Abstract
Sedation allows patients to maintain their airway independently and respond appropriately to physical stimulation and verbal command while maintaining a minimum depressed level of consciousness. Drugs commonly used for sedation of pediatric dental patients include a combination of chloral hydrate, hydroxyzine, and nitrous oxide-oxygen. Midazolam is a benzodiazepine and currently one of the most commonly used intravenous sedative agents. It can be easily titrated to provide a wide range of sedation, from conscious sedation to deep sedation, and exhibits a wide safety margin without severe respiratory and circulatory depression. At an appropriate dose, it also decreases patient anxiety and induces amnesia. We found that the submucosal administration of midazolam combined with chloral hydrate provided increased sedative effects and decreased the postoperative vomiting response compared with conventional chloral hydrate administration, with no significant difference in physiological responses. The depth of sedation can be titrated using this technique.
With an increase in measures to maintain pediatric health because of the observed population decline in recent years, the use of sedation for pharmacological behavior control in children who fear dental treatment is increasing [1]. Wilson and McTigue estimated that 10%-20% of the total pediatric patient population required sedation. Children exhibit increased anxiety or fear toward dental treatment compared with adults, often making it impossible to treat them [2]. Pediatric patient compliance during treatment can directly impact the outcomes; therefore, behavior control is critical. Oppressive physical restraints or hand-over-mouth exercise (HOME) is gradually losing its validity [3]. Sedation can relieve patient stress and induce a minimized state of anxiety and fear, thus providing comfort and safety for the patient and enabling dentists to perform dental treatment smoothly [4]. Commonly used drugs used for pediatric sedation include chloral hydrate (CH), hydroxyzine (H), and nitrous oxide-oxygen (N), although the success rates vary and remain uncertain. Recently, submucosal administration of midazolam (M) along with the oral administration of CH was introduced; several related papers have been published in Korea and are summarized in this paper.
Sedation allows patients to maintain an airway independently and respond appropriately to physical stimulation and verbal command while maintaining a minimum depressed level of consciousness [5]. For the purpose of relieving anxiety, minimal sedation or moderate sedation is employed. In precooperative children under 3 years of age or children who stubbornly refuse treatment, deep sedation is used. In addition, if it is impossible to administer normal treatment to children with physical or mental disabilities, an appropriate level of sedation can be used depending on the level of patient compliance [6]. A study surveying 573 members of the Korean Society of Pediatric Dentistry reported that 66% respondents used sedation in their practice, with commonly used drugs including a combination of CH, H, and N (CH-H-N) [1]. Several studies have evaluated and proven the safety and sedative effects of CH [7]. Furthermore, it was reported that H had antiemetic effects and that its administration in combination with CH resulted in increased sedative effects [8]. The addition of N further enhanced the sedative effects [9].
The sedation success rates with different doses of CH reportedly vary from 18% to 90%, and in most cases with low success rates, a small dose of CH was used [7]. Although the CH dose is incrementally increased to achieve an appropriate sedation level, the resulting potential side effects such as vomiting and nausea cannot be ruled out. Therefore, many studies evaluated combinations of drugs rather than incremented doses of CH only [101112]. In addition, the oral administration of CH is limited by its reliability on patient compliance, a long latency period following administration, irregular and incomplete absorption from the gastrointestinal tract, and the inability to titrate [13].
Benzodiazepines are one of the most commonly used intravenous sedative agents. They can be easily titrated to provide a wide range of sedation, from conscious sedation to deep sedation, have wide safety margins, and carry a low risk of severe respiratory and circulatory depression. Furthermore, an appropriate dose can decrease patient anxiety and additionally induce amnesia. Evident anterograde amnesic effects are induced by intravenous administration, not by other routes of administration. Introduced in clinical practice in the 1980s, M is a benzodiazepine with a short recovery time because it is water soluble and consequently does not form active metabolites [10141516].
M provides increased anxiolytic, sedative, and muscle relaxing effects, with a rapid onset and short duration of action because of its high water solubility. It induces the minimum levels of respiratory and cardiovascular depression and does not increase the local anesthetic level in the plasma. The duration of action is shorter than that of meperidine, and unlike CH, it results in anterograde amnesia [17].
Various studies on M alone or in combination with other drugs have been conducted, and studies evaluating its sedative effects through different routes of administration are also under way [10141516].
Alfonzo-Echeverri et al. [18] indicated that the action pathway and pharmacodynamics of submucosal M injection were similar to those of intramuscular injection. The peak absorption is achieved at 10 min with the former and 20 min with the latter, although there are individual differences and oral submucosal administration can cause pain [18].
Recently, submucosal administration of M following oral administration of CH and H was suggested as an effective alternative to induce sedation during dental treatment of pediatric patients [11]. In cases where dental treatment becomes impossible because of the shallow depth of sedation induced by oral medication, additional submucosal M injection can deepen the depth of sedation. Because M is submucosally administered in a state of partial sedation induced by oral medication, it does not create any additional fear of needle insertion, may not require patient compliance, and is not a difficult method for dentists, considering it is similar to infiltration [19]. Furthermore, submucosal administration should be employed after injection of a small amount of local anesthetic without a vasoconstrictor, because vasoconstrictors included in anesthetics may delay the absorption of sedative agents; likewise, sedative agents may interfere with the effects of local anesthetics [11].
The mechanism of action of submucosal M is reportedly similar to intramuscular injection in terms of pharmacodynamics, with a slightly faster onset of action [20], generally within 15 min [21]. This rapid onset and short duration of action allows increase or decrease of the concentration, which is important for titration [22].
Myers et al. [11] suggested in 2004 that the combination of submucosal M with oral CH administration and N inhalation was an effective alternative to intravenous injection for sedation, with enhanced sedation and no substantial differences in physiological responses. Furthermore, in patients aged 2-5 years who received oral CH and submucosal M, the mean heart rate, respiratory rate, and blood pressure were reported to be within the normal ranges [11]. In another study comparing a group that received oral CH and H (CH-H group) with a group that received buccal submucosal M in addition to oral CH and H (CH-H-M group), the latter exhibited an enhanced sedative effect and a decreased vomiting response [23].
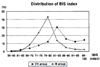
In another study comparing the clinical safety and efficacy of oral CH and H and inhaled N with (CH-M group) or without (CH group) submucosal M for conscious sedation in pediatric patients, evaluation was performed using Houpt's scale. The overall behavior response between groups was compared, with scores of 4, 5, and 6 indicating successful sedation and scores of 1, 2, and 3 indicating failed sedation. No significant difference was observed in the mean crying score between the two groups, while there were significant differences in the mean sleep and movement scores between groups. The CH-M group exhibited better sleep and fewer movements (Table 1). Furthermore, the average score for overall behavior revealed better behavior control in the CH-M group than in the CH group (Table 2). In particular, significant differences were observed for score 6 (Excellent). Therefore, the addition of submucosal M to oral and inhaled medications provided better sedation with lesser movements (Fig. 1) [24].
Another study compared the depth of sedation between CH and CH-M groups using the bispectral (BIS) index. Pediatric subjects were randomly assigned to receive oral CH (60 mg/kg) and H (1 mg/kg) or oral CH (60 mg/kg) and H (1 mg/kg) with submucosal M (0.1 mg/kg); 50% N was maintained during sedation in both groups. The behavior response was evaluated as quiet (Q), crying (C), movement (M), or struggling (S) using a behavior scale. The distribution of behavior responses during a treatment duration of 40 min was determined to reveal 90% G, 7.7% M, 0.5% C, and 1.8% S in the CH group and 92.5% Q, 3.4% M, 0.9% C, and 1.8% S in the CH-M group. Both groups showed the Q response for ≥90% of the duration. These findings indicated no differences in sedative effects between the two groups (Fig. 2).
The BIS index is a numeral scale grading the sedative state on a scale of 0-100, where 0 indicates a state of no brain activity, 40-60 indicates a very deep hypnotic state, 60-70 indicates a moderate hypnotic state, and 100 indicates complete awakening. BIS index scores of 80-90, 60-70, and 90-100 were exhibited by 46%, 20%, and 27% patients, respectively, in the CH group and 66%, 9%, and 19% patients, respectively, in the CH-M group. The score was mainly distributed between 80 and 90 and widely distributed between 60 and 100 in the CH group, while it was intensively distributed between 60 and 100 and rarely distributed within the other ranges (Fig. 3). These results indicate that the addition of submucosal M to oral and inhaled medications can increase the depth and stability of sedation. However, both groups exhibited a score of exhibited a score of 50 for a short period of time for a short period of time. Because the combination involves deep sedation, caution should always be exercised, with emphasis on maintaining and monitoring a free airway [19].
In a study evaluating post-sedation behavior responses and adverse events in pediatric patients who were sedated with submucosal M combined with oral CH and H for dental treatment, many children slept after sedation and showed abnormal behavior and vomiting, although there were no serious adverse events. This indicated the safety of additional buccal submucosal M administration [25].
Another study compared behavior responses and sedative effects between intranasal and submucosal M administered after oral CH and H. Pediatric patients received CH (50 mg/kg) and H (1 mg/kg), and 45 min later, one group additionally received intranasal M (0.2 mg/kg) and the other received buccal submucosal M (0.2 mg/kg); 50% N was maintained during treatment in both groups. There was no significant difference in the mean induction time and maximum treatment time between the two groups. In addition, the vital signs were within the normal ranges, with no significant differences between groups [26].
The rapid onset of action by M means that adverse events or emergency situations can occur rapidly and that the combined use of drugs may increase central nervous system (CNS) inhibition because of drug interactions, leading to a potential risk of hypersedation in which the self-defense reflex unexpectedly disappears [27]. When used with drugs such as barbiturates or alcohol, M can increase CNS inhibition and consequently increase the risk of adverse events such as airway obstruction or hypoventilation. Furthermore, CH produces trichloroethanol as one of its metabolites, which is similar to alcohol. Therefore, the combined use of CH and M may increase the potential for respiratory depression, necessitating extreme caution [28]. In addition, in view of the fact that submucosal injection shows a different absorption route and rapid absorption compared with oral administration, more detailed attention is necessary [29]. Flumazenil, a benzodiazepine antagonist, was introduced in 1980s for use in the management of such adverse events.
Flumazenil can reverse hypersedation associated with benzodiazepines and decrease amnesic effects. It may be administered intramuscularly or submucosally. However, the plasma half-life of flumazenil is shorter than 1 h; therefore, patients who regain consciousness may fall back into a sedative state over time. The use of flumazenil is recommended at an initial dose of 0.3-0.5 mg, and the total dose for patient recovery to an appropriate level of consciousness should not exceed 1 mg [30].
The findings of the abovementioned studies suggest that M can be easily titrated to provide a wide range of sedation, from conscious sedation to deep sedation, has wide safety margins, and carries a low risk of severe respiratory and circulatory depression. When administered in increments over time, titration to adjust the depth of sedation is possible. The use of an appropriate dose can decrease patient anxiety and induce amnesia. In particular, submucosal administration facilitates titration and rapid absorption. Considering that M is administered when the patient is partially sedated with oral medication, it does not provide any additional fear of needle insertion to pediatric patients. Furthermore, submucosal administration is easy for dentists. Finally, the postoperative vomiting response is decreased and intraoperative physiological responses remain stable.
Figures and Tables
 | Fig. 1Percentage overall behavior scores in the CH and CH-M groups in a previous study [24].CH: chloral hydrate + hydroxyzine + nitrous oxide-oxygen; CH-M: CH + midazolam.
|
 | Fig. 2Distribution of behavior responses in the CH and CH-M groups in a previous study [19].CH: chloral hydrate + hydroxyzine + nitrous oxide-oxygen; CH-M: CH + midazolam.
|
 | Fig. 3Distribution of the bisepctral (BIS) index scores in the CH and CH-M groups in a previous study [19]. |
Table 1
Comparison of Houpt's Scale scores between the CH group and CH-M group in a previous study [24]
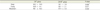
Table 2
Comparison of the overall behavior score between the CH group and CH-M group in a previous study [24]

References
1. An SY, Choi BJ, Kwak JY, Kang JW, Lee JH. A survey of sedation practices in the korean pediatric dental office. J Korean Acad Pediatr Dent. 2005; 32:444–453.
2. Wilson S, McTigue DJ. Survey of conscious sedation practices in pediatric dentistry advanced residency programs. J Dent Educ. 1989; 53:595–597.

3. Carr KR, Wilson S, Nimer S, Thornton JB Jr. Behavior management techniques among pediatric dentists practicing in the southeastern United States. Pediatr Dent. 1999; 21:347–353.
4. Dentistry AAOP. Guideline on behavior guidance for the pediatric dental patient. Pediatr Dent. 2011; 36:179–191.
5. Dentistry AAOP. Guideline on the elective use of minimal, moderate, and deep sedation and general anesthesia for pediatric dental patients. Pediatr Dent. 2005; 27:110–118.
6. Wilson S, Farrell K, Griffen A, Coury D. Conscious sedation experiences in graduate pediatric dentistry programs. Pediatr Dent. 2001; 23:307–314.
7. Nathan JE. Management of the refractory young child with chloral hydrate: dosage selection. ASDC J Dent Child. 1987; 54:22–29.
8. Avalos-Arenas V, Moyao-García D, Nava-Ocampo AA, Zayas-Carranza RE, Fragoso-Ríos R. Is chloral hydrate/ hydroxyzine a good option for paediatric dental outpatient sedation? Curr Med Res Opin. 1998; 14:219–226.

9. Wilson S, Matusak A, Casamassimo PS, Larsen P. The effects of nitrous oxide on pediatric dental patients sedated with chloral hydrate and hydroxyzine. Pediatr Dent. 1998; 20:253–258.
10. Chowdhury J, Vargas KG. Comparison of chloral hydrate, meperidine, and hydroxyzine to midazolam regimens for oral sedation of pediatric dental patients. Pediatr Dent. 2005; 27:191–197.
11. Myers GR, Maestrello CL, Mourino AP, Best AM. Effect of submucosal midazolam on behavior and physiologic response when combined with oral chloral hydrate and nitrous oxide sedation. Pediatr Dent. 2004; 26:37–43.
12. Webb MD, Moore PA. Sedation for pediatric dental patients. Dent Clin North Am. 2002; 46:803–814.

13. Malamed SF. Sedation: A guide to patient management. 5th ed. Elsevier Health Sciences;2009. p. 90–93.
14. Shapira J, Kupietzky A, Kadari A, Fuks AB, Holan G. Comparison of oral midazolam with and without hydroxyzine in the sedation of pediatric dental patients. Pediatr Dent. 2004; 26:492–496.
15. Jensen B. Benzodiazepine sedation in paediatric dentistry. Swed Dent J Suppl. 2005; 153:1–45.
16. Lam C, Udin RD, Malamed SF, Good DL, Forrest JL. Midazolam premedication in children: a pilot study comparing intramuscular and intranasal administration. Anesth Prog. 2005; 52:56–61.

17. Kupietzky A, Houpt MI. Midazolam: a review of its use for conscious sedation of children. Pediatr Dent. 1993; 15:237–241.
18. Alfonzo-Echeverri E, Troutman KC, George W. Absorption and elimination of midazolam by submucosal and intramuscular routes. Anesth Prog. 1990; 37:277–281.
19. Lee YE, Park MK, Kim SY, Kim YH, Jung SH, Baek KW. Sedation evaluation using BIS index assessment with and without the added submucosal midazolam. J Korean Acad Pediatr Dent. 2007; 34:91–98.
20. Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiology. 1985; 62:310–324.
21. Persson P, Nilsson A, Hartvig P, Tamsen A. Pharmacokinetics of midazolam in total i.v. anaesthesia. Br J Anaesth. 1987; 59:548–556.
22. Payne K, Mattheyse FJ, Liebenberg D, Dawes T. The pharmacokinetics of midazolam in paediatric patients. Eur J Clin Pharmacol. 1989; 37:267–272.

23. Lee YE, Park ME, Kim YH, Jung SH, Baek KW. The Sedative Effects of Submucosal Midazolam in Children. J Dent Anesth Pain Med. 2005; 5:101–106.

24. Park MK, Kim YH, Jung SH, Baek KW. Safety and Efficacy of Submucosal Midazolam When Combined with Oral Chloral Hydrate, Hydroxyzine and Nitrous Oxide Sedation by using Houpt's Scale. J Dent Anesth Pain Med. 2006; 6:103–112.

25. Koo JE, Baek KW. Postsedation events in pediatric patients sedated for dental treatment. J Korean Acad Pediatr Dent. 2009; 36:209–216.
26. Kim YH, Jung SH, Baek KW. Comparison of Behavioral Response between Intranasal and Submucosal Midazolam Adminstration. J Korean Acad Pediatr Dent. 2008; 35:427–436.
27. Pearson RC, McCloy RF, Morris P, Bardhan KD. Midazolam and flumazenil in gastroenterology. Acta Anaesthesiol Scand Suppl. 1990; 92:21–24.
28. Sievers TD, Yee JD, Foley ME, Blanding PJ, Berde CB. Midazolam for conscious sedation during pediatric oncology procedures: safety and recovery parameters. Pediatrics. 1991; 88:1172–1179.

29. Griffin JW. Submucosal Sedation 5-year pilot study [abstract]. Anesth Prog. 2000; 47:88.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download