Abstract
Airway difficulties are a major concern for anesthesiologists. Even though fiberoptic intubation is the generally accepted method for management of difficult airways, it is not without disadvantages-requires patient cooperation, and cannot be performed on soiled airway or upper airways with pre-existing narrowing pathology. Additionally, fiberoptic bronchoscopy is not available at every medical institution. In this case, we encountered difficult airway management in a 71-year-old man with a high Mallampati grade and a thick neck who had undergone urologic surgery. Several attempts, including a bronchoscope-guided intubation, were unsuccessful. Finally, blind nasal intubation was successful while the patient's neck was flexed and the tracheal cartilage was gently pressed down. We suggest that blind nasal intubation is a helpful alternative in difficult airway management and it can be a lifesaving technique in emergencies. Additionally, its simplicity makes it a less expensive option when advanced airway technology (fiberoptic bronchoscopy) is unavailable.
Airway difficulties during induction of general anesthesia are a concern for anesthesiologists. The incidence of difficult intubations has been reported to be 5.8%-6.2% in patients who have undergone general surgery [1]. Even though fiberoptic intubation is the generally accepted method for management of difficult airways, it is not without disadvantages-requires patient cooperation, and cannot be performed on soiled airway or upper airways with pre-existing narrowing pathology [2]. Furthermore, fiberoptic bronchoscopy is not available at every medical institution, especially small and medium-sized hospitals. The 2013 Practice Guidelines for Management of the Difficult Airway from the American Society of Anesthesiologists (ASA) recommends use of alternative approaches in cases of difficult or unsuccessful intubations [3]. Blind nasal intubation is a readily available technique for management of difficult airways, such as those in patients with a restricted mouth opening or damaged teeth [4]. Herein, we present a case of blind nasal intubation used as an alternative, albeit difficult, intubation approach on a patient with a high Mallampati grade and a thick neck.
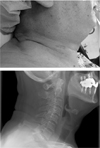
This patient gave informed consent for publication of this case via telephone. A 71-year-old man (weight, 74 kg; height, 171 cm) was scheduled for robotic-assisted laparoscopic prostatectomy. According to his medical history, he had diabetes mellitus that was being treated with medication. The results of his preoperative laboratory tests, electrocardiogram, and chest X-rays were unremarkable. On his pre-anesthetic airway evaluation, difficult airway was predicted due to modified Mallampati test grade of 3, a large tongue, and a 48-cm neck circumference (Fig. 1).
In the surgical suite, electrocardiogram, noninvasive blood pressure monitoring, and pulse oximetry were performed. General anesthesia was induced using 375 mg thiopental sodium. After confirmation that bag mask ventilation was adequate using the two-handed technique, we planned to intubate the patient's trachea after muscle relaxation was induced using 50 mg rocuronium. Mask ventilation using desflurane in 100% oxygen was administered and the target-controlled infusion of remifentanil was simultaneously started at a target Ce of 2 ng/ml until full muscular relaxation was achieved. Despite the fact that a McGrath MAC video laryngoscope (Aircraft Medical, Edinburgh, UK) with blade 4 was easily inserted and exposed the epiglottis, although not the vocal cords, attempts to insert the styletted tracheal tube were unsuccessful. In accordance with the practice guidelines for management of difficult airways [3], we attempted intubation using a light wand (Lighted Stylets, Bovie Medical Corporation, Purchase, NY) that was hockey stick-shaped. A well-defined circumscribed glow presented slightly below the thyroid prominence in the anterior neck, although there was resistance when advancing the tracheal tube through the trachea. As an alternative approach to difficult intubations, a 7-mm internal diameter, cuffed nasotracheal tube was inserted through the patient's nostril into the oropharynx. A fiber bronchoscope (Olympus Corporation, Tokyo, Japan) was passed through the nasotracheal tube into the oropharynx; however, we were unable to identify the epiglottis and vocal cords due to the presence of bloody secretions. For blind nasal intubation, a nasotracheal tube was inserted while the patient's head was extended, the neck was flexed, and the tracheal cartilage was gently pressed down. Finally, nasotracheal introduction of the nasotracheal tube was confirmed via bilateral lung auscultation and capnography. Surgery was completed without adverse events and the patient's trachea was extubated after the neuromuscular blocking effects were reversed using 150 mg sugammadex.
Difficult airways are a major concern for anesthesiologists. Difficulties with tracheal intubation greatly contribute to morbidity and mortality associated with anesthesia [1]. The definition of a difficult airway is a clinical situation in which a conventionally trained anesthesiologist has difficulty ventilating a patient using a facemask or tracheal tube. Incidence of difficult laryngoscopies and difficult mask ventilation during surgery are estimated to be 4.4% and 2.5%, respectively [5]. This approach is based on an updated report from the ASA Task Force on Management of the Difficult Airway [3]. Difficulties with tracheal intubation significantly contribute to airway damage, cardiorespiratory arrest, hypoxic brain injury, unnecessary tracheostomy, and death associated with anesthesia.
Pre-anesthetic evaluation in order to recognize potentially difficult airways is intended to decrease morbidity and mortality related to airway management. Reviewing patient medical records and establishing medical histories are the first steps in the safe control of airways. Physical examination of the anatomical features of the head and neck is useful for detecting physical characteristics that may indicate presence of a difficult airway. It is also important to know how to use equipment and alternative approaches to guarantee patient safety during unsuccessful intubations.
Gonzalez et al. reported that difficult intubations are associated with neck circumference > 43 cm, a Mallampati score ≥ 3, and high body mass index [6]. If initial intubation attempts are unsuccessful after induction of general anesthesia, it is important to request an additional individual who is immediately available to assist in managing the difficult airway. While conducting the facemask ventilation with oxygen, alternative approaches to intubation should be considered. Alternative difficult intubation approaches include video-assisted laryngoscopy, a laryngoscope blade with a flexible tip, a supraglottic airway as an intubation conduit, fiberoptic intubation, a light wand, blind oral intubation, and nasal intubation [3].
For patients with whom tracheal intubation is either difficult or impossible, blind nasal intubation has become an accepted method for securing an airway. Blind nasal intubation usually does not require availability of a special device [7] or appropriate operator training. Blind nasal intubation is also a viable option for patients who are awake. An additional advantage is that presence of blood and secretions do not increase difficulty in blind nasal intubation. This is a technique frequently used by paramedics in out-of-hospital patient care. The average success rate for paramedics using the blind nasotracheal method is 58.0%-72.2% with conventional endotracheal tubes [8910].
The nasal mucosa should be gently prepared with nasal mucosal vasoconstrictors and local anesthetic agents, especially on awake patients. The patient's head and neck, if not contraindicated, are then placed in the sniffing position. The endotracheal tube should be lubricated and passed along the floor of the nose beneath the inferior turbinate [11]. Breathing sounds are confirmed and then the tube is advanced into the trachea through the glottis. If unsuccessful, the patient's head is repositioned and the tube is facilitated via optimal external laryngeal manipulation [12]. Skill of the physician performing the blind nasal intubation is the main determinant for success. Average success rate was 71.3% for participating paramedics who previously attempted blind nasal incubation fewer than 4 times [8]. Success rate increased to 86.0% when using the Endotrol (Mallinckrodt, Hazelwood, MO) endotracheal tube [13]. Use of a Beck Airway Airflow Monitor (Great Plains Ballistics, Lubbock, TX) whistle can facilitate blind nasal intubation [14]. Improved success rate of blind nasal intubation was also achieved by inflating the tracheal tube cuff in order to elevate the tip of the tube [15].
Although blind nasal intubation has been shown to be an effective alternative for the management of difficult airways, its potential risks and complications must be kept in mind. Subluxation of the cricoarytenoid cartilage and damage to the glottic opening occur rarely during endotracheal intubation using a "nonvisualizing" intubating technique. Blind insertion of endotracheal tube frequently leads to esophageal intubation. In some instances, the epiglottis is pushed into the glottic opening. Usually, these changes are spontaneously reversed and do not cause permanent damage [2].
Despite the multitude of available airway management techniques, blind nasal intubation remains a helpful alternative in difficult airway management and can be a lifesaving technique in emergencies. Additionally, its simplicity ensures that it is a less expensive option in locations where advanced airway technology, such as fiberoptic bronchoscopy, is unavailable.
References
1. Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005; 103:429–437.
2. Hagberg CA. Benumof and Hagberg's airway management. 3rd ed. Philadelphia: Elsevier Inc.;2013. p. 403–441.
3. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013; 118:251–270.
4. Finucane BT, Tsui BC, Santora AH. Principles of airway management. 4th ed. St. Louis: Mosby;2011. p. 355.
5. Kheterpal S, Healy D, Aziz MF, Shanks AM, Freundlich RE, Linton F, et al. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology. 2013; 119:1360–1369.

6. Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth Analg. 2008; 106:1132–1136.

7. Zhang J, Lamb A, Hung O, Hung C, Hung D. Blind nasal intubation: teaching a dying art. Can J Anaesth. 2014; 61:1055–1056.

8. O'Brien DJ, Danzl DF, Hooker EA, Daniel LM, Dolan MC. Prehospital blind nasotracheal intubation by paramedics. Ann Emerg Med. 1989; 18:612–617.
9. Dronen SC, Merigian KS, Hedges JR, Hoekstra JW, Borron SW. A comparison of blind nasotracheal and succinylcholineassisted intubation in the poisoned patient. Ann Emerg Med. 1987; 16:650–652.

10. O'Connor RE, Megargel RE, Schnyder ME, Madden JF, Bitner M, Ross R. Paramedic success rate for blind nasotracheal intubation is improved with the use of an endotracheal tube with directional tip control. Ann Emerg Med. 2000; 36:328–332.
11. Hagberg CA, Artime CA. Ariway management in the adult. In : Miller RD, editor. Miller's anesthesia. 8th ed. Philadelphia: Elsevier/Saunders;2015. p. 1670.
12. Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996; 8:136–140.

13. Hooker EA, Hagan S, Coleman R, Heine MF, Greenwood P. Directional-tip endotracheal tubes for blind nasotracheal intubation. Acad Emerg Med. 1996; 3:586–589.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download