This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The need for proper wound closure is of paramount importance after any intra-oral surgery. Various wound closure techniques have been described in literature using traditional non-absorbable suture materials. These include like synthetic absorbable sutures, surgical staples and tissue adhesives. Cyanoacrylates are among the most commonly used biocompatible tissue adhesives. To evaluate and compare intraoral wound healing using 3-0 silk sutures and n-butyl-2-cyanoacrylate after alveoloplasty.
Materials and Methods
A total of 20 patients requiring bilateral alveoloplasty in the same arch (upper or lower) were included in this study. Patients with any pre-existing pathology or systemic disease were excluded. After alveoloplasty was performed, the wound was closed using 3-0 braided silk sutures on one side, and using n-butyl-2-cyanoacrylate bio adhesive on the other side. Patients were evaluated based on the following parameters: time required to achieve wound closure; the incidence of immediate and postoperative hemostasis; the time to the use of the first rescue medication; the side where pain first arises; and the side where wound healing begins first.
Results
Compared to 3-0 silk sutures, cyanoacrylate demonstrated better hemostatic properties, reduced operative time, reduced postoperative pain and better wound healing.
Conclusion
These data suggest that cyanoacrylate glue is an adequate alternative to conventional sutures to close the surgical wound after alveoloplasty, and better than are 3-0 silk sutures.
Go to :

Keywords: Alveoloplasty, Cyanoacrylate, N-butyl-2-cyanoacrylate, Tissue adhesive, Silk
I. Introduction
The need for appropriate wound closure after any intraoral surgical procedure has always been a topic of concern. Dating back for thousands of years, there have been countless techniques used for closing surgical wounds. Regardless of the technique, the basic goals of surgical closure remain the same. These include reducing the dead space, minimizing risk of infection and properly approximating the wound edges to achieve an acceptable aesthetic and functional outcome.
Various wound closure techniques have been described in literature using traditional non-absorbable suture materials and advanced modalities, such as synthetic absorbable sutures, surgical staples and tissue adhesives.
Suturing has traditionally been the conventional method for approximating wound margins. However, suturing may cause permanent suture tracks, wound dehiscence, needle prick injuries, foreign body reactions, granulations, tissue ischemia, tissue tearing and infection
1. Various alternative materials have been used for approximating wounds since ancient times, ranging from human hair to silk sutures. Although the modern suture materials and techniques are very sophisticated, the intended wound closure still may not be achieved
2. Therefore, there is a need for alternative closure options.
This need led to an interest in tissue adhesives as substitutes for sutures to close surgical wounds. Previously ethyl and methyl cyanoacrylate were used for wound closure; however, they were discarded given their potential toxicities
3. Newer generation cyanoacrylate includes n-butyl-2-cyanoacrylate, octyl-2-cyanoacrylate, and isoamyl 2-cyanoacrylate.
N-butyl-2-cyanoacrylate has unique properties, including faster tissue bonding capacity and curing compared to those of octyl cyanoacrylate and iso-amyl 2-cyanoacrylate. In addition, its excellent tensile strength, fast polymerization, biocompatibility, immediate hemostasis, ease of application, and bacteriostatic properties make it a good choice to close surgical wounds. Given the superior properties that n-butyl-2-cyanoacrylate has in comparison to those of other cyanoacrylates, it may also be better for wound healing. Therefore, we believe there is a need to clinically evaluate its role in intra-oral wound closure.
Setiya et al.
4 evaluated the efficacy, advantages and disadvantages of cyanoacrylate glue for sutureless wound closure after surgical removal of impacted mandibular third molars. This study was performed on 50 patients with bilateral, symmetrically impacted third molars. Their analysis showed that there was significantly less postoperative pain, bleeding and swelling when cyanoacrylate was used for closure than there was with suturing. The use of cyanoacrylate also showed better hemostasis than did traditional suturing. However, healing was similar in both groups.
Alveoloplasty is a routine dental procedure that is associated with swelling, bleeding, and pain postoperatively. These types of surgical wounds are conventionally closed using resorbable or non-resorbable sutures and are allowed to heal by primary intention. However, suture can be challenging in this area due to inaccessibility. Suturing is time consuming, and requires adequate skill. At times, resorbable sutures must be removed early because they can be lodged with food and be irritating to the patient. Besides these difficulties, suturing also requires an additional visit for suture removal. In order to overcome these disadvantages, Besides these difficulties, suturing also requires an additional visit for suture removal. In order to overcome these disadvantages, the use of tissue adhesives (cyanoacrylate) in surgical procedures have been described in literature
1456789.
In our study, we compare wound healing after alveoloplasty using silk and n-butyl-2-cyanoacrylate for surgical closure in 20 patients. We also compare the time to closure, hemostasis, and pain postoperatively. Finally, we compared wound healing between the two closure methods.
Go to :

II. Materials and Methods
This prospective, randomized, an in vivo study was carried out from January 2016 to June 2017 in the Department of Oral and Maxillofacial Surgery at Dr. D. Y. Patil Dental College & Hospital, Pimpri, Pune, India. The study was approved by the Ethics Committee of Dr. D. Y. Patil Dental College & Hospital (No. DYPDCH/760/2015/34). Twenty patients (4 females and 16 males) were included in this split mouth clinical study. Each patient underwent alveoloplasty under local anesthesia. Closure was achieved using either 3-0 black braided silk sutures or with n-butyl-2-cyanoacrylate bio adhesive (Endocryl; Samarth Life Sciences Pvt. Ltd., Mumbai, India). The parameter data were noted, tabulated and analyzed using the unpaired t-test and chi-square test.
Inclusion criteria were (1) patients with bilateral edentulous arches (both in the upper or lower arch) requiring alveoloplasty and (2) patients willing to participate in the study. Exclusion criteria included (1) patients with any pre-existing pathology and (2) patients with systemic diseases such as diabetes or anemia.
A detailed and thorough medical history was obtained from the patient, followed by meticulous physical examination. Valid written informed consent for the surgical procedure was obtained from each patient.
Investigations were included hemogram, bleeding time, clotting time, and blood sugar level.
Twenty patients who required alveoloplasty (and fulfilled the above mentioned criteria) were selected. All of the patients were informed about the procedure and the purpose, advantages and disadvantages of the study. The following preoperative laboratory tests were performed: hemogram, bleeding time, clotting time, and blood sugar level. Valid informed written consent was obtained from every patient. An equal volume of 2% lidocaine with 1:200,000 adrenaline was administered on each side. After administrating the local anesthetic agent, a coin toss method was used to select which side would be treated with cyanoacrylate and which with sutures. In the selected subjects, the surgical sites were divided into two treatment groups. Group 1 included wounds that would be closed with 3-0 braided silk sutures (Mersilk; Ethicon, Johnson & Johnson Pvt. Ltd., Himachal Pradesh, India). Group 2 included wounds that would be closed using n-butyl-2-cyanoacrylate bio adhesive (Endocryl). A crestal incision with anterior release was made in all cases to expose the bony spicules. A triangular mucoperiosteal flap was raised. Bony projections were smoothened using a bone file or rongeur forcep. The wound was irrigated with saline.
Hemostasis was achieved. Hemostatic agents, such as collagen plugs or electrocautery, were not used during alveoloplasty. Wound closure was performed using either 3-0 silk or Endocryl. The following medications were given postoperatively to all patients after wound closure:
• Cap. amoxicillin 500 mg capsule three times daily for 5 days after the procedure.
• Tab. diclofenac sodium (50 mg, Voveran; Novartis India, Mumbai, India) twice daily for 5 days (rescue medication).
• Tab. ranitidine 150 mg (Rantac; JB Chemicals & Pharmaceuticals, Pune, India) twice daily for 5 days to any patients with gastric irritation.
Postoperatively, patients were also given chlorhexidine mouthwash 0.12% (Perioguard; Colgate-Palmolive India, Mumbai, India) and instructed to rinse three times per day for 7 days.
The following postoperative parameters were used to evaluate the study subjects: (1) time to achieve wound closure, (2) incidence of immediate and postoperative hemostasis, (3) time to use of rescue medication was noted, (4) the side where pain first arises, (5) wound healing according to the Landry, Turnbull, and Howley index
10, and (6) patient evaluation on the 1st and 7th postoperative days.
These values were recorded, tabulated and statistically evaluated.(
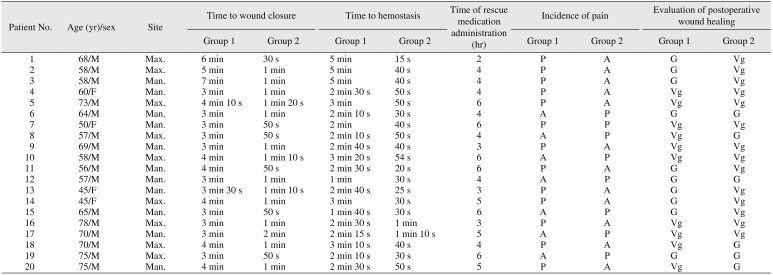
Table 1)
Table 1
Patient distribution and evaluation data
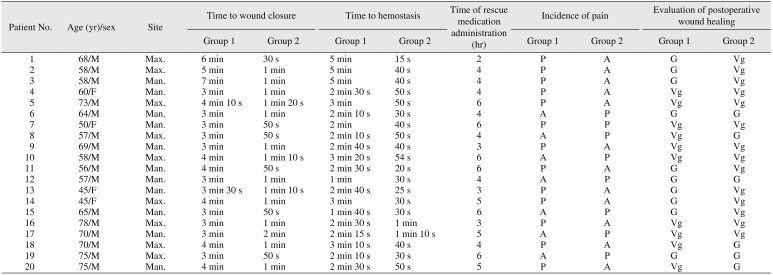
|
Patient No. |
Age (yr)/sex |
Site |
Time to wound closure |
Time to hemostasis |
Time of rescue medication administration (hr) |
Incidence of pain |
Evaluation of postoperative wound healing |
|
Group 1 |
Group 2 |
Group 1 |
Group 2 |
Group 1 |
Group 2 |
Group 1 |
Group 2 |
|
1 |
68/M |
Max. |
6 min |
30 s |
5 min |
15 s |
2 |
P |
A |
G |
Vg |
|
2 |
58/M |
Max. |
5 min |
1 min |
5 min |
40 s |
4 |
P |
A |
G |
Vg |
|
3 |
58/M |
Man. |
7 min |
1 min |
5 min |
40 s |
4 |
P |
A |
G |
Vg |
|
4 |
60/F |
Man. |
3 min |
1 min |
2 min 30 s |
50 s |
4 |
P |
A |
Vg |
Vg |
|
5 |
73/M |
Max. |
4 min 10 s |
1 min 20 s |
3 min |
50 s |
6 |
P |
A |
Vg |
Vg |
|
6 |
64/M |
Man. |
3 min |
1 min |
2 min 10 s |
30 s |
4 |
A |
P |
G |
G |
|
7 |
50/F |
Man. |
3 min |
50 s |
2 min |
40 s |
6 |
P |
P |
Vg |
Vg |
|
8 |
57/M |
Max. |
3 min |
50 s |
2 min 10 s |
50 s |
4 |
A |
P |
Vg |
G |
|
9 |
69/M |
Man. |
3 min |
1 min |
2 min 40 s |
40 s |
3 |
P |
A |
Vg |
Vg |
|
10 |
58/M |
Max. |
4 min |
1 min 10 s |
3 min 20 s |
54 s |
6 |
A |
P |
Vg |
Vg |
|
11 |
56/M |
Man. |
4 min |
50 s |
2 min 30 s |
20 s |
6 |
P |
A |
G |
Vg |
|
12 |
57/M |
Man. |
3 min |
1 min |
1 min |
30 s |
4 |
A |
P |
G |
G |
|
13 |
45/F |
Man. |
3 min 30 s |
1 min 10 s |
2 min 40 s |
25 s |
3 |
P |
A |
G |
Vg |
|
14 |
45/F |
Max. |
4 min |
1 min |
3 min |
30 s |
5 |
P |
A |
G |
Vg |
|
15 |
65/M |
Man. |
3 min |
50 s |
1 min 40 s |
30 s |
6 |
A |
P |
G |
Vg |
|
16 |
78/M |
Max. |
3 min |
1 min |
2 min 30 s |
1 min |
3 |
P |
A |
Vg |
Vg |
|
17 |
70/M |
Man. |
3 min |
2 min |
2 min 15 s |
1 min 10 s |
5 |
A |
P |
Vg |
Vg |
|
18 |
70/M |
Max. |
4 min |
1 min |
3 min 10 s |
40 s |
4 |
P |
A |
Vg |
G |
|
19 |
75/M |
Max. |
3 min |
50 s |
2 min 10 s |
30 s |
6 |
A |
P |
G |
G |
|
20 |
75/M |
Man. |
4 min |
1 min |
2 min 30 s |
50 s |
5 |
P |
A |
Vg |
G |

Go to :

III. Results
The data were compiled as shown in
Table 1. The data were analyzed using the IBM SPSS Statistics (ver. 22.0; IBM, Armonk, NY, USA). A
P-value less than 0.05 was considered statistically significant.
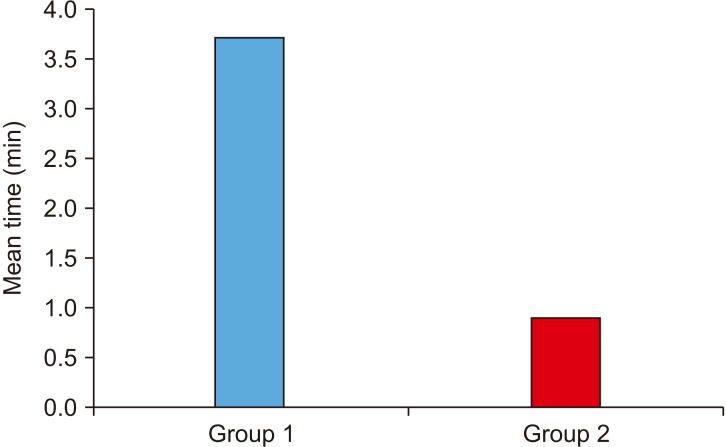
The mean time to wound closure in Group 1 was 3.77±1.11 minutes and 0.91±0.37 minutes in Group 2 with a mean difference of 2.86 minutes (T=10.917,
P<0.001).(
Table 2,
Fig. 1)
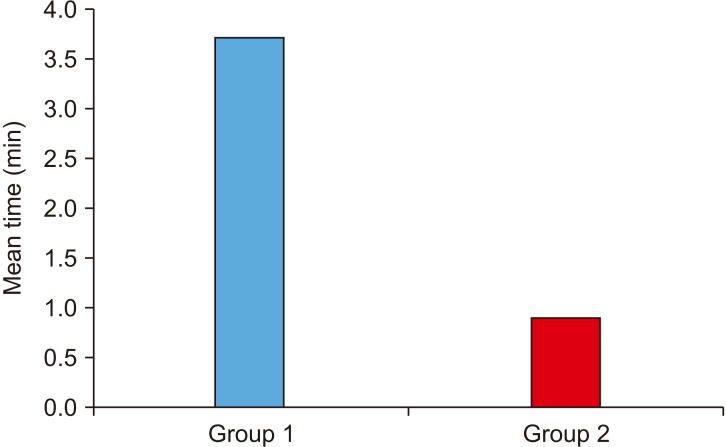 | Fig. 1Comparing the time to achieve wound closure. (Group 1: using silk sutures, Group 2: using n-butyl-2-cyanoacrylate)
|
Table 2
Comparing the time to achieve wound closure

|
Group |
No. of patients |
Mean |
SD |
T |
P-value |
Mean difference |
|
Time to wound closure (min) |
1 |
20 |
3.770 |
1.1108 |
10.917 |
<0.001*
|
2.8600 |
|
2 |
20 |
0.910 |
0.3726 |

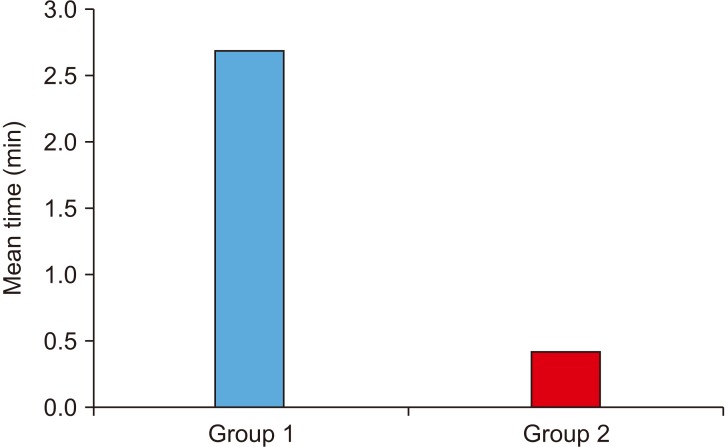
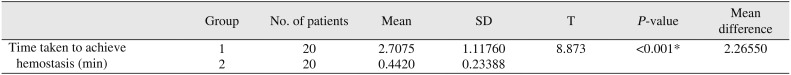
The mean time to achieve hemostasis in Group 1 was 2.71±1.11 minutes and 0.44±0.23 minutes in Group 2 with a mean difference of 2.26 minutes (T=8.873,
P<0.001).(
Table 3,
Fig. 2)
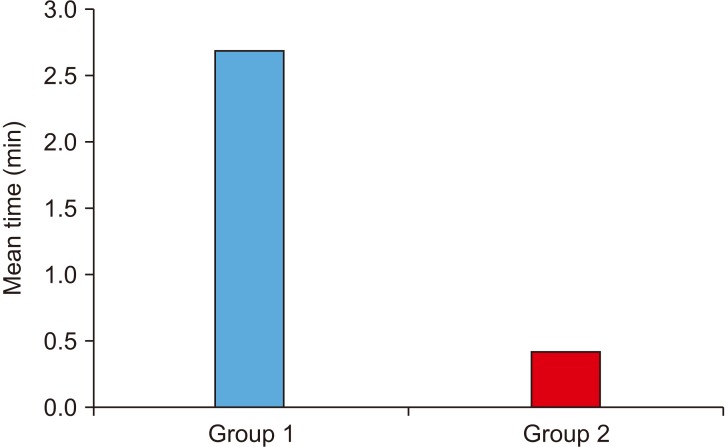 | Fig. 2Comparing the time to achieve hemostasis. (Group 1: using silk sutures, Group 2: using n-butyl-2-cyanoacrylate)
|
Table 3
Comparing the time to achieve hemostasis
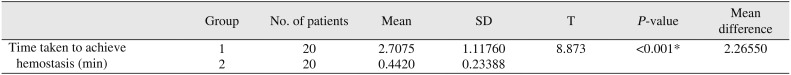
|
Group |
No. of patients |
Mean |
SD |
T |
P-value |
Mean difference |
|
Time taken to achieve hemostasis (min) |
1 |
20 |
2.7075 |
1.11760 |
8.873 |
<0.001*
|
2.26550 |
|
2 |
20 |
0.4420 |
0.23388 |

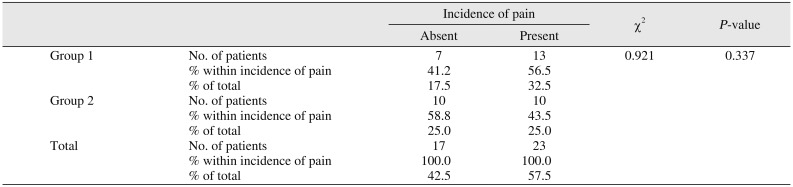
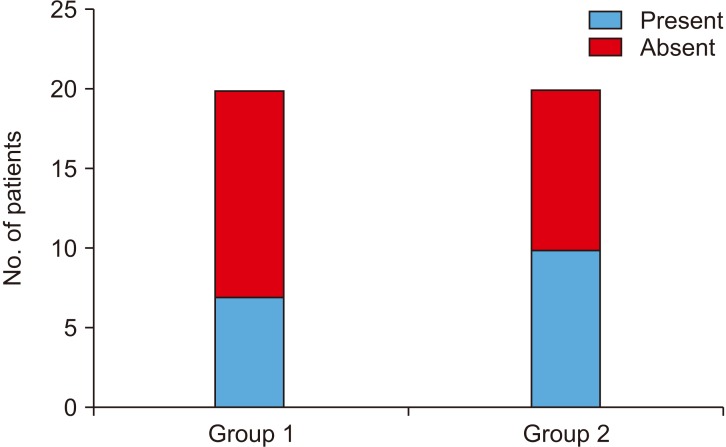
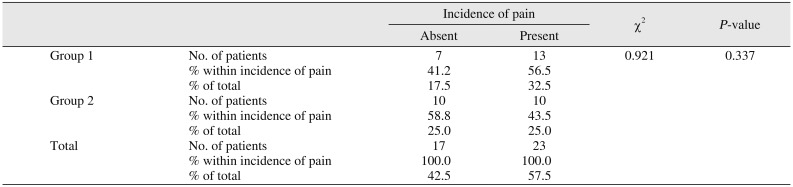
The percentage of patients without pain was 41.2% in Group 1 and 58.8% in Group 2. The incidence of pain, in contrast, was 56.5% in Group 1 and 43.5% in Group 2 (χ
2=0.921,
P=0.337).(
Table 4,
Fig. 3)
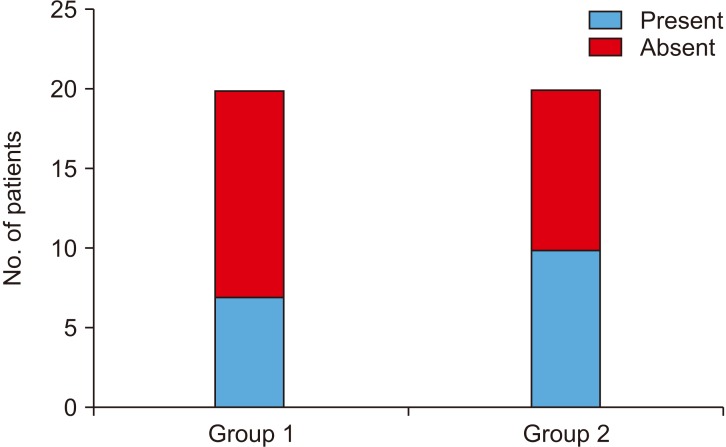 | Fig. 3Comparing postoperative pain between groups. (Group 1: using silk sutures, Group 2: using n-butyl-2-cyanoacrylate)
|
Table 4
Comparing postoperative pain between groups
|
Incidence of pain |
χ2
|
P-value |
|
Absent |
Present |
|
Group 1 |
No. of patients |
7 |
13 |
0.921 |
0.337 |
|
% within incidence of pain |
41.2 |
56.5 |
|
% of total |
17.5 |
32.5 |
|
Group 2 |
No. of patients |
10 |
10 |
|
|
|
% within incidence of pain |
58.8 |
43.5 |
|
% of total |
25.0 |
25.0 |
|
Total |
No. of patients |
17 |
23 |
|
|
|
% within incidence of pain |
100.0 |
100.0 |
|
% of total |
42.5 |
57.5 |

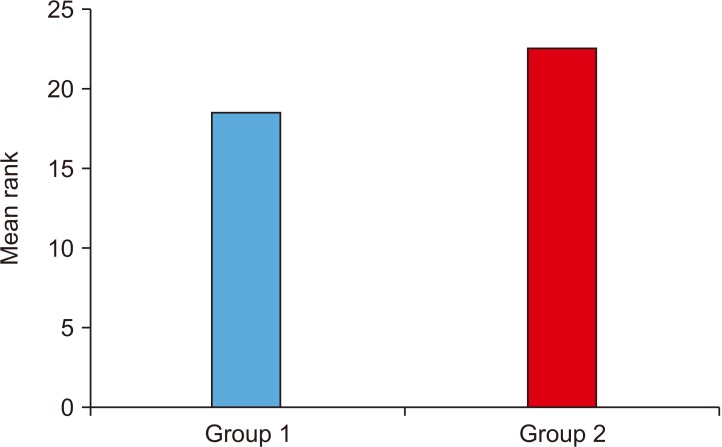
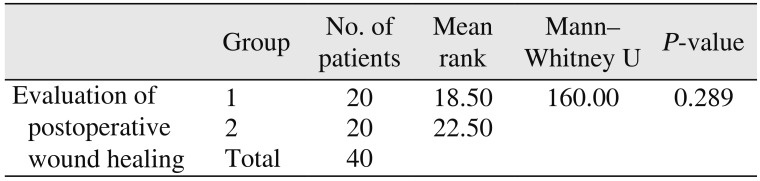
The mean rank value of postoperative wound healing was 18.50 in Group 1 and 22.50 in Group 2 (Mann–Whitney U value=160.00,
P=0.289).(
Table 5,
Fig. 4)
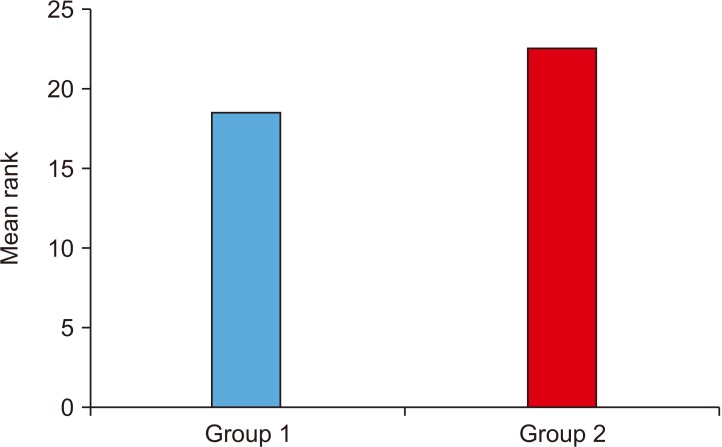 | Fig. 4Comparing postoperative wound healing. (Group 1: using silk sutures, Group 2: using n-butyl-2-cyanoacrylate)
|
Table 5
Comparing postoperative wound healing between groups
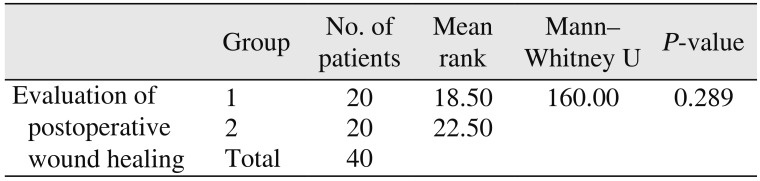
|
Group |
No. of patients |
Mean rank |
Mann–Whitney U |
P-value |
|
Evaluation of postoperative wound healing |
1 |
20 |
18.5 |
160 |
0.289 |
|
2 |
20 |
22.5 |
|
|
|
Total |
40 |
|
|
|

Go to :

IV. Discussion
The principles of wound closure emphasize re-establishing functional soft tissue structural support, reducing wound tension and achieving everted skin edges. Precise approximation of wound margins and proper wound closure produces the most natural esthetic appearance and minimizes the need for later scar revision
3.
A variety of materials have been used for wound closure, including metal clips (staples), adhesive tapes and sutures. Metal clips pose a greater risk for crosshatch marking and less precise wound approximation compared to those of other materials
11. Adhesive tapes are used for wounds that are small, non-exudative and under minimal tension. These tapes can limit wound eversion and may have inconsistent adhesion. Sutures are the most commonly used wound closure materials. They are foreign materials that are woven through the skin and left in place for 5 to 10 days. Sutures that are tied too tight or left for too long can lead to the formation of suture tracks. Patients may also develop suture anxiety, which can lead to significant discomfort on their removal
3.
In order to maximize adhesion and minimize patient discomfort, surgeons and physicians have proposed the use of tissue adhesives as a substitute for sutures in wound closure. Cyanoacrylates are one of the most commonly used tissue adhesives. Various Gelatin derivatives, such as Epoxide, Polyurethane and Resorcin, have been investigated for their use as tissue adhesives in surgery. Cyanoacrylates have gained wider acceptability and achieved a better outcome than have the gelatin derivatives. For the past 50 years, polymer adhesives have been used in medical and dental practice. One major drawback of polymers is that they are not tissue compatible, and may produce an extensive inflammatory reaction
3.
By the early 1970s, cyanoacrylate glue was being used for mending bone, hide and tortoise shell. In the Vietnam War (1996) cyanoacrylate spray was used for hemostasis in wounded soldiers. Adhesives like n-butyl cyanoacrylate not only required less time for wound closure than did traditional methods, but also reduced the prevalence of infection and improved esthetics. The early short-chain tissue adhesives were effective but had limited use because they underwent rapid degradation into byproducts that had significant tissue toxicity. However, longer-chain cyanoacrylates degrade slowly, which limits the accumulation of toxic by-products in the tissues and makes them safe for topical skin closure. Therefore, in 1998, the U.S. Food and Drug Administration approved the use of the first topical skin adhesive. The following three cyanoarylate compounds are now used as topical skin adhesives: 2-octyl-cyanoacrylate (Dermabond and SurgiSeal), n-2-butylcyanoacrylate (Endocryl, Histocryl, Indermil, GluStitch, Peri-Acryl, and LiquiBand) and 2-ethyl-cyanoacrylate (Epiglu).
Cyanoacrylate adhesives have a short shelf life and are moisture sensitive. The shelf life of cyanoacrylate can be extended from about one year to 15 months after manufacturing if they are kept unopened in a cool, dry area (such as a refrigerator at 55°F or 13℃). If the adhesive is used within six months from the time of manufacturing, there is no need to refrigerate it. Similarly, open containers should not be refrigerated. Moving cyanoacrylate from a cool to a hot location can create condensation. In order to such condensation, the adhesive is allowed to reach room temperature before it is opened.
N-butyl 2-cyanoacrylates are biocompatible tissue adhesives that possess favorable properties, such as adequate flow and fast setting. They also have strong bonding properties and strength to hold tissue margins together. Valence bond and van der Waals force help in achieving tissue adhesion. After n-butyl-2-cyanoacrylate is applied, it forms a firm adhesive bond through exothermic polymerization with water, tissue moisture or blood. Cyanoacrylates are exothermic; therefore, heat is released by the polymerization reaction. They are also bacteriostatic. Wound sites that are closed with n-butyl-2-cyanoacrylate have also shown reduced postoperative pain than those closed with other methods. Finally, cyanoacrylates are good hemostatic agents
1.
However the exact mechanism by which n-butyl-2-cyanoacrylate achieves hemostasis is unclear. One hypothesis states that the formation of a macrofilm by the ester causes mechanical blockage, which slows blood flow and provides a surface agent to activate the coagulation cascade. Evidence shows that the macrofilm forms a porous mass that is invaded by blood, and there is subsequent clotting within the pores of the adhesive
3.
Cyanoacrylates offer various advantages, such as: effective and immediate hemostasis, ease of application, bacteriostatic properties, rapid adhesion to hard and soft tissues, maximum bonding strength and water resistant covering. They have a wide range of applications in surgery, as follows: repairing organs, vessels, skin and mucosal grafts; closing lacerations and incisions; dressing post-extraction wounds; and fixing mandibular fractures
3.
In the field of maxillofacial surgery, wound closure using cyanoacrylates has been achieved in multiple settings, including extraction sockets, face, sinus perforations in sinus lift, biopsies, superficial oral ulcerations, gingivectomy, mucogingival flaps, and recurrent multiple aphthous ulcers
461213. Its use in general surgery is also prevalent in for wounds in the axilla, lungs
4613, heart and scalp
61114. It is also used as a hemostatic agent to control bleeding from skin grafts
4111516, brow lifts, cosmetic surgeries
4617 and various anastomoses of intestines, arteries and nerves
4617.
In this study, 16 of the 20 patients were male and 4 were female ranging in age from 50 to 78 years (mean, 64 years). A single surgeon performed bilateral alveoloplasty in all of these patients, and performed the final closure using silk on one side and n-butyl-2-cyanoacrylate on the other. The time taken for closure using silk sutures ranged between 3 to 7 minutes. In contrast, the time for closure using n-butyl-2-cyanoacrylate ranged from only 30 to 2 minutes. Hemostasis using n-butyl-2-cyanoacrylate was achieved in <1.5 minutes, while it took up to 5 minutes to achieve hemostasis using silk sutures. The time to the use of rescue medications ranged from 2 to 6 hours. Six patients had pain on the side where nbutyl-2-cyanoacrylate was used, while 13 patients had pain on the side where silk sutures were placed. One patient presented with pain on both sides. This pain may be attributable to inadequate tissue coaptation between the wound edges, leading to inadvertent cyanoacrylate flow. This impaired flow might lead to collection of food debris, tissue irritation, inflammation and pain. Ten patients showed no significant differences in postoperative healing, while seven patients showed better wound healing with n-butyl-2-cyanoacrylate. Three patients showed better wound healing with silk sutures.
Go to :

V. Conclusion
Cyanoacrylate glue can be used for wound closure after alveoloplasty. We found that glue has better hemostatic properties, reduces operative time and postoperative pain and swelling compared to those of silk suturing. The glue also enabled better wound healing than did suturing.
This procedure was also agreeable to the surgeon. Since the material is bacteriostatic, it offers protection against wound infection. The use of cyanoacrylate had several advantages, such as simplicity, higher speed and better hemostasis properties over those of suturing. It also does not require a second visit for suture removal. The cost of the adhesive was the only limitation to its use. Further prospective studies are needed to substantiate these results, and to assess the overall cost effectiveness of tissue adhesives compared to surgical sutures in low-tension elective procedures. Regardless, our findings suggest that cyanoacrylate glue is a better alternative to conventional suturing for wound closure after alveoloplasty.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download