12). Furthermore, the frequency of varus fixation, lag screw position in the femoral head, and lag screw cut-out were examined. Screw position within the head was determined using the Cleveland zone
13) divided into 9 zones on the AP and later X-ray views of the femoral head. Screws located in the Cleveland zone 5 were considered to be at the center position of the femoral head. Screws located within other Cleveland zones on any radiographic view were not considered to be in the center position. Radiographic fracture union was determined based on no progression of fracture-site impaction, loss of fracture line, medullary cavity formation at the fracture site and continuity of trabeculae at the fracture site. The tip-apex distance (TAD) was measured in all cases to identify risk factors for lag screw cut-out and postoperative complications. Bone mineral density (BMD) was measured with dual energy X-ray absorptiometry (DEXA) in the spine and proximal femur on the contralateral side and reported as T-scores. The need for hip revision surgery due to postoperative complications (e.g., proximal migration of the lag screw, screw cut-out of the femoral head, failed union) was also examined.
Table 2
Baumgartner Classification for Accuracy of Reduction

|
Reduction |
Normal or slight angulation on anteroposterior view and <20° angulation on lateral view |
|
Displacement |
≤4 mm displacement of any fragment |

The student t-test was used to identify potential differences in the mean value of continuous variables between the two groups, and the Pearson's chi-square test was used to assess associations between categorical variables. Statistical significance was considered at P=0.05. Statistical analyses were performed using IBM SPSS Statistics ver. 23 (IBM Corp,. Armonk, NY, USA). This study was approved by the Institutional Review Board of Seoul Medical Center (no. 2019-08-005).
Go to :

RESULTS
1. Distribution and Characteristics of Subjects
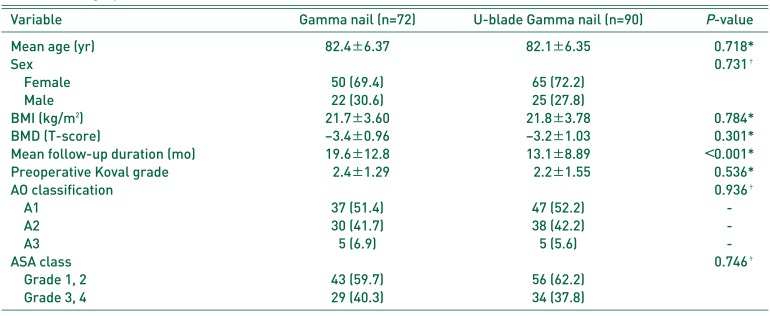
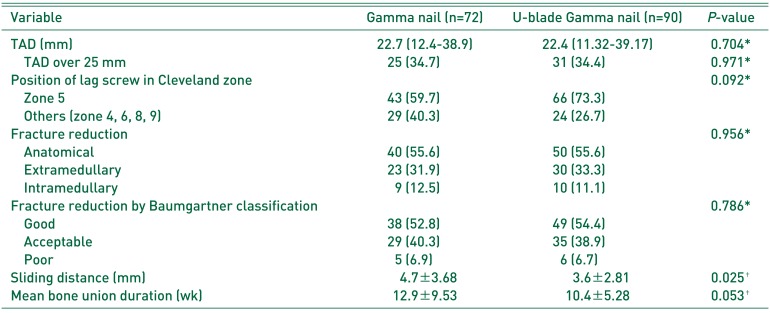
There were no significant difference between the groups treated with the U-blade Gamma3 and Gamma3 nails with respect to: (i) mean ages (82.1 and 82.4 years, respectively; P=0.718), (ii) sex (P=0.731), (iii) mean body mass index (21.8 and 21.7 kg/m2, respectively; P=0.784), (iv) comorbidities (P=0.746) or v) mean T-score measured using DEXA (−3.2 and −3.4, respectively; P=0.301).
2. Clinical Assessment
There was no significant difference between the groups treated with the U-blade Gamma3 and Gamma3 nails based on the AO classification of fracture types: (i) A1 (47 and 37, respectively), (ii) cases of type A1, 30 cases of type A2 (38 and 30, respectively), and A3 (5 in each);
P=0.936. No significant difference was observed in preoperative ambulatory ability between the two groups (
P=0.536). The mean follow-up period was 19.65 months in the Gamma3 nail group and 13.13 months in the U-blade Gamma3 nail group (
Table 3).
Table 3
Demographic Characteristics
|
Variable |
Gamma nail (n=72) |
U-blade Gamma nail (n=90) |
P-value |
|
Mean age (yr) |
82.4±6.37 |
82.1±6.35 |
0.718*
|
|
Sex |
|
|
0.731†
|
|
Female |
50 (69.4) |
65 (72.2) |
|
Male |
22 (30.6) |
25 (27.8) |
|
BMI (kg/m2) |
21.7±3.60 |
21.8±3.78 |
0.784*
|
|
BMD (T-score) |
−3.4±0.96 |
−3.2±1.03 |
0.301*
|
|
Mean follow-up duration (mo) |
19.6±12.8 |
13.1±8.89 |
<0.001*
|
|
Preoperative Koval grade |
2.4±1.29 |
2.2±1.55 |
0.536*
|
|
AO classification |
|
|
0.936†
|
|
A1 |
37 (51.4) |
47 (52.2) |
- |
|
A2 |
30 (41.7) |
38 (42.2) |
- |
|
A3 |
5 (6.9) |
5 (5.6) |
- |
|
ASA class |
|
|
0.746†
|
|
Grade 1, 2 |
43 (59.7) |
56 (62.2) |
|
Grade 3, 4 |
29 (40.3) |
34 (37.8) |

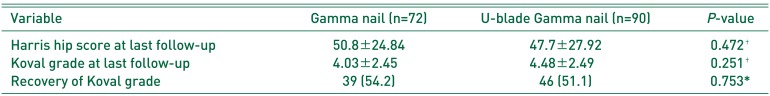
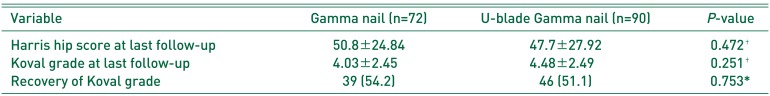
The difference in pre- and postoperative ambulatory ability between the two groups was compared using the Koval classification and HHS, and no difference between the two groups was observed. The change in postoperative ambulatory ability was not statistically different between the two groups (
P=0.753) (
Table 4).
Table 4
Comparison of the Clinical Results
|
Variable |
Gamma nail (n=72) |
U-blade Gamma nail (n=90) |
P-value |
|
Harris hip score at last follow-up |
50.8±24.84 |
47.7±27.92 |
0.472†
|
|
Koval grade at last follow-up |
4.03±2.450 |
4.48±2.490 |
0.251†
|
|
Recovery of Koval grade |
39 (54.2) |
46 (51.1) |
0.753 |

3. Radiologic Assessment
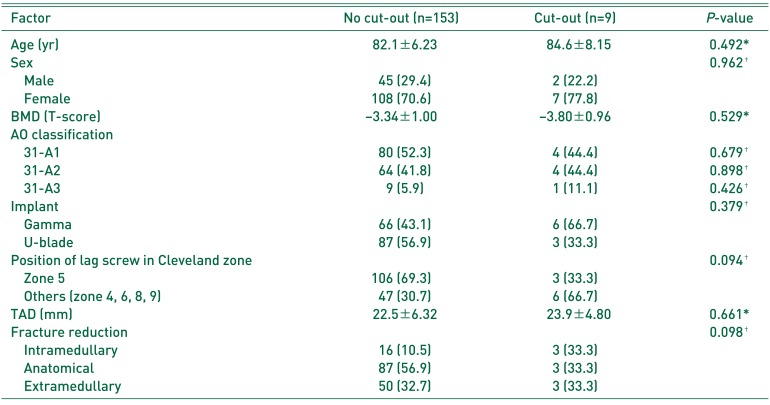
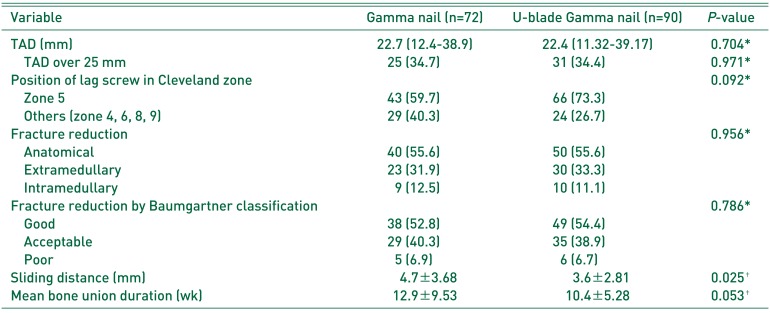
The mean postoperative TAD measured using AP and lateral hip X-rays was not significantly different between the U-blade Gamma3 and Gamma3 nail groups (22.4 and 22.7 mm, respectively; P=0.704). There was no difference in the proportion of patients with TAD values 25±1 mm between the two groups (31 out of 90 and 25 out of 72 cases in the U-blade Gamma3 and Gamma3 groups, respectively; P=0.971). The screw position was located in Cleveland zone 5 in 66 of 90 cases and 43 of 72 cases in the in the U-blade Gamma3 and Gamma3 nail groups, respectively; results which were not significantly different (P=0.092). In regard to fracture reduction, there were 50 cases of anatomical reduction, 30 cases of extramedullary reduction and 10 cases of IM reduction among 90 cases in the U-blade Gamma3 nail group and 40 cases of anatomical reduction, 23 cases of extramedullary reduction and 9 cases of IM reduction among 72 cases in the Gamma3 nail group; these results were also not significantly different (P=0.956). Based on the Baumgartner classification, reduction quality in the 90 patients in the U-blade Gamma3 group was good (n=49), acceptable (n=35), and poor (n=6), compared with good (n=38), acceptable (n=29) and poor (n=5) in the 72 patients in the Gamma3 nail group; these proportions were not significantly different (P=0.786).
The mean sliding distance of the lag screw was significantly shorter in the group treated with U-blade Gamma3 nails compared with Gamma3 nails (3.6 mm and 4.7 mm, respectively;
P=0.025). There was no statistically significant difference in the average time to bone union between patients treated with U-blade Gamma3 nails compared with the Gamma3 nails (10.4 weeks and 12.9 weeks, respectively;
P=0.053) (
Table 5).
Table 5
Comparison of the Radiographic Results
|
Variable |
Gamma nail (n=72) |
U-blade Gamma nail (n=90) |
P-value |
|
TAD (mm) |
22.7 (12.4-38.9) |
22.4 (11.32-39.17) |
0.704*
|
|
TAD over 25 mm |
25 (34.7) |
31 (34.4) |
0.971*
|
|
Position of lag screw in Cleveland zone |
|
|
0.092*
|
|
Zone 5 |
43 (59.7) |
66 (73.3) |
|
Others (zone 4, 6, 8, 9) |
29 (40.3) |
24 (26.7) |
|
Fracture reduction |
|
|
0.956*
|
|
Anatomical |
40 (55.6) |
50 (55.6) |
|
Extramedullary |
23 (31.9) |
30 (33.3) |
|
Intramedullary |
9 (12.5) |
10 (11.1) |
|
Fracture reduction by Baumgartner classification |
|
|
0.786*
|
|
Good |
38 (52.8) |
49 (54.4) |
|
Acceptable |
29 (40.3) |
35 (38.9) |
|
Poor |
5 (6.9) |
6 (6.7) |
|
Sliding distance (mm) |
4.7±3.68 |
3.6±2.81 |
0.025†
|
|
Mean bone union duration (wk) |
12.9±9.53 |
10.4±5.28 |
0.053†
|

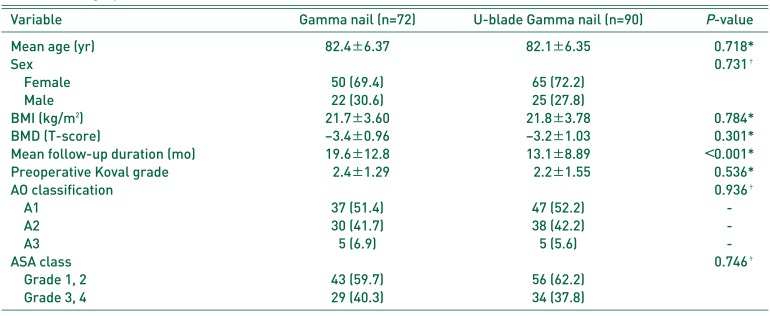
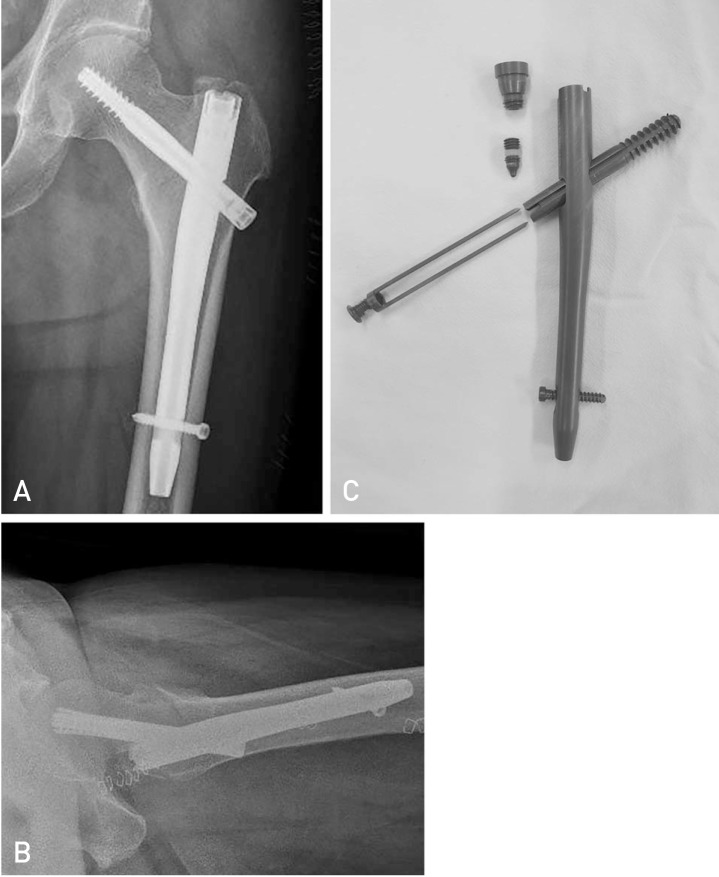
4. Complications
Screw cut-out, a well-known postoperative complication occurred in 3 and 6 individuals in the U-blade Gamma3 and Gamma3 nail groups a difference that was not statistically significant (
P=0.188). The potential association between cut-out and baseline characteristics (e.g., age, sex, BMD, fracture type, implant type, screw position within the head, location of reduction, TAD) was investigated, however, no significant associations were observed (
Table 6). Total hip arthroplasty was performed after the removal of an IM nail in cases with cut-out (
Fig. 2). There were no cases with other postoperative complications (e.g., proximal migration of the lag screw, non-union, peri-implant fracture, infection).
 | Fig. 2
(A) Postoperative anteroposterior radiographs at 1 year of a 97-year-old male with U-blade Gamma3 nail showed fixation failure and blade cut-out through the femoral head into the acetabulum. (B) Revised to a total hip arthroplasty and had returned to walk independently.
|
Table 6
Comparison of the Clinical and Radiographic Results between No Cut-out Group and Cut-out Group
|
Factor |
No cut-out (n=153) |
Cut-out (n=9) |
P-value |
|
Age (yr) |
82.1±6.23 |
84.6±8.15 |
0.492*
|
|
Sex |
|
|
0.962†
|
|
Male |
45 (29.4) |
2 (22.2) |
|
|
Female |
108 (70.6) |
7 (77.8) |
|
|
BMD (T-score) |
−3.34±1.00 |
−3.80±0.96 |
0.529*
|
|
AO classification |
|
|
|
|
31-A1 |
80 (52.3) |
4 (44.4) |
0.679†
|
|
31-A2 |
64 (41.8) |
4 (44.4) |
0.898†
|
|
31-A3 |
9 (5.9) |
1 (11.1) |
0.426†
|
|
Implant |
|
|
0.379†
|
|
Gamma |
66 (43.1) |
6 (66.7) |
|
|
U-blade |
87 (56.9) |
3 (33.3) |
|
|
Position of lag screw in Cleveland zone |
|
|
0.094†
|
|
Zone 5 |
106 (69.3) |
3 (33.3) |
|
|
Others (zone 4, 6, 8, 9) |
47 (30.7) |
6 (66.7) |
|
|
TAD (mm) |
22.5±6.32 |
23.9±4.80 |
0.661*
|
|
Fracture reduction |
|
|
0.098†
|
|
Intramedullary |
16 (10.5) |
3 (33.3) |
|
|
Anatomical |
87 (56.9) |
3 (33.3) |
|
|
Extramedullary |
50 (32.7) |
3 (33.3) |
|

Go to :

DISCUSSION
IM nail fixation is a widely used surgical method for treating intertrochanteric fractures
14), but potential postoperative complications following IM nailing (e.g., rotational deformity, cut-out, proximal rotation of the lag screw) remain a challenge
15). For this reason, this study aimed to investigate the effect of the use of the U-blade lag screw on the occurrence of rotational deformity and lag screw-related complications by comparing the clinical and radiological outcomes between those treated for intertrochanteric fractures with U-blade Gamma3 and Gamma3 nails.
Yoo et al.
9) reported that the use of U-blade Gamma3 nails decreased the rates of complications when used to treat intertrochanteric fractures (e.g., proximal migration of the lag screw) by providing adequate fixation. On the contrary, Lang et al.
11) suggested that the U-blade Gamma3 nail was not effective in reducing complications or achieving better clinical outcomes compared to the conventional Gamma3 nail, especially when considering the additional costs and extended operating time when using the U-blade lag screw.
Importantly, previous studies yielded contradictory results. In the current study, no significant difference was observed with respect to TAD values resulting in sliding of the lag screw in postoperative X-rays between the two groups (
P=0.661), and favorable results were obtained with mean TADs of less than 25 mm in both groups (22.7 mm vs. 22.4 mm). The sliding distance of the lag screw was significantly shorter in the U-blade Gamma3 nail group (4.7 mm vs. 3.6 mm,
P=0.025). This result can be interpreted as resulting from the increased resistance to excessive sliding provided by the U-blade screw, results comparable those reported by Lang et al.
11) who demonstrated that the spreading effect of U-blade lag screw resulted in increased resistance by enlarging the contact surface around the femoral head. Increased resistance against rotation and improved resistance of the U-blade with greater surface area were expected to shorten the time to bone union by enhancing fixation stability, however, no statistically significant difference was found in time to bone union between the two groups tested here (
P=0.053).
Similar to the anatomical reduction of fractures, the status of implant insertion manifested as TAD and femoral head lag screw position is profoundly associated with screw cut-out which is the most common cause for fixation failure following surgical management of intertrochanteric fractures
1617). To analyze potential predictive variables of lag-screw cut-out from the femoral head between the two groups, this study explored age, sex, BMD, fracture type, implant type, screw position within the head, location of reduction, TAD and others. None of these variables were associated with screw cut-out (
Table 6).
It is important to note some of the key limitations to this study. First, the sample size was relatively small, due in part to the loss of several patients to follow-up because of death, an occurrence which was not unexpected because of the age of participants. Second, the interpretation of surgical outcomes of the two different groups should be done cautiously as operations were performed by three different surgeons. Third, fixation failure and complications can be difficult to interpret because of the difference in the follow-up period according to time of operations between the two groups (i.e., pre 2015 and post 2015). Finally, stable and unstable fracture types were both included making assessment of the potential advantages of one nail over the other challenging. Further comparative studies with larger samples, longer-term follow-up and differentiation between facture types are warranted.
Go to :

CONCLUSION
The lag-screw sliding distance was significantly shorter in patients treated with the U-blade Gamma3 nail compared with the Gamma3 nail. Importantly, no significant difference in time to fracture union was observed between the two groups. Of all the clinical and radiological outcomes assessed, the only significant improvement between those treated with U-Blade Gamma and Gamma3 nails was a shorter lag-screw sliding distance.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download