Abstract
Although inferior alveolar nerve block is one of the most common procedures performed at dental clinics, complications or adverse effects can still occur. On rare occasions, ocular disturbances, such as diplopia, blurred vision, amaurosis, mydriasis, abnormal pupillary light reflex, retrobulbar pain, miosis, and enophthalmos, have also been reported after maxillary and mandibular anesthesia. Generally, these symptoms are temporary but they can be rather distressing to both patients and dental practitioners. Herein, we describe a case of diplopia caused by routine inferior alveolar nerve anesthesia, its related physiology, and management.
Inferior alveolar nerve block is one of the most common and safest procedures performed in dental clinics. However, complications and adverse effects can still occur and can last for either a short or long period of time [1]. These complications are varied and can be drug absorption-related (e.g., toxicity, allergic reaction, syncope, and vasoconstriction) and needle insertion-related (e.g., hematoma, pain during injection, paresthesia, trismus, infection, edema, facial nerve paralysis, needle breakage, and unusual neurological symptoms) [2].
On rare occasions, distant complications, such as ipsilateral ocular disturbances [345678910], have also been reported after both maxillary and mandibulary anesthesia. The ocular disturbances have been described as diplopia (double vision), blurred vision, amaurosis (temporary blindness), mydriasis (papillary dilatation), abnormal pupillary light reflex, retrobulbar pain, miosis (papillary restriction), enophthalmos (recession of the eyeball within the orbit), and ophthalmoplegia (paralysis of muscles responsible for eye movement) [34]. While there is currently no agreement as to the exact cause of ocular complications after local anesthetic injections, it is generally agreed that local anesthetic solutions reach the orbital area through vascular, neurologic, myofascial, and lymphatic networks, and the cause is likely to be different for injections administered in the maxilla versus the mandible [4]. Even though these symptoms tend to be temporary, they can be rather distressing to both patients and dental practitioners. Therefore, awareness of its presentation and knowledge about its physiology and local anatomy is of great importance.
Herein, we describe a case of diplopia caused by routine inferior alveolar nerve anesthesia, its related physiology, and its management.
In March 2015, a 29-year-old female patient was admitted to the Department of Advanced General Dentistry at Dankook University Dental Hospital for extraction of her lower third molar and treatment of dental caries. The patient did not have a specific medical history, any known drug reactions (allergic or toxic), and was not taking any medication. Routine clinical and radiologic examination rendered a diagnosis of chronic pericoronitis of the lower right third molar and moderate dental caries of the lower right first molar. Extraction was planned under local anesthesia with premedication, which included antibiotics and analgesics.
Prior to administering anesthesia, patient vital signs were within normal limits. After the patient was placed in a semisupine position, a conventional inferior alveolar nerve block was administered to the right mandibular quadrant using a 30-mm-long, 27-gauge needle. Aspiration performed during injection revealed absence of blood. Two cartridges of 1.8 ml lidocaine hydrochloride 2% with 1:100 000 lidocaine HCl epinephrine (Huons, Bundang-gu, Korea) were administered. A few minutes immediately after local injection, the patient reported experiencing dizziness, blurred vision, diplopia, and discomfort in her eyelids. Blanching of the face was observed on the patient's right lateral nasal wall, inferior orbital ridge, and temporal area. All procedures ceased immediately and we evaluated the patient. Physical examination revealed no changes in vital signs and her mental status was alert. An ocular function test indicated normal visual activity. Eye movement was normal in all directions and clinical examination did not show any abnormalities in facial nerve range.
We diagnosed the patient with temporary diplopia due to local anesthetic injection. The patient was advised of this condition and her eye was covered with a gauze pad. After 20 minutes , all symptoms subsided and all areas returned to normal. After administration of an additional local anesthetic (using a mandibular infiltration technique with 4% articaine with 1:100 000 articaine HCl epinephrine [Huons, Bundang-gu, Korea]) the lower right third molar was surgically extracted. Post-operative follow up 24 hours later showed no abnormalities.
It is difficult to determine the actual frequency of ophthalmologic complications after local intraoral anesthesia is administered because of its often transitory and mild nature. Complications arise in every 1 in 1 000 patients who have undergone regular dental anesthetic procedures; it occurs more often in women that in men [3]. Among documented ophthalmologic complications, diplopia (39.8%) prevailed while ptosis (16.7%), mydriasis (14.8%), and amaurosis (13.0%) have occurred less frequently. Other ophthalmologic complications, such as accommodation disturbance, enophthalmos, miosis, and ophthalmoplegia, presented in a very limited number of cases [11].
Visual activity directly relates to power of accommodation of the eye [6]. This action depends on lens capsule flexibility and retrenchment of the ciliary muscle, which is innervated by the short ciliary nerves and, in turn, the ciliary ganglion [4]. Normally, the medial longitudinal fasciculus in the brainstem combines cranial nerves III (oculomotor nerve), IV (trochlear nerve), and VI (abducens nerve) to produce coordinated movements of the external ocular muscles of both eyes to maintain parallel bilateral focus. Diplopia arises when a peripheral branch of one of the aforementioned nerves or an external ocular muscle is affected [3].
Various pathophysiologic mechanisms of ophthalmologic complications after intraoral local anesthesia are discussed in the literature-intravascular injection of local anesthetics, direct diffusion of local anesthetics, cervical sympathetic block, reflex vasospasm.
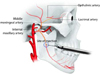
The inferior alveolar vessels (arteries and veins) run posterior to the inferior alveolar nerve, are in closer proximity to the alveolar nerve, and have larger lumina [12]. Although initial aspiration may be negative, marginal movement of either the patient or operator may cause the needle to penetrate the vessel wall. Given that the solution is injected into the inferior alveolar artery under pressure, it may be forced back into the maxillary artery and gain access to the middle meningeal artery. The middle meningeal artery is a branch of the maxillary artery and it enters the skull via the foramen spinosum. It gives breaks off into several branches within the middle cranial fossa and branches back to the lacrimal and ophthalmic arteries. Anesthetic solution carried via this route can produce (via retrograde flow) eye-related symptoms, such as diplopia [4513] (Fig. 1). However, there is a possibility of anesthetic flowing in retrograde direction when the solution is injected under pressure, with a reduction in injection/arterial pressure gradient during diastole.
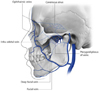
Additionally, after inadvertent administration of anesthetic into the inferior alveolar vein, the anesthetic may flow toward the cavernous sinus via the pterygoid plexus and through emissary veins. Several important structures run through the cavernous sinus (internal carotid artery, abducens nerve) or lie within its lateral wall (oculomotor nerve, trochlear nerve, and ophthalmic and maxillary divisions of the trigeminal nerve). These structures eventually reach the orbit, which explains the occurrence of multiple ophthalmologic complications. Due to its location within the cavernous sinus, the abducens nerve is more vulnerable to the effects of the anesthesia [413]. Alternatively, the solution flows to the orbit (via communication between the pterygoid plexus and the inferior orbital fissure) and reaches the inferior ophthalmic vein, which lacks valves (Fig. 2) [3].
Another hypothesis regarding the cause of diplopia is malfunction of the extraocular muscles after diffusion of the anesthetic solution (following anesthetization of the abductor muscle) in the infratemporal fossa, pterygomaxillary fossa, inferior orbital fissure, or orbital cavity. The effect of diffusion varies depending on type of anesthesia used and caution is required when administering an anesthetic with high diffusion, such as articaine [5].
Contraction of blood vessels or mechanical stimulation of sympathetic vasoconstrictor fibers supplying the area has been reported as a possible cause of skin blanching [8]. If a needle damages an alveolar arterial wall, it may activate sympathetic fibers. It creates a vasospastic impulse that passes the internal carotid plexus and reaches the orbit via the ophthalmic artery. Autonomic dysregulation caused by vascular wall trauma is supported by the often-accompanying phenomenon of facial skin blanching, which is the result of vasoconstriction of the infraorbital artery [3]. Local anesthesia is often combined with a vasoconstrictor to slow local blood flow and resorption, thereby maintaining long-lasting local anesthetic effects. Therefore, adrenaline (epinephrine) works peripherally on the α-adrenergic receptors of the skin and mucosa, and results in constriction of blood vessels and skin blanching [1415].
While ophthalmic complications following inferior alveolar nerve anesthesia are rare, they are distressing events. To prevent ocular complications, all local anesthetic injections should be accompanied by aspiration prior to the actual injection. Effects of diffusion vary depending on type of anesthetic used and caution is required when administering an anesthetic with high diffusion, such as articaine [5]. If a significant amount of anesthetic will be injected, it should be administered slowly and with frequent aspirations. If ocular complications occur, vital signs, presence of unconsciousness, eye movement, blindness, facial muscle movement, and blanching must be evaluated. The following management guidelines are suggested: (1) the dentist reassures the patient of the usually transient nature of these complications; (2) he/she covers the affected eye with gauze dressing to protect the cornea over duration of anesthesia; (3) then, the patient should be escorted home by a responsible adult because their monocular vision is devoid of the capacity to judge distances accurately; and (4) if ophthalmologic complications last longer than 6 hours, the dentist should refer the patient to an ophthalmologist for further evaluation [5].
Figures and Tables
References
1. Malamed S. Handbook of local anesthesia. 5th ed. St Louis: Mosby;2004.
2. The Korean Dental Society of Anesthesiology. Dental Anesthesiology. 2nd ed. Seoul: Koonja;2010.
3. Steenen SA, Dubois L, Saeed P, de Lange J. Ophthalmologic complications after intraoral local anesthesia: case report and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:e1–e5.

4. Boynes SG, Echeverria Z, Abdulwahab M. Ocular complications associated with local anesthesia administration in dentistry. Dent Clin North Am. 2010; 54:677–686.

5. Choi EH, Seo JY, Jung BY, Park W. Diplopia after inferior alveolar nerve block anesthesia: report of 2 cases and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:e21–e24.

6. Ngeow WC, Shim CK, Chai WL. Transient loss of power of accommodation in 1 eye following inferior alveolar nerve block: report of 2 cases. J Can Dent Assoc. 2006; 72:927–931.
7. Rood JP. Ocular complication of inferior dental nerve block. A case report. Br Dent J. 1972; 132:23–24.

8. Uckan S, Cilasun U, Erkman O. Rare ocular and cutaneous complication of inferior alveolar nerve block. J Oral Maxillofac Surg. 2006; 64:719–721.

9. van der Bijl P, Lamb TL. Prolonged diplopia following a mandibular block injection. Anesth Prog. 1996; 43:116–117.
11. von Arx T, Lozanoff S, Zinkernagel M. Ophthalmologic complications after intraoral local anesthesia. Swiss Dent J. 2014; 124:784–806.
12. Khoury JN, Mihailidis S, Ghabriel M, Townsend G. Applied anatomy of the pterygomandibular space: improving the success of inferior alveolar nerve blocks. Aust Dent J. 2011; 56:112–121.

13. Williams JV, Williams LR, Colbert SD, Revington PJ. Amaurosis, ophthalmoplegia, ptosis, mydriasis and periorbital blanching following inferior alveolar nerve anaesthesia. Oral Maxillofac Surg. 2011; 15:67–70.

14. Webber B, Orlansky H, Lipton C, Stevens M. Complications of an intra-arterial injection from an inferior alveolar nerve block. J Am Dent Assoc. 2001; 132:1702–1704.

15. Ezirganli S, Kazancioglu HO. An unforeseen complication arising from inferior alveolar nerve block: is anemia possible? J Craniofac Surg. 2013; 24:2178–2179.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download