Abstract
The difficult oral healthcare in intellectually disabled patients with poor behavioral control has led to debate over the cost-effectiveness and validity of implant treatment in these patients. The patient in the present report had schizophrenia that had led to poor oral care and severe dental caries in the full mouth. Tooth extraction and a removable prosthesis were planned, but the guardian wanted an implant procedure. Since the guardian showed strong will and cooperation with regard to the patient's oral healthcare, extraction followed by immediate implant placement was performed across two rounds of general anesthesia. Since the outcome appears successful, we present this case report. Immediate implant placement after tooth extraction requires fewer surgeries and rounds of general anesthesia, reduces horizontal bone resorption, and can achieve better esthetic results. Therefore, as long as a certain degree of oral care is possible, this can be a positive option for restoration of a partially edentulous mouth, even in intellectually disabled patients.
In a large number of patients with neurologic disabilities, a lack of behavioral control leads to poor dental health. Especially schizophrenic patients have false beliefs, confused thinking, hallucinations, reduced emotional expression, and lack of motivation. The support and concern of their family play key role in maintaining medical and dental health status. In order to prevent cavities and periodontal disease, these patients require regular dental examinations and help from family members. However, when this is not possible, many patients that do visit the dentist undergo tooth extraction for multiple irreparable teeth and require prosthodontic restoration. Generally, in disabled patients, a removable prosthesis is placed after tooth extraction. This approach is used because implant supported prostheses are expensive and require multiple rounds of surgery under general anesthesia due to difficulties with behavioral control, and because they show reduced therapeutic efficacy, relative to cost, if implant failure occurs due to a lack of care after placement. However, immediate implant placement after tooth extraction allow minimization of the number of surgeries and rounds of general anesthesia, so when postoperative care can be guaranteed to some extent, this may be one treatment option. Furthermore, cases of implant-supported prostheses have been reported recently in various neurologic disability patients, and are showing a high success rate [123].
In 2004, at the ITI consensus conference, 4 types of implant placements were distinguished according to timing. Type 1 refers to immediate placement after tooth extraction, while Type 2 refers to placement performed 4-8 weeks after extraction, following healing of the soft tissue. Type 3 refers to placement 12-16 weeks after extraction, and Type 4 refers to placement 6 months after extraction, when complete healing has occurred. Of these, immediate implant placement refers to placement performed immediately after extraction, without waiting for healing of the soft or hard tissue. In spite of the advantage of being able to reduce the number of surgeries, there has previously been considerable debate about immediate implant placement, due to concerns about the implant success rate, esthetic outcomes, and preservation of the alveolar bone. Nevertheless, the current success rate for immediate implant placement is approximately 95% [4], which is similar to other types of implant placements. The esthetic risk is low for thick tissue biotypes [5], and although immediate implant placement cannot prevent horizontal and vertical resorption of the alveolar bone [678], when it is accompanied by a bone graft during surgery, horizontal resorption can be reduced and esthetic outcomes can be improved [9].
The present case report is of a patient requiring prosthodontic restoration after extraction of a large number of teeth. The initial treatment plan was for dentures, but the guardian wanted implant supported prosthesis and so, following an explanation of the pros and cons, expenses, and the guardian's responsibility for postoperative oral hygiene care, the treatment plan was changed with the guardian's consent. The surgery was performed across several rounds of outpatient general anesthesia, and the outcome was successful. Hence, we report this case with the consent of the patient's guardian.
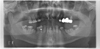
The patient was male, 62 years old, 180 cm in height, and with a body weight of 90 kg. He was taking anti-schizophrenic drugs and thyroid hormone treatment for schizophrenia that started 30 years earlier, and hypothyroidism discovered 1 year earlier. The patient first visited the present hospital on 13th June 2014 and required extraction of a large number of teeth and treatment for dental caries. Treatment cooperation was low due to the schizophrenia, and 2 rounds of treatment under general anesthesia were planned, with a team consisting of specialists in prosthodontics, conservative dentistry, and oral & maxillofacial surgery (Fig. 1). On the initial examination, a treatment plan of dentures following tooth extraction was established, but the guardian wanted a fixed prosthesis using an implant. After an explanation of the pros and cons of treatment, the costs, and the responsibility of the guardian for postoperative oral hygiene care, the treatment plan was changed with the guardian's consent.
In the preanesthetic assessment, the patient showed slight findings of hypothyroidism (T3, 67 ng/dl; free T4, 1.17 ng/dl; and TSH, 4.39 µIU/ml). However, liver and kidney function were normal. The patient's overall responses were slow, he showed apathetic behaviors, and he was capable of activity using a wheelchair.
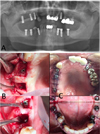
On 23rd October 2014, the patient was admitted after 8 hours of fasting, and total intravenous anesthesia was performed using propofol and remifentanil. Extraction of teeth #11, 12, 14, 15, 16, 17, 24, 34, 36, 37, 38, 44, 46, and 47, and immediate implant placement at locations #14 (4.0*10.0 mm), 24 (4.0*10.0 mm), 34 (4.5*10.0 mm), 44 (4.5*10.0 mm), 46 (5.0*8.5 mm), and 47 (5.0*8.5 mm) were performed under general anesthesia (Fig. 2). One week later, general anesthesia was performed by the same method, followed by extraction of tooth #35 and implant placement at locations #15 (4.5*10.0 mm), 17 (4.5*8.5 mm), 35 (4.5*10.0 mm), and 37 (4.5*10.0 mm). In the case of the 2nd left mandibular molar and the 1st and 2nd right mandibular molars, the implant was placed in the septum, which had been carefully preserved during extraction. Here, because the distance from the buccal alveolar bone was over 2 mm (approximately 3 mm) [69], a graft was performed with xenogenic bone (Bio-Oss, Geistlich) (Fig. 3). During implant placement, in order to place the mandibular and maxillary implants in the ideal position so that their path would not impair occlusion, guide pins were used to check the antagonistic relationships persistently. All implants were OSSTEM TS III SA, and across the two rounds of surgery, a total of 16 teeth were extracted and 10 implants placed. The patient visited the hospital as an outpatient every 2-4 days until soft tissue healing in order to dress a wound. Approximately 6 months after the first operation (Fig. 4), the patient underwent a third round of general anesthesia for the second operation (Fig. 5). No implant failure was detected during the second operation, and the patient is currently undergoing implant loading with no failures observed.
Like most patients with mental retardation, schizophrenia patients show poorer dental health than typical individuals [10]. Thus, for the same reason, when implants are placed in disabled patients with poor oral hygiene care, the risk of failure is high, and in such cases, the benefits of surgery under general anesthesia are debatable. As a result, implant treatment is contraindicated in some disabled patients. However, in reality, as long as oral hygiene care is not neglected, implant treatment can be a positive option for disabled patients [1112]. For the patients in the present study, schizophrenic symptoms had been mild for several years, plaque control was also favorable, as was cooperation for general dental treatment. However, schizophrenic symptoms had become more severe recently, and the patient had been admitted to a closed ward, during which time oral care had been mostly neglected, leading to a rapid decline in oral health. In this case, the guardian showed very good cooperation, and a strong will for treatment and taking responsibility for the patient's oral care after treatment. Therefore, it was determined that implant placement in this patient was not unconditionally contraindicated, and could be a possible treatment option. After close consultation with the Prosthodontics Department, a treatment plan for immediate implant placement after tooth extraction was established in order to reduce the number of rounds of general anesthesia. Generally, in immediate implant placement, a satisfactory outcome can be achieved as long as the following conditions are satisfied: 1) intact socket walls, 2) facial bone wall at least 1 mm in thickness, 3) thick soft tissue, 4) no acute infection at the site, and 5) availability of bone apical and palatal to the socket to provide primary stability [13]. In the present case, a number of teeth had deteriorated because of caries, but the state of the alveolar bone was favorable and the above conditions were satisfied.
Thus, as long as cases are selected carefully, immediate implant placement after tooth extraction may be a good treatment option for disabled patients, making it possible to reduce the number of surgeries and rounds of general anesthesia, and to achieve predictable, esthetically satisfactory outcomes.
Figures and Tables
Fig. 2
A: Panoramic view of implant after the first operation (2014.10.24), B: After extraction, C: After implant placement.

Fig. 3
A: Panoramic view of implant after the first operation (2014.10.30), B: After implant placement - right maxilla, C: After implant placement - left mandible.

References
1. Jackowski J, Dent DM, Andrich J, Kdppeler H, Zöllner A, Jöhren P, et al. Implant-supported denture in a patient with huntington's disease: Interdisciplinary aspects. Spec Care Dentist. 2001; 21:15–20.

2. Lustig JP, Yanko R, Zilberman U. Use of dental implants in patients with Down syndrome: A case report. Spec Care Dentist. 2002; 22:201–204.

3. Ekfeldt A. Early experience of implant-supported prostheses in patients with neurologic disabilities. Int J Prosthodont. 2004; 18:132–138.
4. Quirynen M, Van Assche N, Botticelli D, Berglundh T. How does the timing of implant placement to extraction affect outcome. Int J Oral Maxillofac Implants. 2007; 22:203–223.
5. Kois JC. Predictable single-tooth peri-implant esthetics: Five diagnostic keys. Compend Contin Educ Dent. 2004; 25:895–896.
6. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004; 31:820–828.

7. Chen ST, Wilson TG Jr, Hammerle CH. Immediate or early placement of implants following tooth extraction: Review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004; 19:12–25.
8. Covani U, Bortolaia C, Barone A, Sbordone L. Buccolingual crestal bone changes after immediate and delayed implant placement. J Periodontol. 2004; 75:1605–1612.

9. Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implants. 2009; 24:Suppl. 186–217.
10. McCreadie RG, Stevens H, Henderson J, Hall D, McCaul R, Filik R, et al. The dental health of people with schizophrenia. Acta Psychiatr Scand. 2004; 110:306–310.

11. Lopez-Jimenez J, Romero-Dominguez A, Gimenez-Prats MJ. Implants in handicapped patients. Med Oral. 2003; 8:288–293.
12. Oczakir C, Balmer S, Merickse-Stern R. Implantprosthodontic treatment for special care patients: A case series study. Int J Prosthodont. 2005; 18:383.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download