Abstract
Dental treatment under sedation requires various sedation depths depending on the invasiveness of the procedure and patient drug sensitivity. Inappropriate sedation depth may cause patient discomfort or endangerment. For these reasons, patient-controlled sedation (PCS) pumps are commonly used. Patients are able to control the sedation depths themselves by pushing the demand button after the practitioner sets up the bolus dose and lock-out time. Dexmedetomidine is an α-2 adrenoreceptor agonist with sedative, analgesic, and anxiolytic properties. It has been widely used for sedation for its minimal respiratory depression; however, there are few studies on PCS using dexmedetomidine. This study assessed the applicability of dexmedetomidine to PCS.
Dental treatments under sedation require different sedation depths according to the invasiveness of the procedure and because patient drug sensitivity varies. Thus, appropriate sedation may be difficult by typical drug administration [1]. For these reasons, patient-controlled sedation (PCS), based on the principles of postoperative patient-controlled analgesia, has been in clinical use for about 20 years. In PCS, medication is administered when the patient pushes the demand button after the bolus dose and lock-out time have been set. Propofol or midazolam is often used in PCS [2], but various fields have reported on sedation using dexmedetomidine. Because dexmedetomidine presents a lower risk of delirium or hypoventilation, it may be more a better choice than conventional sedatives [3]. In this context, we report a case of our own experience by using PCS with dexmedetomidine to perform oral surgery on a patient with dental phobia.
The patient was a 50-year-old man (height 159 cm, weight 69 kg) scheduled for extraction of impacted wisdom teeth (#18, 28, 38, and 48) and saucerization owing to chronic osteomyelitis in the right mandibular molar area. The patient had a history of heavy snoring, but was otherwise in good health. However, he had an extreme phobia of tooth extraction. The oral surgeon also determined that the procedure would be highly invasive; as a result, intravenous sedation was requested from the department of dental anesthesiology. We planned conscious sedation using dexmedetomidine to help secure the patient's airway during the extraction procedure. The authors also planned PCS for adequate titration of sedation levels. The patient received an explanation about the dental procedure under sedation, after which he provided written consents for the procedure and the case report.
The results of the pre-anesthesia examination performed the day before the surgery after the patient was admitted showed no specific findings, except eosinophil levels elevated to 13% in the blood test. He was given instruction for NPO for eight hours before the procedure and was sent to the operating room after securing an 18-gauge intravenous line in his left arm.
The PCS pump used was a Perfusor® Space PCA Infusion Pump System (B. Braun Medical Inc., Germany). Dexmedetomidine (Precedex 200 µg/2 ml) was diluted in normal saline to prepare a 50 ml solution at 4 µg/ml. Without setting a basal infusion dose in the PCS pump, the bolus dose, lock-out time, and injection speed were set to 0.1 µg/kg, 1 min, and 1,500 ml/h, respectively.
Electrocardiogram, noninvasive blood pressure, oxygen saturation, and bispectral index (BIS) monitors were attached to the patient. The patient held the PCS demand button in one hand and the patient was instructed to push the button if he felt any anxiety or pain. Oxygen was supplied through a nasal canula, while capnography measurements were obtained simultaneously (Fig. 1).
The sedation procedure took a total of 100 min, and the procedure included saucerization of the region around #37 and extraction of impacted wisdom teeth (#18, 28, 38, and 48). The single dose administered when the patient pushed the button was 1.73 ml, equivalent to 6.93 µg. The patient pushed the button a total of 13 times, but was pushed four times within the lock-out time; therefore, the drug was actually administered nine times, totaling 15.6 ml (62.4 µg).
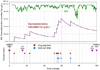
The patient maintained his state of consciousness and was able to respond to commands. His respiratory rate and vital signs also remained within a normal range (Fig. 2). During the operation, the button was pushed several times during painful procedures. Afterwards, the BIS value dropped to around 60 once, but was maintained around 90 throughout. The serum dexmedetomidine concentrations calculated from the patient and the number of times the button was pushed are shown in Fig. 3. The patient was discharged the next day without any complications.
During dental procedures, pain is controlled with appropriate local anesthesia, but pain may still occur depending on the type of procedure and individual situations. Many patients have fear and anxiety about pain related to dental procedures, which presents difficulties in providing the proper treatment [4]. Therefore, the use of sedation techniques is increasing in an effort to reduce the level of anxiety and stress experienced by patients, in addition to controlling pain [5]. Generally, sedation controls the patient's state of consciousness, but depending the sedation depth is associated with risk of hypoventilation and airway obstruction [2]. Moreover, interpatient differences in sedation depth may occur based on the invasiveness of the procedure, and situations may arise in which the patient is unable to cooperate adequately. In addition, patients may be dissatisfied with the person performing the sedation procedure [6]. In particular, because individual patients can show varying stress reactions, drug sensitivities, and degrees of anxiety and pain, it is often impossible to administer a uniform drug dose, which also makes appropriate, controlled administration of such drugs all the more necessary.
For these reasons, PCS, which involves the injection of sedatives when the patient pushes a demand button as needed after the bolus dose and lock-out time have been set, was first implemented for clinical use about 20 years ago and has been in use since [7]. Review of existing data on clinical experience with PCS indicates that giving patients the authority to control their levels of anxiety or pain results in increased satisfaction with the procedure [8910].
The drugs used in PCS must allow a state of sedation to be reached quickly; in addition, the depth and active duration of sedation must be easily controllable, and must not show adverse effects such as cardiovascular inhibition or respiratory depression. However, it is difficult to find drugs that meet these criteria. In actuality, sedatives such as propofol and midazolam are commonly used, either alone or in combination [2]. For procedures that require pain control, sedatives are often combined with fastacting analgesics such as alfentanil, remifentanil, and ketamine. Because it is believed that fast-acting drugs offer better efficacy during PCS; administration of propofol is preferred over that of midazolam because it more quickly reaches its maximum effect after injection [11].
However, when a dentist administers PCS, midazolam is preferred since it has excellent anti-anxiety and memory loss effects, as well as relatively fewer adverse effects, such as respiratory depression. Garip et al. administered 2 ml midazolam at 0.5 mg/ml and a lock-out time of 5 min for extraction of the 3rd molars. When compared to combined administration with 12.5 µg/ml of remifentanil, a higher level of satisfaction was found [12]. Recent cases using dexmedetomidine have also been reported [13].
Dexmedetomidine is a powerful selective α2-adrenoceptor agonist, which is more receptor-sensitive than clonidine, with 10-fold greater sedation and pain control effects [1415]. Dexmedetomidine-treated individuals were easily roused and cooperative despite having achieved clinically effective sedation, which is unique compared with currently available sedatives [16]. Dexmedetomidine (2.0 µg/kg), administered as a 2-min infusion to 37 healthy males, produced a slight increase in carbon dioxide partial pressure (pCO2) and a decrease in minute ventilation with minimal change in ventilator frequency [17]. Intravenous dexmedetomidine did not cause respiratory depression in volunteers who received a 24-hour maintenance infusion (target plasma concentrations ranging from 0.3 to 1.25 µg/L). SpO2 remained ≥90% in all individuals [17].
Intravenous administration of dexmedetomidine for 2 min at 0.25-2 µg/kg reportedly results in a dose-dependent sedation with a maximum effect after 10 min [18]. In our case, the bolus dose was set to 0.1 µg/kg and lock-out time to 1 min. In addition, the dose was set to deliver up to 0.3 µg/kg within 2 min and up to 1.0 µg/kg over 10 min. This dose represents the typical loading dose used in sedation for dental treatments [19]. The lock-out time was set to the relatively short time of 1 min because dexmedetomidine has a relatively small effect on respiration and hemodynamics. However, this time setting can be considered short with respect to the pharmacodynamic aspect of maximum effect of 10 min reported in Koreans [20]. As a result, the observed decrease in BIS relative to serum concentrations calculated from pharmacodynamic index occurred after 10 min (Fig. 3).
In our case, sedation was successfully performed using PCS with dexmedetomidine on a patient with dental phobia. This method may be a useful sedation technique that may help increase patient satisfaction and reduce respiratory depression during dental treatments.
Figures and Tables
Fig. 1
Upper Left: Patient with nasal cannula and Bispectral index sensor, with 3 L/min O2 supplied through the nasal cannula. Upper right: Demand button on patient's hand, with a Velcro belt that prevents the patient from missing the button; Lower left: Upon pressing the button, the patient is administered dexmedetomidine; Lower right: If the patient presses the button more than once within 1 min, the lock-out time is activated.

Fig. 3
Bispectral index and calculated plasma concentrations of dexmedetomidine [20]. BIS: Bispectral index, Cp: plasma concentration of dexmedetomidine
References
1. Senel AC, Altintas NY, Senel FC, Pampu A, Tosun E, Ungor C, et al. Evaluation of sedation in oral and maxillofacial surgery in ambulatory patients: Failure and complications. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 114:592–596.
2. Rodrigo C. Patient-controlled sedation. Anesth Prog. 1998; 45:117–126.
3. Ustun Y, Gunduz M, Erdogan O, Benlidayi ME. Dexmedetomidine versus midazolam in outpatient third molar surgery. J Oral Maxillofac Surg. 2006; 64:1353–1358.

4. Davies JG, Wilson KI, Clements AL. A joint approach to treating dental phobia: A re-evaluation of a collaboration between community dental services and specialist psychotherapy services ten years on. Br Dent J. 2011; 211:159–162.

5. Sbaraglia P. Sedation or general anaesthesia requirements. A literature review of dental phobia. Ont Dent. 1997; 74:19–22.
6. Korean Society for Intravenous Anesthesia. Sedation. 2004. Seoul: Seoul Eui-hak Publishing & Printing Co.
7. Rudkin GE, Osborne GA, Curtis NJ. Intra-operative patient-controlled sedation. Anaesthesia. 1991; 46:90–92.

8. Osborne GA, Rudkin GE, Curtis NJ, Vickers D, Craker AJ. Intra-operative patient-controlled sedation. Comparison of patient-controlled propofol with anaesthetist-administered midazolam and fentanyl. Anaesthesia. 1991; 46:553–556.

9. Oei-Lim VL, Kalkman CJ, Makkes PC, Ooms WG. Patient-controlled versus anesthesiologist-controlled conscious sedation with propofol for dental treatment in anxious patients. Anesth Analg. 1998; 86:967–972.

10. Lok IH, Chan MT, Chan DL, Cheung LP, Haines CJ, Yuen PM. A prospective randomized trial comparing patient-controlled sedation using propofol and alfentanil and physician-administered sedation using diazepam and pethidine during transvaginal ultrasound-guided oocyte retrieval. Hum Reprod. 2002; 17:2101–2106.

11. Rudkin GE, Osborne GA, Finn BP, Jarvis DA, Vickers D. Intra-operative patient-controlled sedation. Comparison of patient-controlled propofol with patient-controlled midazolam. Anaesthesia. 1992; 47:376–381.

12. Garip H, Gurkan Y, Toker K, Goker K. A comparison of midazolam and midazolam with remifentanil for patient-controlled sedation during operations on third molars. Br J Oral Maxillofac Surg. 2007; 45:212–216.

13. Chlan LL, Weinert CR, Skaar DJ, Tracy MF. Patient-controlled sedation: A novel approach to sedation management for mechanically ventilated patients. Chest. 2010; 138:1045–1053.
14. Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000; 59:263–268.
15. Lawrence CJ, Prinzen FW, deLange S. The effect of dexmedetomidine on the balance of myocardial energy requirement and oxygen supply and demand. Anesthesia and Analgesia. 1996; 82:544–550.

16. Chrysostomou C, Schmitt CG. Dexmedetomidine: sedation, analgesia and beyond. Expert Opin Drug Metab Toxicol. 2008; 4:619–627.

17. Belleville JP, Ward DS, Bloor BC, Maze M. Effects of intravenous dexmedetomidine in humans 1. Sedation, ventilation, and metabolic-rate. Anesthesiology. 1992; 77:1125–1133.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download