Spinal muscular atrophy (SMA) is an autosomal recessive neurodegenerative disease characterized by progressive proximal muscle weakness and atrophy resulting from degeneration of the alpha motor neurons of the anterior horn of the spinal cord. SMA is phenotypically heterogeneous and is classified into four clinical subtypes based on the age of onset and motor function achieved [
1]. Type I SMA presents marked weakness and developmental motor regression before the age of six months and usually results in death within two years. Type II SMA presents before the age of 18 months and is associated with difficulty in walking independently. Type III SMA presents after the age of 18 months and individuals walk independently with only supportive care and is seldom fatal. Type IV SMA presents in the second or third decade of life, with only minor muscle weakness. The incidence of all types of SMA is estimated to be 1 in 10,000 live births globally [
2].
SMA is caused by variants in
SMN1 located on chromosome 5q13.2. Ninety-five percent of SMA patients have homozygous
SMN1 deletions, whereas the remaining 5% have compound heterozygous
SMN1 deletion and point variant. Most patients inherit variants from their parents; only approximately 2% of the affected patients have
de-novo variants [
1]. Although SMA patients lack a functional copy of
SMN1, the nearly identical gene
SMN2, located in the centromeric region of the same chromosome, produces a less functional protein through alternative splicing. The number of
SMN2 copies varies within the general population and is inversely associated with disease severity [
1].
In December 2016, the US Food and Drug Administration approved nusinersen (SPINRAZA™, Biogen, Cambridge, MA, USA), the first effective treatment for SMA (
www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm534611.htm). Nusinersen is a modified antisense oligonucleotide that binds to a specific sequence, including exon 7 of
SMN2 pre-messenger RNA, and increases the production of full-length SMN proteins. Nusinersen treatment in pre-symptomatic infants meaningfully increased the likelihood of survival and improved motor function [
3]. Therefore, it is important to screen for SMA, carrier frequency of SMA, and
SMN2 copy number at an early stage. Methods for SMA screening in newborns or adults have been actively studied and analyzed for cost-effectiveness [
45]. Although the
SMN1 heterozygous deletion carrier frequency reportedly is between 2.00% (95% confidence interval [CI], 0.35–7.74%) and 2.15% (95% CI, 0.94–4.57%) in the Korean population [
67], no large-scale population studies have been performed. Therefore, we conducted a large-scale study to estimate the SMA carrier frequency in Korean newborns. Using the multiplex ligation-dependent probe amplification (MLPA) assay, we assessed the distribution of
SMN1 and
SMN2 copy numbers in umbilical cord blood samples from the newborns.
In total, 1,581 anonymous DNA samples obtained from a public umbilical cord blood bank (Seoul Metropolitan Government Cord Blood Bank, Seoul, Korea) were used. This study protocol was exempted from review by the Institutional Review Board (IRB) of Seoul National University Boramae Hospital, Seoul, Korea (07-2019-17) because the samples have been kept as a repository study under the approval of IRB. All samples were collected from mothers who provided informed consent for donation and research use of their cord blood. The MLPA analysis has been conducted since July 2019.
The MLPA assay was conducted using SALSA MLPA probemix P460-A1 SMA kits (MRC-Holland, Amsterdam, Netherlands), according to the manufacturer's instructions (
https://www.mlpa.com/WebForms/WebFormDBData.aspx?FileOID=_ImdLw-TiaZY.). The PCR products were analyzed using an ABI PRISM 3100 ABI Genetic Analyzer (Applied Biosystems, Foster City, CA, USA). The data were analyzed using GeneMarker software, version 2.6 (Softgenetics, State College, PA, USA). Gene frequencies were calculated with VassarStats (
http://vassarstats.net/), with 95% CI. The Hardy-Weinberg equilibrium was assessed by a professional web-based program (
https://wpcalc.com/en/equilibrium-hardy-weinberg/).
The distribution of
SMN1 and
SMN2 copy numbers in the population is shown in
Fig. 1. Of the 1,581 newborns, 29 (1.83%; 95% CI, 1.25–2.66%) were SMA carriers. Therefore, the carrier frequency in this population was estimated to be 1,834 per 100,000 (95% CI, 1,254–2,659) or 1 in 55 (95% CI, 1/79–1/38). Homozygous
SMN1 deletion was not detected. One newborn was suspected as an
SMN1 silent (2+0) carrier with two
SMN1 copies on one chromosome 5 and deletion on the other [
8]. We also assessed
SMN2 copy numbers in this study population: 63.1% (N=998) had two copies of
SMN2, 29.8% (N=471) had 0 or one copy, and 7.1% (N=112) had three or more copies. Among the SMA carriers, 24.1% (N=7) had 0 or one copy of
SMN2, 58.6% (N=17) had two copies, and 17.2% (N=5) had three or more copies.
In this study, the
SMN1 heterozygous deletion carrier frequency was 1.83–1.90% (including silent carriers), which is similar to or lower than the frequencies reported in the previous Korean studies [
67]; however, in these studies, the CI was wide because of small sample numbers. Given the narrower CI in the current study, the SMA carrier frequency found here might be more accurate. Similar to findings in a previous study, the carrier frequency in our study was higher than that reported for other ethnicities, except Caucasians [
9]. However, it was similar to or lower than that reported for the East Asian population (
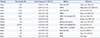
Table 1) [
101112131415161718]. The incidence of SMA caused by
SMN1 homozygous deletion calculated using the Hardy–Weinberg equation was 1/11,815 in Koreans.
According to data from the Korean Statistical Information Service (
http://kosis.kr/; accessed on 17 May 2019), in 2017, the total population of South Korea was 51.42 million, with 357,771 births. Based on the carrier frequency in this study, the number of carriers was estimated to be 0.94 million in total, and 6,547 in newborns per year. Thus, the estimated incidence rate of SMA due to
SMN1 deletion in Korea based on Hardy–Weinberg equilibrium is 30 cases per year.
With the development of drugs for the treatment of SMA, the need for newborn or carrier screening for the early diagnosis of SMA has become important. The US Secretary of Health and Human Services' Advisory Committee on Heritable Disorders in Newborns and Children recommends the addition of SMA screening to default newborn screening programs (
https://www.hrsa.gov/advisory-committees/heritable-disorders/rusp/index.html), and the American College of Medical Genetics and the American College of Obstetricians and Gynecologists recommend routine SMA carrier screening [
1920]. Cost-effectiveness analyses of SMA screening have been reported. Little, et al. [
4] reported that although universal prenatal screening for SMA is not cost-effective, screening of high-risk populations, such as those with a family history, may be. Zhang, et al. [
5] reported that while SMA-only preconception carrier screening is not cost-effective, a combination screen for other conditions, such as cystic fibrosis and fragile X syndrome may prove to be and may prevent up to 30 SMA patients per million (all adults between the ages of 18 and 25 in the Australian health care system). Since the approval of nusinersen, there has been a lack of cost-effective analyses for newborn or carrier screening of SMA. Therefore, large-scale prospective newborn or carrier screening studies are needed for predicting the efficacy of nusinersen treatment.
Our study had some limitations. First, while 5% of SMA patients are known to have
SMN1 missense variant, the MLPA assay is not a suitable method for detecting missense variants. Second, we experienced difficulties in identifying silent carrier phenotypes (e.g.,
SMN1 ‘2+0’ genotype) due to limitations of the MLPA method. Therefore, the SMA carrier frequency might be underestimated. This study also had various advantages. This is the first large-scale population study on the SMA carrier frequency in Koreans conducted using samples from a public umbilical cord blood bank. Further, because the CI used herein was narrower than that reported in previous studies [
67], the SMA carrier frequency and incidence predicted here might be more accurate. Finally, we evaluated the distribution of
SMN2 copy number in the general Korean population, which is important for predicting both the prognosis of patients with SMA and the efficacy of nusinersen treatment.
Our data indicate that carriers of SMN1 heterozygous deletion are not uncommon in the general Korean population. The carrier frequency was similar to or lower than that in the East Asian population and higher than that in other ethnicities. To our knowledge, this is the largest cohort study of SMN1 and SMN2 copy numbers in the Korean population to date, and our data are expected to serve as a reference for further investigation of SMA in the Korean population.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download