Abstract
Background
During head and neck surgery including orthognathic surgery, mild intraoperative hypothermia occurs frequently. Hypothermia is associated with postanesthetic shivering, which may increase the risk of other postoperative complications. To improve intraoperative thermoregulation, devices such as forced-air warming blankets can be applied. This study aimed to evaluate the effect of supplemental forced-air warming blankets in preventing postanesthetic shivering.
Methods
This retrospective study included 113 patients who underwent orthognathic surgery between March and September 2015. According to the active warming method utilized during surgery, patients were divided into two groups: Group W (n = 55), circulating-water mattress; and Group F (n = 58), circulating-water mattress and forced-air warming blanket. Surgical notes and anesthesia and recovery room records were evaluated.
Results
Initial axillary temperatures did not significantly differ between groups (Group W = 35.9 ± 0.7℃, Group F = 35.8 ± 0.6℃). However, at the end of surgery, the temperatures in Group W were significantly lower than those in Group F (35.2 ± 0.5℃ and 36.2 ± 0.5℃, respectively, P = 0.04). The average body temperatures in Groups W and F were, respectively, 35.9 ± 0.5℃ and 36.2 ± 0.5℃ (P = 0.0001). In Group W, 24 patients (43.6%) experienced postanesthetic shivering, while in Group F, only 12 (20.7%) patients required treatment for postanesthetic shivering (P = 0.009, odds ratio = 0.333, 95% confidence interval: 0.147–0.772).
Inadvertent hypothermia is common in patients undergoing orthognathic surgery. Core temperature may drop by as much as 6℃ under general anesthesia [1]. The average operating time for bimaxillary osteotomy is 3–4 h, but in some cases, the procedure can extend to up to 6–7 h [23]. The combination of prolonged exposure to a cool operating room temperature and impaired thermoregulatory response due to the influence of anesthesia can result in hypothermia [45].
The complications that can arise from hypothermia include heart failure, surgical site infection, prolonged drug action, and immunosuppression, and the condition can also affect kidney function [56]. Shivering is also a common complication of hypothermia following general anesthesia or during moderate to deep sedation. From these muscular contractions, the body will generate heat energy as it raises the metabolic rate by 300% [7]. Thus, the oxygen demand is also far greater than the baseline requirement during shivering, and this may put strain on the cardiovascular system [8]. Shivering is often a distressing experience for the patient, which can be worse than the surgical pain, and it is closely related to patient recovery [5]. Perioperative hypothermia increases the risk of adverse outcomes and affects the postanesthetic recovery of patients [5].
To avoid these complications, the importance of maintaining intraoperative core temperature has been stressed in numerous papers [9]. Possible preventive measures for perioperative hypothermia include the following: prewarming the patient before surgery; raising the ambient temperature; actively warming the patient during surgery; passively warming the patient; warming intravenous fluids or blood products; warming irrigation fluids; and warming the airway gases.
In order to maintain intraoperative normothermia in patients undergoing surgery at Seoul National University Dental Hospital (SNUDH), a circulating-water mattress is commonly used. Although forced-air warming blankets are known to be the most effective in delivering heat, their clinical use has been restricted due to difficulties in application during surgery [10]. The use of surgical drapes, the size and site of the operation, and influence on the ambient surgical environment can limit the use of forced-air warming blankets. To improve the quality of intraoperative thermoregulation management, forced-air warming blankets have been introduced during orthognathic surgery, as the site of the operation does not affect the use of these devices. In the current study, the effectiveness of this additional device in maintaining core temperature during orthognathic surgery and reducing postanesthetic shivering was analyzed.
The institutional review board (IRB) at Seoul National University, School of Dentistry approved this retrospective study (IRB No.: S-D20150039). Consecutive records of patients who underwent planned orthognathic surgery at SNUDH from March to September 2015 were analyzed. As a Quality Improvement activity, operating rooms were equipped with forced-air warming blankets during this time period.
A total of 113 patient records are included in this study. Prior to the planned surgery, patients were assessed for current and past medical history, medications, allergies, and presence of preoperative fever. The Americal society of Anesthesiologist physical status (ASA PS) status was also determined.
Depending on the date of the scheduled orthognathic operation, patients received one of two different core temperature managements:
Group W: Medi-Therm III® circulating-water mattress Hyper/Hypothermia System (Gaymar Industries, Inc., Orchard Park, NY, USA)
Group F: Bair Hugger® forced-air warming blanket with surgical access (Model 525 blanket, Model 505 blower; Arizant Healthcare, Inc., Eden Prairie, MN, USA) and Medi-Therm III® circulating-water mattress.
The following data were obtained from patients' records: age, gender, weight, and height. From this information, body mass index (BMI) and body surface area (BSA) were calculated. The formula used to estimate BSA was the Du Bois formula. Other information collected from records included: length of surgery, duration of anesthesia, anesthetic induction agent, anesthetic maintenance agent, muscle relaxant, opioids, intravenous fluid volume, blood transfusion, and temperature during operation. Postoperative data such as body temperature during recovery, presence of shivering, and the drug type and dosage used to treat shivering were collected from postanesthesia care unit (PACU) records.
The temperature of operating rooms was set at 21℃ and humidity was controlled at 59–61%. When the patient entered the operating room, a thermometer probe (CARESCAPE™ Monitor B650, GE Healthcare, Little Chalfont, Buckinghamshire, UK) was placed in the left axillary fossa of each patient and secured with surgical tape. Vital signs and other measurements such as continuous arterial blood pressure, end-tidal carbon dioxide partial pressure, anesthesia gas monitoring, and bispectral index (BIS) were recorded.
After induction, patients were actively warmed either with a circulating-water mattress only or with a forced-air warming blanket in addition to a circulating-water mattress. In Group W, patients lay on the warm mattress, for which the temperature was set at 37℃, and a cotton blanket was placed on the patient before the body was covered with surgical drapes. In Group F, before covering the patient with surgical drapes, a forced-air warming intraoperative blanket was first placed over the patient. The forced-air warming blanket used in the operating room was designed to cover only the lower half of the patient's body, away from the operation site. The body temperatures of both groups were monitored and recorded continuously from the axillary fossa. When the axillary temperature declined below 36℃, the forced-air warming blanket was activated in Group F to maintain the temperature above 36℃, whereas patients in Group W were solely reliant on the circulating-water mattress. During the last 30 min of the operation, patients in Group F were actively heated with the forced-air warming blanket.
In the recovery room, both groups of patients were covered with a forced-air warming blanket that provided full-body coverage. Patients were closely monitored for any signs of shivering by designated qualified nursing staff. In addition to shivering, other vital signs were monitored and recorded: body temperature, blood pressure, heart rate, and oxygen saturation. If shivering occurred, patients in both groups were given an injection of pethidine hydrochloride (HCl) (50 mg/ml). If the symptom continued even after the first dose of 25 mg, another 25 mg of pethidine HCl was given with an interval of 5–10 min.
Moderate to severe shivering, which distressed the patient sufficiently to require medical intervention, was categorized as postanesthetic shivering. Mild or non-distressing shivering was not included as an incidence of shivering in this study.
Statistical analysis was performed using IBM SPSS Statistics version 22 (IBM Inc., Armonk, NY, USA). The variables were analyzed using the Student's t-test, the chi-square, test or Fisher's exact test according to the data. A value of P < 0.05 was considered significant. The odds ratio for shivering events vs. the warming group was calculated, with a 95% confidence interval.
One hundred thirteen patients who underwent orthognathic surgery at SNUDH were included in the current study. There were 55 patients in Group W and 58 patients in Group F. The demographics and intraoperative variables of the two groups did not differ significantly (P > 0.05). The mean duration of orthognathic surgery was around 7 h in both groups. Estimated BSA was not different significantly between the two groups (P = 0.29). The patient demographics and intraoperative variables are summarized in Table 1.
The initial axillary temperatures were not significantly different between Group W and Group F (P = 0.25), but the difference in temperatures at the end of surgery was significant (<0.001). The difference in axillary temperatures between the two groups was sustained even after patients' transfer from the operating room to the recovery room (<0.001). The axillary temperatures of patients in Group F remained significantly higher than those of patients in Group W at the time of discharge from the recovery room to the wards (<0.001) (Table 2).
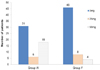
Depending on the occurrence of postanesthetic shivering, Groups W and F were subdivided and the mean axillary temperature during surgery is shown with the 5th-95th percentile in Fig. 1. In Group W, 24 patients (43.6%) suffered from postanesthetic shivering, whereas in Group F, 12 (20.7%) patients required treatment for postanesthetic shivering (Fig. 2, P = 0.009). A total of 36 patients were administered pethidine HCl injection due to postanesthetic shivering. Among those who required treatment for postanesthetic shivering, 50% of patients (n = 18) had been provided with only a circulating-water mattress during the operation and were given 50 mg of pethidine HCl, whereas only 4 patients in Group F were administered the same amount of medication to treat postanesthetic shivering (Fig. 3).
To investigate factors that may result in postanesthetic shivering, patients who experienced shivering were compared with the non-shivering group, and our findings are summarized in Table 3. There were no statistically significant differences between the two groups with the exception of the temperature upon discharge from the recovery room.
In this study, the group that received only a circulating-water mattress to maintain intraoperative temperature was more than twice as likely to experience shivering during the recovery period as the group that received both a mattress and a forced-air warming blanket (Group W = 43.6%, Group F = 20.7%, respectively). It has been demonstrated that regulating body temperature using a forced-air warming device in combination with a circulating-water mattress is more effective in preventing shivering than the use of a mattress alone, as in the findings of Kim et al. [11]. In Group F, the average intraoperative temperature and the temperature at the end of surgery were significantly higher than those of Group W. From these significant differences in temperature, we may infer that the temperature during surgery has had an effect on the occurrence of postanesthetic shivering.
Generally, perioperative body heat loss is believed to be an inevitable occurrence, and as many as 90% of patients in the postoperative period will suffer from hypothermia [12]. A rapid decrease in intraoperative temperature has been observed during the first 30 min of general anesthesia, which coincides with a redistribution of body heat from the core to the periphery that has been mentioned in several studies [131415]. The importance of maintaining normothermia during operations is indisputable. However, a survey on intraoperative temperature management in European hospitals revealed that only 38.5% of patients under general anesthesia had active intraoperative warming devices [16]. Although a warm overlaying mattress is clinically advantageous in application, there are studies recommending a convective heating method using a forced-air warming blanket over a conductive heating method: a warm mattress [717]. Furthermore, both American Society of PeriAnesthesia Nurses (ASPAN) guidelines and National Institute for Health and Care Excellence (NICE) clinical guidelines suggest that any patients undergoing an operation that lasts longer than 30 min should be actively warmed during the operation using a forced-air warming device [14]. Warming of the patient has been stressed in studies such as that of Torossian et al., which recommend that any patient (no prewarming) undergoing general anesthesia lasting longer than 1 h should be actively warmed during the operation [39]. The current intraoperative body temperature management for orthognathic surgery at SNUDH entails the use of a circulating-water mattress, which is considered effective in maintaining body core temperature above 36℃ [17]. The mean duration of orthognathic surgery in the current study was around 7 h, which is longer than the average operating time reported in other studies. SNUDH is a teaching hospital, where young professionals in training learn and acquire skills to perform operations including orthognathic surgery, which may have increased the operating time. With an increase in operating time, the patient is exposed to the cool operating room environment for a longer period, which may have an effect on the intraoperative core temperature.
Depending on the surgical site and method, the body temperature may vary greatly, and a measurement method should be established to reduce error. Torossian et al. have suggested either measuring the temperature from the pulmonary artery or measuring the temperature sublingually [7]. The former method is invasive to practice, and therefore the latter method, which is more convenient to access, can be considered as the measurement site. However, in operations involving the head and neck, sublingual measurement may obstruct the surgical site. In the current study, the temperature was measured from the axillary fossa, which is a reasonable site to estimate core temperature in a well-controlled hospital setting [13].
One common complication of hypothermia is shivering, which increases oxygen consumption, influences surgical outcomes, and may delay hospital inpatient discharge [1314]. A number of classifications are available to assess and grade shivering. The scale used by Singh et al. [18] and Mohta et al. [19], for instance, requires evaluation of the muscular activity of one or more muscle groups, yet with full body coverage of a patient with a blanket in a recovery room, it would be challenging to observe muscular activities. Although the shivering grading used by Casey et al. [20] is simpler to adapt in a clinical environment, in this investigation, shivering was assessed according to the clinical signs of distress to the patient that required medical intervention. The incidence of postanesthetic shivering has been reported to range from 6.3% to 66%, which indicates that a considerable number of patients may experience potentially very unpleasant recovery from anesthesia [21]. About 32% of patients suffered from postanesthetic shivering in this study, which falls within the expected frequency range. From this investigation, the additional use of a forced-air warming blanket not only reduced the incidence of postanesthetic shivering by half, but also reduced the amount of pethidine HCl administered to treat the shivering.
Perioperative hypothermia as a direct cause of postanesthetic shivering has been the subject of debate. Involuntary muscular activities in the absence of hypothermia have been reported, which suggests that postanesthetic shivering has many other contributing factors: uninhibited spinal reflexes, surgical pain, decreased sympathetic activity, and adrenal suppression [522]. Most anesthetic agents decrease vasoconstriction and the shivering threshold [23]. As a result, thermoregulatory shivering is common after surgery [2324]. Additionally, there are studies supporting a high correlation between core temperature during surgery and the incidence of shivering postoperatively [1325]. However, it was not possible to determine the relationship between intraoperative axillary temperature and the incidence of postanesthetic shivering from the information we have investigated. The only significant difference between the shivering and non-shivering groups was the body temperature upon discharge from the recovery room. This might be due to the high use of forced-air warming blankets in order to treat the postanesthetic shivering.
Shivering is one of the least critical complications of perioperative hypothermia; nevertheless, it affects patient recovery outcomes and comfort. To provide the best surgical outcomes, and to increase patient satisfaction and comfort, reducing the incidence of postanesthetic shivering is vital. Although the etiology of postanesthetic shivering in relation to perioperative hypothermia is unclear and controversial, shivering is an inevitable thermoregulatory phenomenon [2627]. Thus, effective preventative measures such as effective maintenance of patient normothermia during surgery should be established. Nonetheless, to reduce the incidence of non-thermoregulatory postanesthetic shivering, further investigation is required.
The possible factors that contribute to postanesthetic shivering were not able to be determined from this study. However, the use of a forced-air warming blanket together with a circulating-water mattress was found to decrease the incidence of shivering during recovery from general anesthesia, and the amount of pethidine used to treat shivering was less in this group. Therefore, this study confirms the benefit of supplementing with a forced-air warming blanket during orthognathic surgery to maintain normothermia and reduce inadvertent postanesthetic shivering.
Figures and Tables
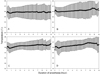 | Fig. 1Mean axillary temperature vs. time starting from induction of anesthesia. A, Group W with no experience of postanesthetic shivering; B, Group W with experience of postanesthetic shivering; C, Group F with no experience of postanesthetic shivering; D, Group F with experience of postanesthetic shivering. Data presented as mean with 5th-95th percentile. The mean temperature pattern for shivering and non-shivering groups resemble each other. The mean axillary temperature of Group F (C and D) was maintained above 36℃ during surgery whereas those in Group W (A and B) declined below 36℃. |
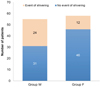 | Fig. 2Number of patients who experienced postanesthetic shivering (P = 0.009, odds ratio = 0.333, 95% confidence interval: 0.147–0.772). |
References
1. Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2013; 45:38–43.
2. Garg M, Cascarini L, Coombes DM, Walsh S, Tsarouchi D, Bentley R, et al. Multicentre study of operating time and inpatient stay for orthognathic surgery. Br J Oral Maxillofac Surg. 2010; 48:360–363.

3. Thomas AA, Rittersma J. Anaesthetic experiences in orthodontic surgery. J Maxillofac Surg. 1978; 6:204–206.

4. Warttig S, Alderson P, Campbell G, Smith AF. Interventions for treating inadvertent postoperative hypothermia. Cochrane Database Syst Rev. 2014; 11:CD009892.

5. Reynolds L, Beckmann J, Kurz A. Perioperative complications of hypothermia. Best Pract Res Clin Anaesthesiol. 2008; 22:645–657.

6. Díaz M, Becker DE. Thermoregulation: Physiological and clinical considerations during sedation and general anesthesia. Anesth Prog. 2010; 57:25–32.

7. Torossian A, Brauer A, Hocker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypothermia. Dtsch Arztebl Int. 2015; 112:166–172.

8. Scott EM, Buckland R. A systematic review of intraoperative warming to prevent postoperative complications. AORN J. 2006; 83:1090–1113.

9. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008; 109:318–338.

10. Casati A, Baroncini S, Pattono R, Fanelli G, Bonarelli S, Musto P, et al. Effects of sympathetic blockade on the efficiency of forced-air warming during combined spinal-epidural anesthesia for total hip arthroplasty. J Clin Anesth. 1999; 11:360–363.

11. Kim HY, Lee KC, Lee MJ, Kim MN, Kim JS, Lee WS, et al. Comparison of the efficacy of a forced-air warming system and circulating-water mattress on core temperature and post-anesthesia shivering in elderly patients undergoing total knee arthroplasty under spinal anesthesia. Korean J Anesthesiol. 2014; 66:352–357.

12. Moola S, Lockwood C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. Int J Evid Based Healthc. 2011; 9:337–345.

13. Insler SR, Sessler DI. Perioperative thermoregulation and temperature monitoring. Anesthesiol Clin. 2006; 24:823–837.

14. NICE. Clinical-practice-guideline, the management of inadvertent perioperative hypothermia in adults. 2008.
15. Tekgul ZT, Pektas S, Yildirim U, Karaman Y, Cakmak M, Ozkarakas H, et al. A prospective randomized double-blind study on the effects of the temperature of irrigation solutions on thermoregulation and postoperative complications in percutaneous nephrolithotomy. J Anesth. 2015; 29:165–169.

16. Torossian A. Survey on intraoperative temperature management in europe. Eur J Anaesthesiol. 2007; 24:668–675.

17. NICE. Inditherm patient warming mattress for the prevention of inadvertent hypothermia. National Institute for Health and Clinical Excellence. 2011.
18. Singh P, Dimitriou V, Mahajan RP, Crossley AW. Double-blind comparison between doxapram and pethidine in the treatment of postanaesthetic shivering. Br J Anaesth. 1993; 71:685–688.

19. Mohta M, Kumari N, Tyagi A, Sethi AK, Agarwal D, Singh M. Tramadol for prevention of postanaesthetic shivering: A randomised double-blind comparison with pethidine. Anaesthesia. 2009; 64:141–146.

20. Casey WF, Smith CE, Katz JM, O'Loughlin K, Weeks SK. Intravenous meperidine for control of shivering during caesarean section under epidural anaesthesia. Can J Anaesth. 1988; 35:128–133.

21. Alfonsi P. Postanaesthetic shivering: Epidemiology, pathophysiology, and approaches to prevention and management. Minerva Anestesiol. 2003; 69:438–442.
22. Sessler DI, Rubinstein EH, Moayeri A. Physiologic responses to mild perianesthetic hypothermia in humans. Anesthesiology. 1991; 75:594–610.

23. Leslie K, Sessler DI. Perioperative hypothermia in the high-risk surgical patient. Best Pract Res Clin Anaesthesiol. 2003; 17:485–498.

24. Horn EP, Sessler DI, Standl T, Schroeder F, Bartz HJ, Beyer JC, et al. Non-thermoregulatory shivering in patients recovering from isoflurane or desflurane anesthesia. Anesthesiology. 1998; 89:878–886.

25. Lienhart A, Fiez N, Deriaz H. Postoperative shivering: Analysis of main associated factors. Ann Fr Anesth Reanim. 1992; 11:488–495.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download