This article has been
cited by other articles in ScienceCentral.
Abstract
Objectives
The aim of this study was to evaluate pulmonary function in patients with mandibular fractures and to determine the pattern of pulmonary functions in these patients.
Materials and Methods
This was a cross-sectional study of pulmonary functions in Nigerian non-smoking patients with isolated mandibular fractures managed at our health institution from December 2015 to June 2017. Forced vital capacity (FVC), forced expiratory volume in one second (FEV1), peak expiratory flow rate (PEFR), and ratio of FEV1 to FVC (FEV1/FVC) were measured for all participants using a portable spirometer just before treatment. The pulmonary indices were compared with the predicted reference values for Nigerians to determine the respiratory pattern.
Results
Forty participants consisting of six females (15.0%) and thirty-four males (85.0%) with a female to male ratio of 1:5.7 were included in this study. The mean patient age was 34.5±13.1 years (range, 17–63 years). The mean FVC, FEV1, FEV1/FVC, and PEFR were 3.8±1.2 L, 3.0±1.0 L, 74.3%±13.8%, and 5.2±2.2 L/s, respectively. Comparison of data with predicted values revealed that 17 subjects (42.5%) had normal pulmonary function pattern while 23 subjects (57.5%) had features suggestive of obstructive and restrictive pulmonary function patterns.
Conclusion
Isolated mandibular fractures presented with abnormal pulmonary function pattern.
Keywords: Pulmonary function, Mandibular fractures, Spirometry, Airway obstruction
I. Introduction
Mandibular fractures do not typically present with respiratory difficulty or pulmonary complications
12. However, there are rare cases of mandibular fractures with related airway obstruction mostly due to loss of anterior tongue support and mandibular attachment of genioglossus
234. In addition, treatment of mandibular fractures by closed reduction with maxillomandibular fixation has been reported to cause airway obstruction with potentially fatal implications in patients with respiratory disease
567.
The pulmonary function of patients with mandibular fractures without rare, emergent airway compromise is still unknown and whether these stable isolated mandibular fractures present with normal or deranged pulmonary function has not been evaluated. The aim of this study was therefore to evaluate the pulmonary function and patterns in patients with isolated mandibular fractures.
II. Materials and Methods
This was a cross-sectional study of 40 Nigerian patients with clinical and radiological features of isolated mandibular fractures who were managed at the Obafemi Awolowo University Teaching Hospitals Complex (OAUTHC), Ile-Ife, from December 2015 to June 2017. The study was approved by the Ethics and Research Committee of the OAUTHC (ECR/2015/05/08). All recruited patients signed informed consent forms. The study was conducted in compliance with the Declaration of Helsinki. None of the studied participants presented with clinical features of respiratory distress or impending airway compromise.
Exclusion criteria included subjects with pre-existing lung pathology or respiratory disease, current smokers or those who stopped smoking less than two years ago, and subjects whose occupations might predispose them to impaired pulmonary function, such as cement factory, bakery, sawmill, and wheat flour mill workers.
Biodata were recorded and weight and height of subjects were measured using a weighing scale (Seca Scales; Seca, Birmingham, UK) and stadiometer (CMS Weighing Equipment, London, UK). Forced vital capacity (FVC), forced expiratory volume in one second (FEV
1), peak expiratory flow rate (PEFR), and ratio of FEV
1 to FVC (FEV
1/FVC) were measured for all participants just before treatment using a Spirobank G spirometer (Medical International Research, Rome, Italy). This spirometer has a turbine sensor that obviates calibration.(
Fig. 1) The procedure was explained to the participants and was performed according to the American Thoracic Society and European Thoracic Society standards and recommendations
8.(
Fig. 2)
Predicted values of pulmonary function parameters (FVC [L], FEV
1 [L], FEV
1/FVC [%], and PEFR [L/s]) were determined using reference values for Nigerians
8. The measured pulmonary function values from all patients were compared with the predicted values. Participants with FEV
1/FVC less than 70% were categorized as having obstructive pulmonary function abnormality. Participants with FVC values less than 80% of the predicted value were classified as having a restrictive pulmonary function pattern, while those with FVC values greater than or equal to 80% of the predicted value were categorized as having a normal pulmonary function pattern
910.
Data analysis was performed using IBM SPSS Statistics (ver. 21; IBM Corp., Armonk, NY, USA). Descriptive statistics were carried out for socio-demographic variables. Descriptive variables that were continuous parameters such as mean, median, minimum, maximum, and measures of variability were determined. For descriptive variables that were categorical, simple frequencies and percentages were determined. Fisher's exact test was used to determine any association between pulmonary function pattern and mandibular fracture sites. A P-value less than 0.05 was considered significant.
III. Results
Forty subjects with isolated mandibular fractures consisting of six females (15.0%) and 34 males (85.0%) with a female to male ratio of 1:5.7 were included in this study. The mean age of participants was 34.5±13.1 years, with a range of 17 to 63 years. Most participants (45%) were in the third decade of life.
Road traffic crashes (automobile, motorcycle, and pedestrian injuries) accounted for 87.5% of all sampled fractures while assaults (5%), sports-related accidents (5%), and occupational accidents (2.5%) were responsible for the remaining fractured mandibles.
Twenty-three patients (57.5%) presented with unilateral mandibular fracture, 16 patients (40.0%) had bilateral mandibular fracture, and double unilateral mandibular fracture was seen in one subject (2.5%). The body of the mandible was the most fractured site (54.4%) with fractures occurring at mandibular parasymphyseal and angle regions, accounting for 21.1% and 12.3% of fractured sites, respectively.
The mean FVC, FEV
1, FEV
1/FVC, and PEFR were 3.8±1.2 L, 3.0±1.0 L, 74.3%±13.8%, and 5.2±2.2 L/s, respectively. As stated under Materials and Methods section, 17 subjects (42.5%) had normal pulmonary function pattern while 23 subjects (57.5%) had abnormal pulmonary function patterns (obstructive and restrictive).(
Table 1) There was no statistically significant association between pulmonary function pattern and mandibular fracture sites.(
Table 2)
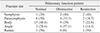
Table 3 shows the participants' pulmonary function patterns at the 7th postoperative week.
IV. Discussion
Age and sex distributions of the participants in this study were similar to previous reports on maxillofacial fractures in Nigeria, in which mandibular fractures are prevalent among men and most common in the third decade of life in both sexes
11. Road traffic crash was responsible for most of the mandibular fractures in this study. This is in agreement with the findings of Chrcanovic et al.
12 and Oginni et al.
13 but in contrast to etiological factors in developed nations, in which assaults and interpersonal violence are the leading causes of mandibular fractures
14.
The mean preoperative values of measured pulmonary function parameters in the present study were similar to those in the report by Akhiwu et al.
6. In the previous report, however, the authors failed to measure FEV
1/FVC and interpret pulmonary function parameters of each subject in the study. Therefore, categorization of patients (whose parameters were measured) into different respiratory function patterns (normal, obstructive, and restrictive) was not performed. Despite the fact that mean pulmonary function parameters of all participants were normal compared with predicted values
915, analysis of measured pulmonary function parameters for each participant revealed that more than half of the participants had abnormal respiratory function (obstructive and restrictive respiratory patterns), while 17 participants (42.5%) had normal respiratory function pattern.
The implication of this finding is that impaired pulmonary function can be found in patients with mandibular fractures with no lung disease, previous history of smoking, or occupational exposure that could predispose them to abnormal respiratory function. Our finding is unexpected in this group of stable patients with no airway compromise and background pulmonary disease. This is in sharp contrast to the severe and life-threatening cases of airway compromise following mandibular fractures often managed in emergency rooms
234.
In cases of isolated mandibular fractures in conscious patients with no comminuted or severely impacted anterior fractured segment, as in the present study participants, there is some degree of pulmonary dysfunction that patients have ability to cope with. This is in line with the observation by Chen et al.
16 who evaluated the relationship between upper airway space and changes in hyoid position following mandibular fractures in 180 patients and 30 volunteers and found that mandibular fractures are closely related to upper airway and hyoid position. The authors concluded that bilateral mandibular body and parasymphyseal fractures have a significant influence on oropharyngeal and laryngopharyngeal portions of the upper airway with consequent respiratory function impairments
15. This may lead to an unstable tongue base with backward and downward displacement of the fractured anterior segment in comminuted and unfavorable parasymphyseal fractures
2416.
Of all unilateral mandibular fractures, only unilateral mandibular body fracture was found to significantly affect the laryngopharyngeal airway
16. There was no association between the pulmonary function pattern and fracture site in the present study, which was probably due to the small sample size and exclusion of mandibular condylar fractures. Furthermore, sublingual hematoma and edema, which are clinical signs of mandibular fractures, were also found to reduce tongue space and tend to displace the tongue backward, resulting in narrowing of the oropharynx
16, and pain from a fractured mandible may be responsible for suboptimal pulmonary function found in these participants with isolated fractured mandibles.
The limitations of this study include its small sample size, heterogeneous duration of injury, and non-assessment of presenting pain before pulmonary function tests were done. In addition, oxygen saturation in the study participants was not evaluated. Further study with a large sample size to determine pulmonary function in stable mandibular fracture patients with similar duration of injury and baseline assessment of pain and oxygen saturation is warranted.
V. Conclusion
These drawbacks notwithstanding, isolated mandibular fractures may be associated with impaired pulmonary function parameters, as some participants presented with values suggestive of obstructive and restrictive pulmonary function patterns.
Figures and Tables
Fig. 1
Portable office spirometer used for pulmonary function tests.

Fig. 2
A study participant undergoing spirometry testing.

Table 1
Pulmonary function pattern of participants

Table 2
Distribution of participants' fracture sites and pulmonary function patterns
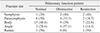
Table 3
Comparison of participants' pulmonary function patterns at baseline (preoperatively) and 7th postoperative week





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download