1. Yalççn S, Oncü B, Emes Y, Atalay B, Aktaş I. Surgical treatment of oroantral fistulas: a clinical study of 23 cases. J Oral Maxillofac Surg. 2011; 69:333–339. PMID:
21145640.
2. Visscher SH, van Minnen B, Bos RR. Closure of oroantral communications: a review of the literature. J Oral Maxillofac Surg. 2010; 68:1384–1391. PMID:
20227153.

3. Parvini P, Obreja K, Sader R, Becker J, Schwarz F, Salti L. Surgical options in oroantral fistula management: a narrative review. Int J Implant Dent. 2018; 4:40. PMID:
30588578.

4. Dym H, Wolf JC. Oroantral communication. Oral Maxillofac Surg Clin North Am. 2012; 24:239–247. viii–ix. PMID:
22503070.

5. Hernando J, Gallego L, Junquera L, Villarreal P. Oroantral communications. A retrospective analysis. Med Oral Patol Oral Cir Bucal. 2010; 15:e499–e503. PMID:
20038901.

6. Rehrmann A. [Eine methode zur schliessung von kieferhöhlenperforationen]. Dtsch Zahnärztl Wschr. 1936; 39:1136–1138. German.
7. Killey HC, Kay LW. Observations based on the surgical closure of 362 oro-antral fistulas. Int Surg. 1972; 57:545–549. PMID:
5042434.
8. von Wowern N. Closure of oroantral fistula with buccal flap: Rehrmann versus Môczár. Int J Oral Surg. 1982; 11:156–165. PMID:
6813275.

9. Haanaes HR, Pedersen KN. Treatment of oroantral communication. Int J Oral Surg. 1974; 3:124–132. PMID:
4209425.

10. Martín-Granizo R, Naval L, Costas A, Goizueta C, Rodriguez F, Monje F, et al. Use of buccal fat pad to repair intraoral defects: review of 30 cases. Br J Oral Maxillofac Surg. 1997; 35:81–84. PMID:
9146863.

11. el-Hakim IE, el-Fakharany AM. The use of the pedicled buccal fat pad (BFP) and palatal rotating flaps in closure of oroantral communication and palatal defects. J Laryngol Otol. 1999; 113:834–838. PMID:
10664688.

12. Rapidis AD, Alexandridis CA, Eleftheriadis E, Angelopoulos AP. The use of the buccal fat pad for reconstruction of oral defects: review of the literature and report of 15 cases. J Oral Maxillofac Surg. 2000; 58:158–163. PMID:
10670594.

13. Egyedi P. Utilization of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J Maxillofac Surg. 1977; 5:241–244. PMID:
338848.

14. Arce K. Buccal fat pad in maxillary reconstruction. Atlas Oral Maxillofac Surg Clin North Am. 2007; 15:23–32. PMID:
17434059.

15. Stajcić Z. The buccal fat pad in the closure of oro-antral communications: a study of 56 cases. J Craniomaxillofac Surg. 1992; 20:193–197. PMID:
1401089.
16. Baumann A, Ewers R. Application of the buccal fat pad in oral reconstruction. J Oral Maxillofac Surg. 2000; 58:389–392. discussion 392–3. PMID:
10759118.

17. Yang S, Jee YJ, Ryu DM. Reconstruction of large oroantral defects using a pedicled buccal fat pad. Maxillofac Plast Reconstr Surg. 2018; 40:7. PMID:
29637060.

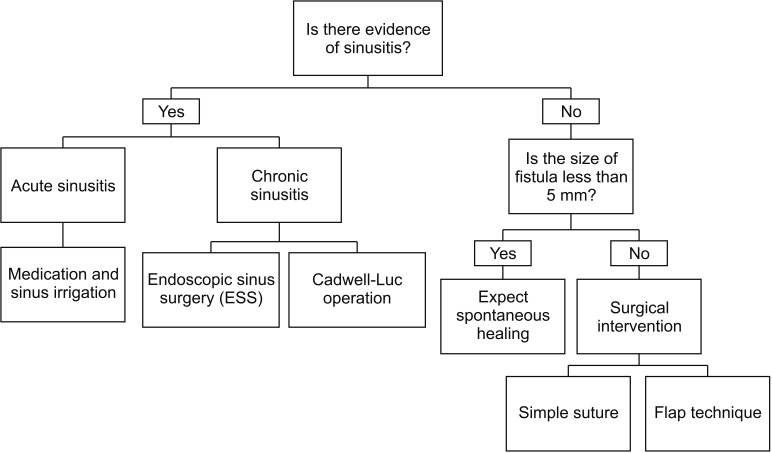
18. Parvini P, Obreja K, Begic A, Schwarz F, Becker J, Sader R, et al. Decision-making in closure of oroantral communication and fistula. Int J Implant Dent. 2019; 5:13. PMID:
30931487.

19. Paterson C, Thomson MC, Caldwell B, Young R, McLean A, Porteous S, et al. Radiotherapy-induced xerostomia: a randomised, double-blind, controlled trial of Visco-ease™ oral spray compared with placebo in patients with cancer of the head and neck. Br J Oral Maxillofac Surg. 2019; 57:1119–1125. PMID:
31672256.

20. Dirix P, Nuyts S, Van den Bogaert W. Radiation-induced xerostomia in patients with head and neck cancer: a literature review. Cancer. 2006; 107:2525–2534. PMID:
17078052.
21. Dirix P, Nuyts S, Vander Poorten V, Delaere P, Van den Bogaert W. The influence of xerostomia after radiotherapy on quality of life: results of a questionnaire in head and neck cancer. Support Care Cancer. 2008; 16:171–179. PMID:
17618467.
22. Vissink A, Mitchell JB, Baum BJ, Limesand KH, Jensen SB, Fox PC, et al. Clinical management of salivary gland hypofunction and xerostomia in head-and-neck cancer patients: successes and barriers. Int J Radiat Oncol Biol Phys. 2010; 78:983–991. PMID:
20970030.

23. Tideman H, Bosanquet A, Scott J. Use of the buccal fat pad as a pedicled graft. J Oral Maxillofac Surg. 1986; 44:435–440. PMID:
3457926.

24. Wells DL, Capes JO. Complications of dentoalveolar surgery. In : Fonseca RJ, editor. Oral and maxillofacial surgery. Philadelphia: WB Saunders;2000. p. 432.
25. Ehrl PA. Oroantral communication. Epicritical study of 175 patients, with special concern to secondary operative closure. Int J Oral Surg. 1980; 9:351–358. PMID:
6783559.
26. Anavi Y, Gal G, Silfen R, Calderon S. Palatal rotation-advancement flap for delayed repair of oroantral fistula: a retrospective evaluation of 63 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 96:527–534. PMID:
14600685.

27. Jamali JA. Palatal flap. Oral Maxillofac Surg Clin North Am. 2014; 26:305–311. PMID:
25086692.

28. Ward BB. The palatal flap. Oral Maxillofac Surg Clin North Am. 2003; 15:467–473. vPMID:
18088697.

29. Hong SO, Shim GJ, Kwon YD. Novel approach to the maxillary sinusitis after sinus graft. Maxillofac Plast Reconstr Surg. 2017; 39:18. PMID:
28695114.

30. Er N, Tuncer HY, Karaca C, Copuroğlu S. Treatment of oroantral fistulas using bony press-fit technique. J Oral Maxillofac Surg. 2013; 71:659–666. PMID:
23507319.

31. Lin GH, Chan HL, Wang HL. The significance of keratinized mucosa on implant health: a systematic review. J Periodontol. 2013; 84:1755–1767. PMID:
23451989.

32. Brito C, Tenenbaum HC, Wong BK, Schmitt C, Nogueira-Filho G. Is keratinized mucosa indispensable to maintain peri-implant health? A systematic review of the literature. J Biomed Mater Res B Appl Biomater. 2014; 102:643–650. PMID:
24124021.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download