1. Danielsson L, Lindberg H. Prevalence of coxarthrosis in an urban population during four decades. Clin Orthop Relat Res. 1997; (342):106–110.

2. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015; 31:2307–2313.e2. PMID:
26194938.

3. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013; 29:661–665. PMID:
23375668.

4. Schairer WW, Nwachukwu BU, McCormick F, Lyman S, Mayman D. Use of hip arthroscopy and risk of conversion to total hip arthroplasty: a population-based analysis. Arthroscopy. 2016; 32:587–593. PMID:
26671201.

5. Lee JW, Hwang DS, Kang C, Hwang JM, Chung HJ. Arthroscopic repair of acetabular labral tears associated with femoroacetabular impingement: 7-10 years of long-term follow-up results. Clin Orthop Surg. 2019; 11:28–35. PMID:
30838105.

6. Philippon MJ, Ejnisman L, Ellis HB, Briggs KK. Outcomes 2 to 5 years following hip arthroscopy for femoroacetabular impingement in the patient aged 11 to 16 years. Arthroscopy. 2012; 28:1255–1261. PMID:
22560486.

7. Jayakumar P, Ramachandran M, Youm T, Achan P. Arthroscopy of the hip for paediatric and adolescent disorders: current concepts. J Bone Joint Surg Br. 2012; 94:290–296. PMID:
22371532.
8. Byrd JW, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009; 467:739–746. PMID:
19096902.

9. Suarez-Ahedo C, Gui C, Rabe SM, Walsh JP, Chandrasekaran S, Domb BG. Relationship between age at onset of symptoms and intraoperative findings in hip arthroscopic surgery. Orthop J Sports Med. 2017; 5:2325967117737480. PMID:
29226162.

10. Herrmann SJ, Bernauer M, Erdle B, Südkamp NP, Helwig P, Hauschild O. Osteoarthritic changes rather than age predict outcome following arthroscopic treatment of femoroacetabular impingement in middle-aged patients. BMC Musculoskelet Disord. 2016; 17:253. PMID:
27278243.

11. Wilkin G, March G, Beaulé PE. Arthroscopic acetabular labral debridement in patients forty-five years of age or older has minimal benefit for pain and function. J Bone Joint Surg Am. 2014; 96:113–118. PMID:
24430410.

12. Javed A, O'Donnell JM. Arthroscopic femoral osteochondroplasty for cam femoroacetabular impingement in patients over 60 years of age. J Bone Joint Surg Br. 2011; 93:326–331. PMID:
21357953.

13. Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007; 456:128–132. PMID:
17106273.

14. Griffin DW, Kinnard MJ, Formby PM, McCabe MP, Anderson TD. Outcomes of hip arthroscopy in the older adult: a systematic review of the literature. Am J Sports Med. 2017; 45:1928–1936. PMID:
27756723.

15. Piuzzi NS, Slullitel PA, Bertona A, et al. Hip arthroscopy in osteoarthritis: a systematic review of the literature. Hip Int. 2016; 26:8–14.

16. Kemp JL, MacDonald D, Collins NJ, Hatton AL, Crossley KM. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res. 2015; 473:1055–1073. PMID:
25231154.

17. Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016; 50:1169–1176. PMID:
27629403.
18. Hoaglund FT, Steinbach LS. Primary osteoarthritis of the hip: etiology and epidemiology. J Am Acad Orthop Surg. 2001; 9:320–327. PMID:
11575911.

19. Lodhia P, Slobogean GP, Noonan VK, Gilbart MK. Patient-reported outcome instruments for femoroacetabular impingement and hip labral pathology: a systematic review of the clinimetric evidence. Arthroscopy. 2011; 27:279–286. PMID:
21035994.

20. Byrd JW. Evaluation of the hip: history and physical examination. N Am J Sports Phys Ther. 2007; 2:231–240. PMID:
21509142.
21. Stelzeneder D, Mamisch TC, Kress I, et al. Patterns of joint damage seen on MRI in early hip osteoarthritis due to structural hip deformities. Osteoarthritis Cartilage. 2012; 20:661–669. PMID:
22469848.

22. Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoral acetabular impingement in patients with preoperative generalized degenerative changes. Arthroscopy. 2010; 26:623–629. PMID:
20434659.

23. Capogna BM, Ryan MK, Begly JP, Chenard KE, Mahure SA, Youm T. Clinical outcomes of hip arthroscopy in patients 60 or older: a minimum of 2-year follow-up. Arthroscopy. 2016; 32:2505–2510. PMID:
27544591.
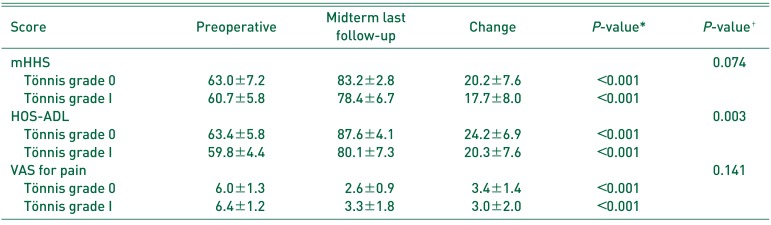
24. Domb BG, Chaharbakhshi EO, Rybalko D, Close MR, Litrenta J, Perets I. Outcomes of hip arthroscopic surgery in patients with Tönnis grade 1 osteoarthritis at a minimum 5-year follow-up: a matched-pair comparison with a Tönnis grade 0 control group. Am J Sports Med. 2017; 45:2294–2302. PMID:
28609644.

25. Chandrasekaran S, Gui C, Darwish N, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of hip arthroscopic surgery in patients with Tönnis grade 1 osteoarthritis with a minimum 2-year follow-up: evaluation using a matched-pair analysis with a control group with Tönnis grade 0. Am J Sports Med. 2016; 44:1781–1788. PMID:
27045086.
26. Egerton T, Hinman RS, Takla A, Bennell KL, O'Donnell J. Intraoperative cartilage degeneration predicts outcome 12 months after hip arthroscopy. Clin Orthop Relat Res. 2013; 471:593–599. PMID:
22992870.

27. Philippon MJ, Schroder E Souza BG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy. 2012; 28:59–65. PMID:
21982390.

28. Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013; 471:2492–2496. PMID:
23292888.

29. Bedi A, Dolan M, Hetsroni I, et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med. 2011; 39:43S–49S. PMID:
21709031.
30. Ross JR, Larson CM, Adeoye O, Kelly BT, Bedi A. Residual deformity is the most common reason for revision hip arthroscopy: a three-dimensional CT study. Clin Orthop Relat Res. 2015; 473:1388–1395. PMID:
25475714.

31. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007; 35:1918–1921. PMID:
17703000.

32. Kim C, Nevitt MC, Niu J, et al. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. BMJ. 2015; 351:h5983. PMID:
26631296.

33. Grant AD, Sala DA, Davidovitch RI. The labrum: structure, function, and injury with femoro-acetabular impingement. J Child Orthop. 2012; 6:357–372. PMID:
24082951.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download