I. Introduction
Pentoxifylline [1-(5-oxohexyl)-3,7-dimethylxanthine, PTX] is a methylxanthine derivative
1 that has been implicated in the pathogenesis of peripheral vessel disease and intermittent lameness
2. PTX is a non-selective inhibitor of cyclic nucleotide phosphodiesterase (PDE) that inhibits cyclic adenosine monophosphate (cAMP) PDE, increases cAMP and adenosine-5′-triphosphate in erythrocytes, and increases red blood cell deformability. PTX decreases leukocyte adhesion to endothelial cells, increases prostacyclin production, and inhibits platelet aggregation. These effects induce capillary dilatation, reduce blood viscosity, and improve peripheral blood flow
3. Recently, PTX has been shown to exhibit immunomodulatory functions to downregulate the production of proinflammatory cytokines, particularly tumor necrosis factor alpha (TNF-α)
4.
Tocopherols are a class of organic chemical compounds consisting of various methylated phenols. These compounds possess antioxidant effects to protect cell membranes from lipid peroxidation and are known to partially inhibit transforming growth factor-β1. Tocopherols also reduce inflammation and tissue fibrosis. The combination of PTX and tocopherol has synergistic effects, but the mechanism of action remains unclear
5.
The effects of PTX and tocopherol have been reported to be encouraging in the treatment of osteoradionecrosis (ORN)
67. There are some reports that the combination of PTX and tocopherol is effective against bisphosphonate-related osteonecrosis of the jaw (BRONJ).
ORN, BRONJ, and chronic osteomyelitis have similar clinical characteristics, yet are different in pathophysiology. The three disease entities are clinically similar and may represent oral bone exposure that cannot be cured within an 8-week period
8. Various classification systems have been proposed for these disease entities. In the staging of osteomyelitis, Notani's classification of ORN was used in this study. In a panorama image, stage I is defined as lesions restricted to the alveolar bone, stage II is defined as lesions restricted to the alveolar bone and/or above the inferior alveolar canal, while stage III was defined as the invasion to the lower part of the inferior alveolar canal, extraoral fistulae, or pathologic bone fracture
9. BRONJ patients are defined as those with a history of treatment with bisphosphonates, bone exposure for eight weeks or longer, and no history of radiation therapy (RT) or evidence of metastatic disease to the jaws
10. Patients without a history of RT or antiresorptive drugs such as bisphosphonates were classified as chronic osteomyelitis. The BRONJ group was classified according to the BRONJ staging system with 2014 American Association of Oral and Maxillofacial Surgeons (AAOMS) guidelines
1011.
Basic images involve periapicals and panoramas. Computed tomography creates three dimensional images and accurately shows the extension of lesions. Panoramic radiographs are routinely performed during diagnosis and follow-up and allow for easy comparisons of bony changes following treatment. In this study, the effects of PTX and tocopherol were evaluated by serial panoramic analysis of patients diagnosed with ORN, BRONJ, or chronic osteomyelitis in jaw.
Go to :

II. Materials and Methods
We retrospectively analyzed 25 patients who were prescribed PTX and tocopherol for treatment of ORN, BRONJ, or chronic osteomyelitis of the mandible between January 2014 and May 2018 in Seoul National University Dental Hospital. All patients received a combination of 800 mg of PTX and 800 IU of vitamin E every day. The PTX dosage was designed to avoid severe adverse effects in patients without vascular disease, while the vitamin E dosage was determined to supply sufficient antioxidant activity. There were no serious side effects during the study period. All patients were divided into two groups: PTX and tocopherol for less than 90 days (short-term), and group for more than 90 days (long-term). While the effect of PTX may be seen within 2 to 4 weeks, it is recommended that treatment be continued at least 8 weeks
12.
We evaluated serial dental panoramas using Adobe Photoshop CS6 (Adobe System Inc., San Jose, CA, USA). The Orthopantomograph OP100 (Instrumentaruim Corp., Helsinki, Finland) was used for panoramic radiographs. By setting the region of interest (ROI) as the radiolucent defect area in dental panoramic views and drawing the contour of the bone defect using the selection tool of Adobe Photoshop CS6, the average densities of the selected area could be obtained as pixel values.(
Fig. 1) We analyzed the panoramic views taken before prescription and three and six months after the first prescription. One observer measured the densities of the ROI and contralateral side and used the average value of the three measurements. Clinical photographs were taken at the same time point as the radiographs, and the degree of densities in the radiographs was compared with the clinical characteristics. Bony healing was evaluated by two methods: the first method involved measurement of radiographic densities of ROI, while the second method calculated the ratio of the densities of ROI to the opposite side. Densities of the contralateral side to the ROI was measured by the same method and set as the reference value. Using the selection tool of Photoshop CS6, the same dimension was designated for analysis with reference to the number of pixels of the selected area. The teeth and foreign body were excluded from the ROI and only the bone area was evaluated. The differences of densities between ROI and the reference value were used for statistical analysis with the IBM SPSS 23.0 program (IBM Corp., Armonk, NY, USA). The Mann–Whitney test and repeated measures ANOVA were used in the study, and the results were considered statistically significant at
P<0.05.
 | Fig. 1The method used in this study to quantify the densities of defects in the panoramic views. These analyses were performed using Adobe Photoshop CS6 Histogram (Adobe System Inc., USA).
|
Initial complete blood count (CBC) and erythrocyte sedimentation rate (ESR) were statistically analyzed between disease groups using the Kruskal–Wallis test. The Bonferroni correction was used to modify the alpha level, and statistical significance was considered at P<0.05.
We compared the blood sample tests for baseline and follow up data after three to six months. The inflammatory markers of white blood cell (WBC), ESR, and absolute neutrophil count (ANC) were compared according to time, duration of PTX and tocopherol usage, and disease entity. Statistical analysis was performed with repeated measures ANOVA, and the results were considered statistically significant at P<0.05.
The collection and processing of this retrospective clinical data were approved by the Institutional Review Board of Seoul National University (IRB No. S-D20160041).
Go to :

III. Results
Among the 25 patients, 8 were diagnosed with ORN, 9 were diagnosed with BRONJ, and 8 were diagnosed with chronic osteomyelitis.(
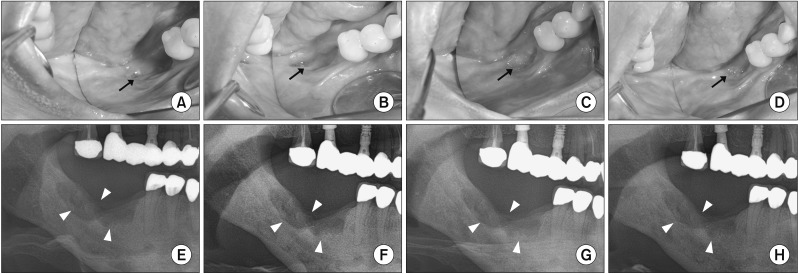
Table 1) Ten of the 25 patients were men; however, the proportion of women was significantly higher in the BRONJ group, 8 of 9 patients. The average age was 66.32±14.39 with a duration of medication of 151.8±80.65 days (range, 56–315 days). Two patients received only medical treatment with one patient receiving RT to cure tonsillar cancer 8.3 years prior to refer from a local clinic for an unhealed extraction socket diagnosed as ORN. The patient was treated with PTX and tocopherol for approximately 10 months, and radiographic densities increased in the panoramic view. Clinical photos were taken at the same time as the radiographs. One year after PTX and tocopherol usage, soft tissue healing was observed without bony exposure.(
Fig. 2) The other patient was diagnosed with squamous cell carcinoma on the lower gingiva and treated with partial mandibulectomy, partial maxillectomy, and selective neck dissection and reconstruction with a radial forearm free flap. Postoperative RT was performed for near resection margins and perineural invasion. Radiographic change was observed during osteotomy of the mandible with the swing approach. The patient was treated with PTX and tocopherol for approximately 6 months. Other patients, except two, underwent surgical treatment such as curettage, sequestrectomy, saucerization, and initiation of PTX and tocopherol when the surgical site became stable before beginning administration.
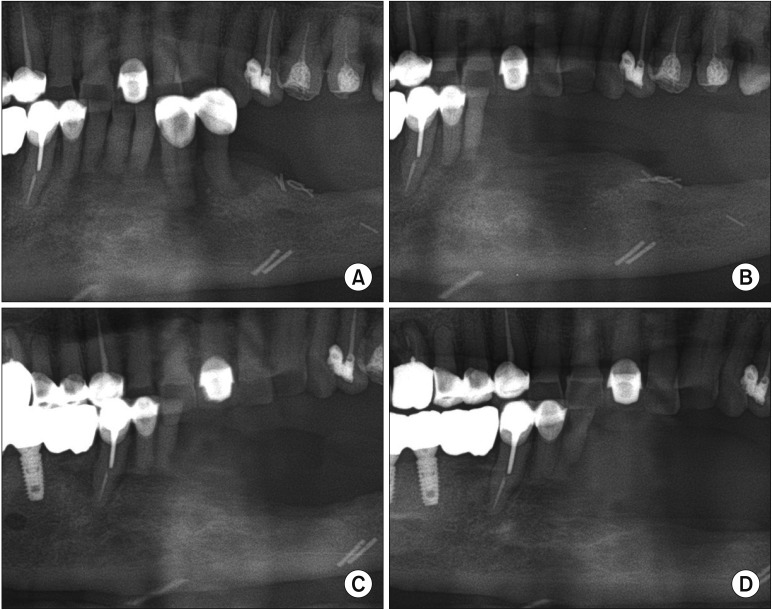
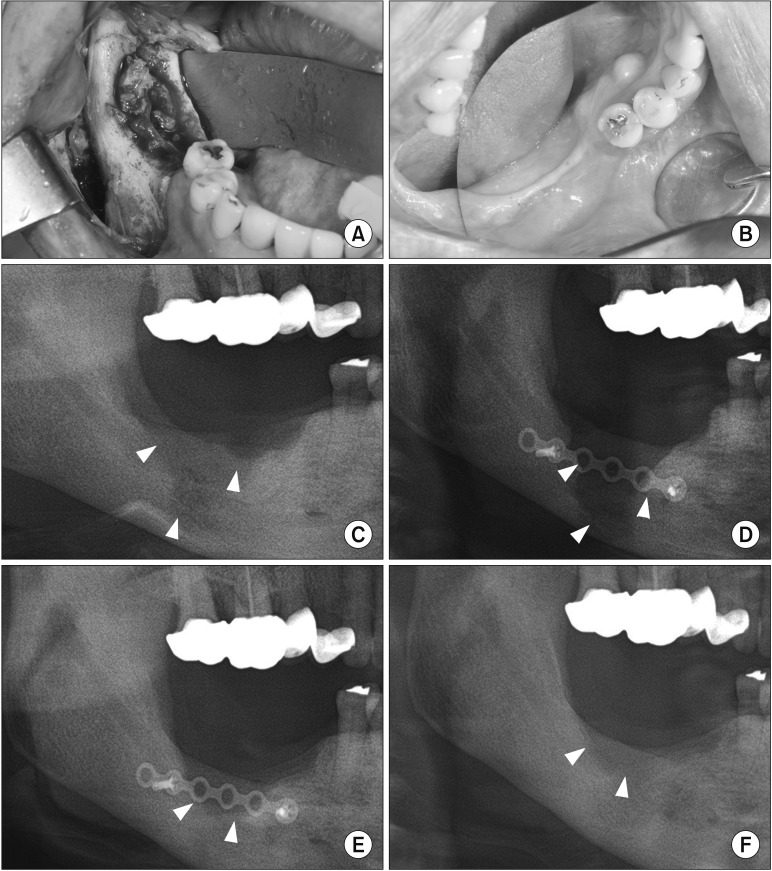
Fig. 3 shows serial radiographic changes of the patient (Case No. 7) with ORN. This patient received surgical intervention including extraction and saucerization. After wound healing, PTX and tocopherol were prescribed for 56 days. Six months after drug administration, the radiographic bony densities decreased and osteolytic bony lesions were extended. However, in the case diagnosed with Stage 3 BRONJ, long-term use of PTX and tocopherol with surgery produced good bony healing.(
Fig. 4) Osteolytic lesions that extended to the mandibular border were diminished.
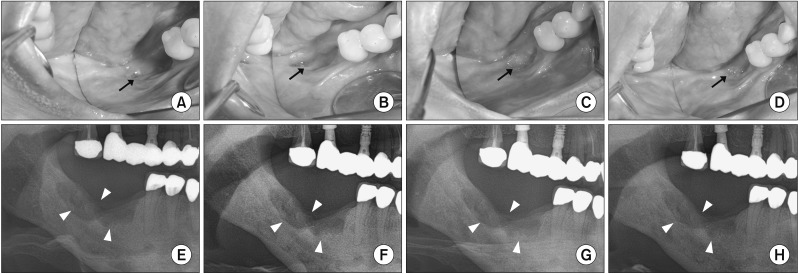 | Fig. 2Serial occlusal clinical photos and panoramic views after using pentoxifylline and tocopherol in the Case No. 2 patient who had not undergone any surgery and had taken medication for osteoradionecrosis for 315 days. A, E. Before prescription. B, F. Three months after drug administration. C, G. Six months after drug administration. D, H. One year after drug administration. (Arrows: lesion with intra-oral bone exposure, decreased over time; Arrowheads: osteoradionecrosis observed in the panoramic radiographs)
|
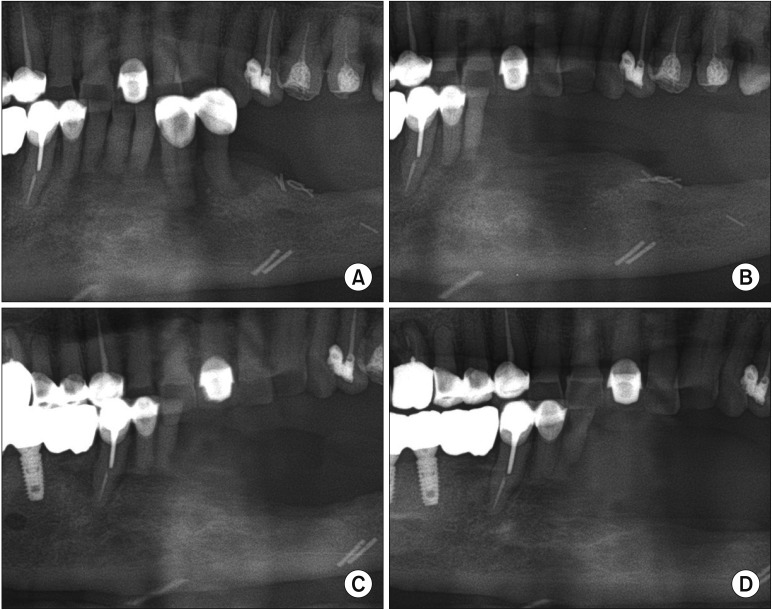 | Fig. 3Serial radiographic changes after using pentoxifylline and tocopherol in the Case No. 7 patient who began medications after surgical wound healing (56 days). A. Before surgical treatment. B. After surgery including extraction and saucerization and before beginning medications. C. Three months after drug administration. D. Six months after drug administration with the figure showing an extended osteolytic lesion.
|
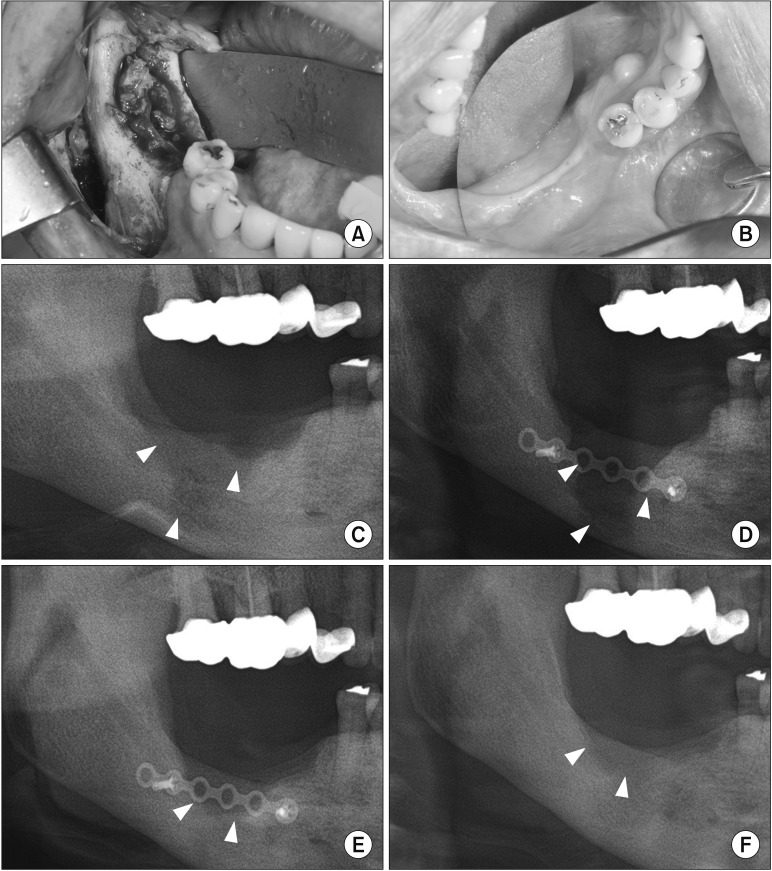 | Fig. 4Serial radiographic changes with clinical photos after using pentoxifylline (PTX) and tocopherol in the Case No. 10 patient who began PTX and tocopherol after surgical wound healing for treatment of bisphosphonate-related osteonecrosis of the jaw (BRONJ) for 8 months. A. Clinical picture showing the pathologic lesion before surgery. B. One year after surgery and drug administration. C. Preoperative panorama showing the lesion extending to the mandibular border. D. One week after surgery, at the beginning treatment of PTX and tocopherol. E. Six months after drug administration. F. One year after drug administration. (Arrowheads: radiolucent lesion of BRONJ in the panoramic views)
|
Table 1
Summary of the cases of ORN, BRONJ, or chronic osteomyelitis treated with PTX and tocopherol

|
Case No. |
Sex |
Age (yr) |
Disease |
Duration of drug usage (day) |
Related past medical history |
Staging |
Radiation dose (Gy)/causative medication |
Initiation factor |
Onset (yr) |
Site |
Intervention |
|
1 |
M |
84 |
ORN |
90 |
ACC on SMG |
2 |
66 |
Ext. |
4.61 |
#35 |
Sequestrectomy |
|
2 |
F |
42 |
ORN |
315 |
Tonsillar cancer |
2 |
- |
Ext. |
8.3 |
#46,47 |
Medication only |
|
3 |
M |
60 |
ORN |
140 |
SCC on lower gingiva |
3 |
60 |
Ext. |
0.62 |
Angle |
OR & IF |
|
4 |
M |
55 |
ORN |
174 |
SCC on lower gingiva |
3 |
63 |
Osteotomy |
0.4 |
Body |
Medication only |
|
5 |
F |
67 |
ORN |
56 |
ACC on parotid gland |
1 |
70 |
Ext. |
5.74 |
#34,35,36,37 |
Saucerization |
|
6 |
F |
71 |
ORN |
98 |
ACC on lower lip |
2 |
72 |
Ext. |
4.07 |
Anterior mandible |
Saucerization |
|
7 |
M |
86 |
ORN |
56 |
SCC on tongue |
2 |
70 |
- |
- |
Anterior mandible |
- |
|
8 |
F |
57 |
ORN |
252 |
SCC on retromolar trigone |
1 |
63 |
- |
1.38 |
#37 |
Saucerization |
|
9 |
F |
61 |
BRONJ |
320 |
Osteoporosis |
2 |
Alendronate |
- |
- |
#45,46,47 |
Saucerization |
|
10 |
F |
79 |
BRONJ |
237 |
Osteoporosis |
3 |
- |
Ext. |
- |
#46,47 |
Sequestrectomy |
|
11 |
F |
83 |
BRONJ |
230 |
Osteoporosis |
2 |
Risedronate, alendronate |
Ext. |
- |
#44,45,46 |
Saucerization |
|
12 |
F |
71 |
BRONJ |
112 |
Osteoporosis |
2 |
- |
Ext. |
- |
#36,37 |
Saucerization |
|
13 |
F |
86 |
BRONJ |
84 |
Osteoporosis |
2 |
Ibandronate |
Ext. |
- |
#45,46,47 |
Saucerization |
|
14 |
F |
70 |
BRONJ |
56 |
Multiple myeloma |
2 |
- |
- |
- |
#37,38 ascending ramus |
Saucerization |
|
15 |
M |
84 |
BRONJ |
168 |
Osteoporosis |
2 |
Ibandronate |
Ext. |
- |
#46,47 |
Saucerization |
|
16 |
F |
69 |
BRONJ |
178 |
Osteoporosis |
2 |
Alendronate |
- |
- |
#47,48 |
Saucerization |
|
17 |
F |
82 |
BRONJ |
119 |
Osteoporosis |
2 |
Alendronate |
Ext. |
- |
#35 |
Saucerization |
|
18 |
M |
79 |
OM |
180 |
- |
1 |
- |
- |
- |
#37,38 |
Sequestrectomy |
|
19 |
F |
50 |
OM |
252 |
- |
2 |
- |
- |
- |
#44,45,46 |
Saucerization |
|
20 |
F |
50 |
OM |
174 |
- |
2 |
- |
- |
- |
#35,36,37 |
Ext., sequestrectomy |
|
21 |
M |
56 |
OM |
168 |
- |
2 |
- |
- |
- |
#47,48 |
Ext., saucerization |
|
22 |
M |
64 |
OM |
140 |
- |
3 |
- |
- |
- |
#38 |
Saucerization |
|
23 |
M |
41 |
OM |
84 |
- |
2 |
- |
- |
- |
#47 |
Sequestrectomy |
|
24 |
F |
67 |
OM |
56 |
- |
1 |
- |
- |
- |
#47 |
Saucerization |
|
25 |
M |
44 |
OM |
56 |
- |
3 |
- |
- |
- |
#48 |
Saucerization |

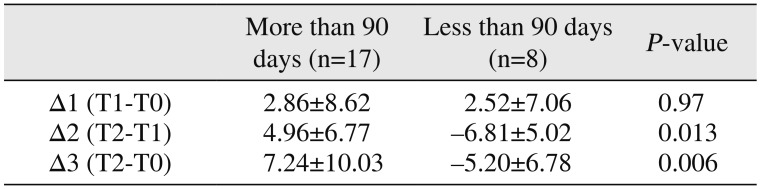
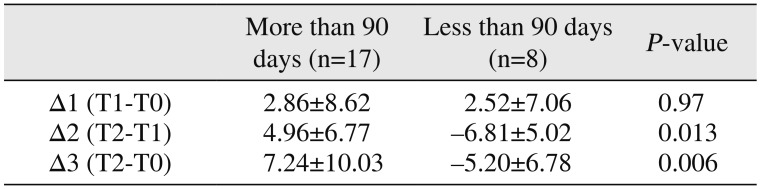
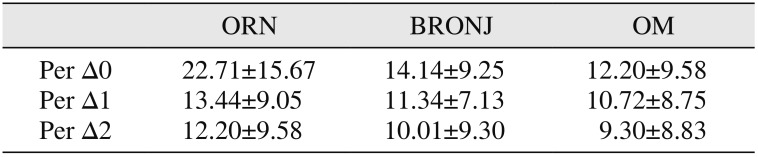
We compared the radiographic changes in the panoramic view at T0 (before the start of medication), T1 (3 months after medication), and T2 (6 months after medication). We divided the experimental group according to duration of medication usage and type of disease. Statistically significant increases were observed in the changes in T2–T1 (Δ2) and T2–T0 (Δ3) in those taking the drug in excess of 90 days (
P<0.05).(
Table 2) There was no significant difference between diseases of ORN, BRONJ, and chronic osteomyelitis. Changes of radiographic densities compared to the reference site were also evaluated. Difference of densities between the ROIs and the contralateral sites was divided by the density of the contralateral sites. The percentages were evaluated before drug administration. Three and six months after administration, the differences of radiographic densities compared to the contralateral sites exhibited statistically significant reductions (
P<0.05). However, there was no statistical difference between the disease groups.(
Table 3)
Table 2
Comparison of changes in radiographic densities according to duration of pentoxifylline (PTX) and tocopherol use
|
More than 90 days (n=17) |
Less than 90 days (n=8) |
P-value |
|
Δ1 (T1-T0) |
2.86±8.62 |
2.52±7.06 |
0.97 |
|
Δ2 (T2-T1) |
4.96±6.77 |
−6.81±5.02 |
0.013 |
|
Δ3 (T2-T0) |
7.24±10.03 |
−5.20±6.78 |
0.006 |

Table 3
Comparison of the time and disease differences of the radiation densities between the region of interest and the contralateral side
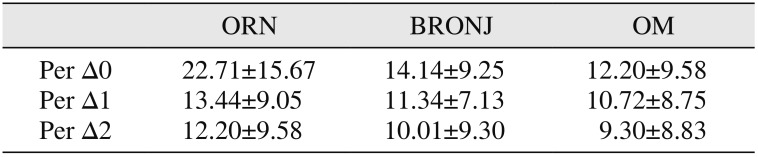
|
ORN |
BRONJ |
OM |
|
Per Δ0 |
22.71±15.67 |
14.14±9.25 |
12.20±9.58 |
|
Per Δ1 |
13.44±9.05 |
11.34±7.13 |
10.72±8.75 |
|
Per Δ2 |
12.20±9.58 |
10.01±9.30 |
9.30±8.83 |

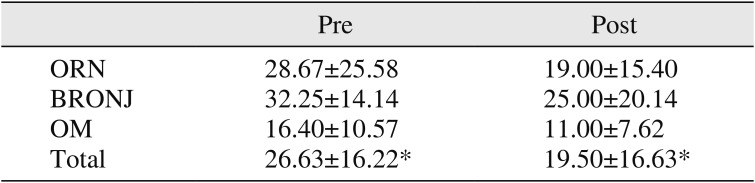
We collected laboratory data including WBC, hemoglobin (Hb), hematocrit (Hct), ANC, and ESR at the initial hospital visit. Statistically significant differences were found in Hb between the ORN and BRONJ groups (
P=0.016). In the laboratory test of inflammatory markers, only ESR exhibited statistically significant changes with time (
P<0.05).(
Table 4) There were no statistically significant differences according to disease group or duration of drug usage over time.
Table 4
Changes in ESR over time
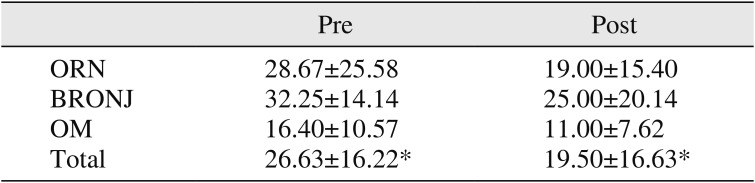
|
Pre |
Post |
|
ORN |
28.67±25.58 |
19.00±15.40 |
|
BRONJ |
32.25±14.14 |
25.00±20.14 |
|
OM |
16.40±10.57 |
11.00±7.62 |
|
Total |
26.63±16.22*
|
19.50±16.63*
|

Go to :

IV. Discussion
The efficacy of PTX appeared within 2 to 4 weeks, and it is recommended that this drug be used for at least 8 weeks. Efficacy has been demonstrated in a double-blind trial for 6 months
12. Radiography is the major non-invasive method for detecting bone healing. In general, bone healing results in an increase in radiopacity, leading to high optical density
13. Therefore, we used panoramic radiographs for evaluation of the effect of PTX and tocopherol in jaw osteomyelitis. In this study, there was a significant increase in radiographic densities in the group administered the drugs for more than 90 days compared to the group that had less than 90-days of administration for a period of 6 months after administration of PTX and tocopherol. At three months, both groups exhibited an increase in radiographic densities. However, between three and six months after administration of drugs (T2–T1, Δ2), the radiographic densities significantly increased in the group that had more than 90 days of administration of the drugs. Since surgical procedures such as curettage, sequestrectomy, and saucerization involve removal of partially pathological bone tissue, the degree of radiographic densities was reduced by surgery. Except for two cases, administration of drugs was initiated after wound stabilization. Therefore, over three months, bone healing occurred after the surgical procedure, and radiographic densities increased in most of the cases. After the initial healing period of surgery, continuous administration of the combination of PTX and tocopherol had a positive effect on bone healing. Not only did the degree of densities of the panorama increase, but intraoral bone exposures and inflammation clinically decreased.(
Fig. 2. D,
4. B) There was no significant difference in degree of increase in radiographic densities based on disease.
In the result of the ratio of densities of ROI compared to the contralateral site, there was no statistical significance between disease group and duration of drug administration (P>0.05). Due to radiographic characteristics after bone healing, the radiographic densities were similar to that of the surrounding bone, not contralateral side. In BRONJ, sclerotic changes were more often observed compared to that in ORN and osteomyelitis. After the bone healing period, radiographic densities further increased compared to the reference contralateral site.
Typically, the first choice for diagnostic imaging of osteonecrosis or osteomyelitis is the dental periapical view and panoramic radiography. Panoramic radiography is relatively easy to perform, is inexpensive and convenient, and exposes the patient to the lowest radiation dose
14. Initial changes of ORN manifest in subtle areas of deformed trabecular structures with rarefaction. As the disease progresses, osteolytic bone destruction becomes radiographically evident and produces a patchy radiolucent appearance with radiodense islands of necrotic bone or sequestrum. In BRONJ, radiographic changes include osteolytic and sclerotic lesions. While the radiographic appearances of ORN and BRONJ may overlap, the prominent activation of osteoclasts and the attenuation of osteoblastic function during ORN result in the rarefying appearance with loss of cortical outlines and trabecular density. In contrast, osteoclastic inhibition in BRONJ resulted in an overall increase in density of the trabeculae and cortex
15. In our results, there were no statistical differences between the disease groups. However, in the BRONJ group, radiographic densities increased after wound healing compared to the contralateral site. ORN exhibits predominantly osteolytic lesions on radiographs, while sclerotic lesions are frequently observed with BRONJ. Changes in the degree of densities on x-rays are greater for ORN lesions even though there is no statistical significance.
Unfortunately, there are no long-term follow-up patients after discontinuation of PTX and tocopherol for therapeutic benefit. Of the 8 patients who took drugs for short-term period, five patients were treated with chronic osteomyelitis and BRONJ. Even after the drug was withdrawn, they showed stable bone healing. One of the other three patients in the ORN group showed same radiolucent lesion in the panorama one year after drug cessation. He started PTX and tocopherol treatment again. The rebound effect after drug withdrawal may be related to the type of disease and the extent of the lesion.
Laboratory data including WBC, Hb, Hct, ANC, and ESR values were collected at the initial hospital visit. Statistically significant differences were found in Hb between the ORN and BRONJ groups (P=0.016). The mean value of Hb in BRONJ patients was lowest of the groups since most of the patients were older women suffering from osteoporosis. Among the inflammatory laboratory markers, only ESR exhibited statistically significant change with time. However, there were no differences between ORN, BRONJ, and chronic osteomyelitis. Therefore, recovery of ESR to normal range may be considered as an index to evaluate successful treatment of osteomyelitis.
Established radiation induced bony damage is known to be irreversible. However, Delanian and Lefaix
16 suggested that radiation induced fibrosis could be reversed by antioxidant therapy with PTX, tocopherol, and clodronate. Delanian et al.
6 published a prospective clinical trial of 18 patients diagnosed with mandibular refractory ORN who had failed to improve after at least two months of conventional treatment. Sixteen of the 18 patients with ORN had complete mucosal healing with a median time to recovery of six months. Delanian et al.
7 developed an impressive regimen (PENTOCLO-PENtoxifylline-TOcopherol-CLOdronate) in a refractory group of 54 patients. The amount of exposed bone was reduced by 42% (2 months), 62% (4 months), 77% (6 months), 92% (12 months), and 96% (18 months). McLeod et al.
17 reported a retrospective study of 12 patients who received PTX and tocopherol with improvement in five patients, no change in five patients, and worsening in two patients. However, three patients whose final score improved after operations despite progression of ORN while on PTX and tocopherol underwent radical resection and reconstruction. In a retrospective study of 71 patients treated for ORN of the mandible after medical management composed of PTX, tocopherol, and doxycycline, the patients who required resection and free flap reconstruction declined from 51% (20/39) to 25% (8/32)
18.
In a study of six patients in the field of BRONJ treatment, all the patients with BRONJ after treatment with PTX and tocopherol exhibited improved symptoms by an average reduction of 74% in bone exposed areas
19. ONJ from osteoporotic patients who underwent yearly zoledronic acid administration and were concomitantly treated with corticosteroids was effectively managed with PTX and tocopherol
20. In a recent case series, all seven patients suffering from ONJ demonstrated symptom relief, while four patients exhibited bony regeneration of radiolucent defects
21.
In this clinical study, two patients (Cases No. 2 and No. 4) were diagnosed with ORN and received only medical treatment with PTX and tocopherol without any surgical intervention. Those patients did not experience any adverse effects due to the medication. Clinical photos and serial panoramic views show mucosal coverage and gradient bone occupying the defect.(
Fig. 2)
Generally, established ORN, BRONJ, and chronic osteomyelitis do not regress spontaneously. Pathologic lesions can be stabilized or gradually worsen and can often be enlarged to such an extent that management becomes difficult. PTX has been reported to reduce radiation induced fibrosis. The mechanism of inhibiting fibrosis or reversing fibrosis has yet to be elucidated
22. PTX has been shown to enhance microvascular blood flow and reduce platelet aggregation to maintain perfusion in radiated tissue. PTX also down-regulates the production of proinflammatory cytokines, particularly TNF-α, in response to noxious stimuli and inhibits granulocyte-mediated cytotoxicity after TNF-α exposure and provides protection against radiation-induced, cytokinemediated cellular damage
23. PTX and tocopherol can be used as an auxiliary to surgery for the treatment of ORN, BRONJ, and chronic osteomyelitis. Unfortunately, there is no guideline for how long PTX and tocopherol should be taken. In a study by Delanian et al.
24, two-thirds of patients responded to a maximal response after an average of two years. They recommended that long term treatment of more than three years in the presence of severe radiation induced fibrosis because of the risk of rebound effects. In this study, most patients were treated with primary surgery such as curettage, sequestrectomy, and saucerization. Drugs have been shown to increase bone filling and stabilize pathological conditions of the mandible when used over an extended period of three months or more. Further long-term studies involving large numbers of patients with additional inflammation markers, such as C-reactive protein and procalcitonin, are needed.
Go to :






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download