Abstract
Background
Dental injury as a result of oroendotracheal intubation during general anesthesia is very common. We report our experiences of using mouthguard to prevent dental injury during intubation based on our protocol.
Methods
This retrospective study enrolled patients referred for preanesthetic evaluation, those patients with a history of any of the dental treatments to their anterior teeth listed on our fabrication protocol from January 1, 2009 to June 30, 2010.
Results
No cases of dental trauma during oroendotracheal intubation were reported among the 202 patients who used a protective device. 66% of the patients had risk factors for hard tissue damage aged 10-40 years. At the ages of 40-70 years, the incidence of risk group for periodontal damage was higher.
Endotracheal intubation refers to the placement of a flexible plastic tube into the trachea via the mouth, larynx, and vocal cords, in order to protect the patient's airway and provide mechanical ventilation [1,2,3]. Two types of intubation are commonly used: oroendotracheal and nasoendotracheal. In most cases oroendotracheal intubation is the procedure of choice, except for surgery on the mouth and oropharynx. Damage to the teeth during general anesthesia via oroendotracheal intubation is very common. This complication, which is embarrassing to anesthesiologists, occurs with a reported incidence of 0.17-12.1% [1,3,4,5,6,7,8]. This occurs mainly due to misuse of the laryngoscope. However, even experienced anesthesiologists can experience this when patient has potential risk factors such as pathologically weakened teeth. The recent expansion of the esthetics field of dentistry has resulted in an increase in the number of anterior teeth treated with tooth-colored restorations, including porcelain veneers, resin, and porcelain fused to metal restorations. These materials provide esthetically excellent results for patients; however, they are much more brittle than natural teeth. The risk of dental injury is higher in these patients, but the esthetic restoration is often very difficult to distinguish from the natural tooth.
Preanesthetic history taking and physical examination can prevent dental injury. Even though an anesthesiologist's can perform a thorough preanesthetic evaluation, the taking of a complete dental history is beyond the scope of the unfamiliar anesthesiologist. Dental consultations before general anesthesia could be an option for the prevention of dental injury during surgery; however, this is very bothersome step for both the anesthesiologist and the patient. A definitive guideline for the anesthesiologist regarding the requirement of a dental consultation would be an efficient way of reducing dental complications during oroendotracheal intubation under general anesthesia.
We present herein our experience of providing a protective device for the prevention of dental injury during oroendotracheal intubation under general anesthesia, and provide useful guidelines for anesthesiologists for use during their preanesthetic patient evaluation to help them to determine whether they should be referred for a dental consultation prior to surgery.
We enrolled in this study all of those patients who visited the Department of Advanced General Dentistry for the fabrication of a protective dental splint to prevent dental injury during general anesthesia under oroendotracheal intubation between January 1, 2009 and June 30, 2010.
During preanesthetic evaluation by the operation coordinator, those patients with a history of any dental treatment to their anterior teeth (from central incisor to second premolar) listed on our fabrication guidelines were dental trauma during oroendotracheal intubation under general anesthesia, they were advised of their need for a dental splint. The detail clinical pathway and fabrication guidelines are given in Fig. 1, 2 and Table 1.
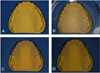
With the patient's agreement, an individualized protective dental device was fabricated (Fig. 3). First, a dental impression was taken using irreversible hydrocolloid materials (Alginoplast, Hanau, Germany), and then an individualized dental cast model was fabricated with improved dental stone (Hi-Koseton, Osaka, Japan). After trimming the irregular surfaces of the dental model (Fig. 3A), 3-mm-thick thermoplastic sheet (Bioplast, Iserlohn, Germany) was fitted to the dental cast (Fig. 3B) and trimmed to cover the ten anterior teeth (from the right second premolar to left second premolar), including 2 mm of the subgingival area (Fig. 3C). Small holes were then made on both sides between the canine and first premolar, and a 15-cm-long piece of dental floss was tied through the hole (Fig. 3D). Each mouthguard took about 1 hour to fabricate. Fig. 3 shows the mouthguard before (Fig. 4A) and after (Fig. 4B) delivery to a patient. The protective device was delivered to the patient on the hospital admission date, which was usually the day before the operation.
We analyzed the demographic data of the patients, and took details of the department where the consultation was made and the kind of operation that the patients were due to undergo. The reasons for fabricating a dental splint were also evaluated using the demographic data. Additional dental treatments, such as tooth extraction or dental scaling, were reviewed. Using the patients' electronic medical charts, we sought any complication during general anesthesia after the use of a dental splint.
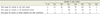
This study enrolled 202 patients (43 males and 159 females) between January 1, 2009 and June 30, 2010. The distributions of age and consulting departments are presented in Fig. 5 and Table 2. The number of patients having each risk factor (as evaluated by clinical and radiographic examinations) is listed in Table 3. In 17 patients, "hopeless" teeth were removed because it was decided that these could not be protected from dislodgement or exfoliation by a mouthguard. Other additional dental treatments included dental scaling and operative treatment. No cases of dental trauma during oroendotracheal intubation were reported with the use of protective devices in the 202 patients (as ascertained from a review of their electronic medical charts).
Dental injury caused by endotracheal intubation during general anesthesia is a common complication [3,4,9], with a reported incidence of between 0.17% and 12.1% [2,3,4,5,6,7,8]. According to a nationwide survey conducted by Lockhart et al. in 1986, 1 dental injury occurred in every 1,000 endotracheal intubations [3]. Furthermore, dental injury was the most frequently reported claim in a review of medicolegal claims against anesthetists associated with the Medical Defence Association of Victoria, Melbourne, Australia [10]. Newland et al. [11] reported that the incidence of dental injury was 1 per 2,073 cases of anesthesia; 86% of dental injuries were discovered by anestheologist. The most frequently injured teeth were the maxillary incisors, with the risk being much higher (approximately 20-fold) in patients with poor dentition or reconstructive work. The incidence does not appear to differ significantly with age, gender, American Society of Anesthesiologists physical status, airway management, or incidence of obesity. Givol et al. [2] reported that the major risk factor for dental injury was preexisting poor dentition, and a second risk factor was intubation difficulty.
It is recommended that patients with a risk factor for dental injury during intubation be screened by a dental practitioner before undergoing surgery [12]. However, it is time consuming and difficult for an anesthesiologist to distinguish which cases require such a dental consultation. Following the critical pathway we have presented herein allowed us to screen a patient according to each risk group before surgery, and fabricate the equipment needed to protect that patient from dental injuries during intubation. One factor that distinguishes our study from previous studies is that we divided dental risk into three groups as described below: hard tissue, periodontal tissue, and implants.
The first risk group (injuries to the hard tissue) refers to tooth fracture or the presence of prostheses. This risk group represented 65% of all cases in our study. Teeth that are decayed or have prosthetics are weaker than sound teeth, and have a greater risk of fracture. Moreover, non-vital or root-canal-treated teeth are also weak, and thus need a protective device. Pathologically weakened teeth can readily be injured by small tensile force, and therefore more caution is needed for these teeth, which are costly to replace.
The second risk group refers to injuries to the periodontal tissue. This risk group represented 28% of all cases in our study. Teeth are easier to dislodge when the bony support of the tooth is lost due to periodontal disease. The incidence of periodontal disease is higher in older patients, so assessment of the periodontal tissue is important. Of the referred patients, 74% were in 40s, 50s, and 60s, and the proportion of risk to the periodontal tissue in all three risky groups was 85%. Patients with periodontal disease may have tooth mobility or gingival recession, in which tooth luxation or avulsion can occur due to the periodontal damage.
It may be better to extract than to save hopeless teeth. After preanesthetic dental assessment, we extracted 17 hopeless teeth, thus preventing exfoliation and possible subsequent inhalation of a tooth into their airways during intubation. Patients with a history of orthodontic treatment also need to be cautioned, since teeth can fall out due to the root resorption and consequent increased mobility. Moreover, patients who have a history of tooth trauma may have tooth and root-structure problems. For example, they may have a shortened root and weakened tooth structure. Therefore, a mouthguard is needed during intubation to protect these teeth.
The third risk group refers to dental implants and their prostheses. This risk group represented 7% of all cases in our study. With regard to the type of damage incurred, the implant group can be divided into damage of the superstructures of prosthesis and damage of implant fixture and surrounding bones. Dental implant treatment has recently become popular because it helps to maintain sound adjacent teeth and is a fixed-type treatment, thus reducing the discomfort associated with removable prostheses. Even with successful osseointegration, implants are naturally weak against lateral forces, and so they need to be protected. Moreover, since successful implants may be difficult to distinguish from natural teeth and damage to them will prove costly, dentists must take care to examine a patient's dentition very carefully prior to surgery.
The rationale underlying the use of a mouthguard during oroendotracheal intubation differs with the patient's age. In neonates, the damage caused by oroendotracheal intubation may cause abnormal development of the underlying teeth, and deciduous teeth in young children have shallow roots and are easy to dislodge and exfoliate, especially between the ages of 5 and 9 years [1,13]. In the current cohort, 66% of the patients in the hard-tissue risk group were aged 10-40 years. At these ages, hard-tissue risk factors such as dental caries, restorations, and prostheses represent the greatest risks. At ages 40-70 years, the risks of all three types of damage (i.e., hard tissue, periodontal tissue, and implants) were high (Table 4). This age group has cumulative preexisting hard-tissue risk factors such restorations and prostheses, and a high incidence of periodontal disease leading to missing teeth, so the frequency of implant treatment is high. At ages > 70 years, the risk of periodontal disease was relative high.
Several methods of preventing dental injury have been introduced by anesthesiologists to reduce oroendotracheal-intubation-induced trauma, such as adhesive plaster [14], gauze rolls, and folded tape [4], but these do not provide protection against levering forces. Other methods include using a transformed blade [15], the left molar approach for laryngoscopy to spare the incisor teeth [16], or preformed or individualized tooth protectors [17]. Methods such as transforming a blade or intubating in a different direction have limitations regarding the adequate protection of a patient's teeth and periodontal tissues; however, the mouthguard can cover and protect the teeth from trauma. Implementing a preformed mouthguard can be rapid and convenient, but individual adaptation may be limited or impossible to achieve. Individualized tooth protectors have the greatest adaptability and are the most definitive way of protecting the teeth.
The requirements of a protective device include easy manipulation, effective protection to risky teeth, and stability (to prevent aspiration). Even though various materials are available, we used 3-mm-thick Bioplast film because it is easy to manipulate, clear, and flexible, and hence easy to apply. It can also be used several times within a short time period. A mouthguard can be fabricated from this material by taking a single, irreversible, hydrocolloid impression without any patient discomfort. The simple manipulation method and convenient delivery is advantageous to the medical team. Patients who were referred to our dental department following the critical pathway guidelines received clinical and radiographic examinations. The dentist screened the patients by following the risk-group guidelines and subsequently fabricated an individualized mouthguard. Any teeth diagnosed with localized advanced periodontitis were extracted before surgery since these are difficult to protect using only one such protective device. However, our pathway is subject to some limitations. It is effective only when there is a special operative coordinator who can guide the clinical pathway prior to surgery. Patients must visit the dental clinic twice and pay the additional costs associated with obtaining an x-ray and fabricating a mouthguard. We informed patients about the possibility of dental injuries and the necessity of a preanesthetic dental evaluation, and all of the patients consented to participate without any complaint.
In conclusion, it is not easy for the anesthesiologist to evaluate risk factors such as poor dentition and reconstructive work and to fabricate protective mouthguard; thus, the most reliable and practical method is a preanesthetic dental consultation. The reasons for constructing such a protective device differ with the patient's age, a fact that the operative coordinator should be aware of. Particularly careful attention should be paid to multiply rehabilitated patients and those with poor oral hygiene. Our pathway could help to prevent dental injury due to oroendotracheal intubation under general anesthesia.
Figures and Tables
ACKNOWLEDGEMENT
This study was supported by a faculty research grant of Yonsei University College of Dentistry for 2011 (6-2011-0053).
References
1. Chen JJ, Susetio L, Chao CC. Oral complications associated with endotracheal general anesthesia. Anaesthesiologica Sinica. 1990; 28:163–169.
2. Givol N, Gershtansky Y, Halamish-Shani T, Taicher S, Perel A, Segal E. Perianesthetic dental injuries: Analysis of incident reports. J Clin Anesth. 2004; 16:173–176.

3. Lockhart PB, Feldbau EV, Gabel RA, Connolly SF, Silversin JB. Dental complications during and after tracheal intubation. J Am Dent Assoc. 1986; 112:480–483.

4. Burton JF, Baker AB. Dental damage during anaesthesia and surgery. Anaesth Intensive Care. 1987; 15:262–268.

5. Deppe H, Reeker W, Horch HH, Kochs E. Tooth injury during intubation--diagnostic and therapeutic aspects. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998; 33:722–725.
6. Folwaczny M, Hickel R. Oro-dental injuries during intubation anesthesia. Anaesthesist. 1998; 47:707–731.
7. Magnin C, Bory EN, Motin J. Tooth injuries during intubation: a new preventive device. Ann Fr Anesth Reanim. 1991; 10:171–174.
8. Warner ME, Benenfeld SM, Warner MA, Schroeder DR, Maxson PM. Perianesthetic dental injuries: Frequency, outcomes, and risk factors. Anesthesiology. 1999; 90:1302–1305.

9. Owen H, Waddell-Smith I. Dental trauma associated with anaesthesia. Anaesth Intensive Care. 2000; 28:133–145.

10. Cass NM. Medicolegal claims against anaesthetists: A 20 year study. Anaesth Intensive Care. 2004; 32:47–58.

11. Newland MC, Ellis SJ, Peters KR, Simonson JA, Durham TM, Ullrich FA, et al. Dental injury associated with anesthesia: A report of 161,687 anesthetics given over 14 years. J Clin Anesth. 2007; 19:339–345.

12. Chadwick RG, Lindsay SM. Dental injuries during general anaesthesia. Br Dent J. 1996; 180:255–258.

13. Hagelsten JO, Marvitz L. Prevention of dental damage during anesthesia. Z Prakt Anasth. 1971; 6:195–205.
14. Ghabash MB, Matta MS, Mehanna CB. Prevention of dental trauma during endotracheal intubation. Anesth Analg. 1997; 84:230–231.





 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download