Abstract
Background
Identifying early markers of septic complications can aid in the diagnosis and therapeutic management of hospitalized patients. In this study, the utility of procalcitonin (PCT) vs. C-reactive protein (CRP) as early markers of sepsis was compared.
Methods
A series of 2,697 consecutive blood samples was collected from hospitalized patients and serum PCT and CRP levels were measured. Patients were categorized by PCT level as follows: < 0.05 ng/ml, 0.05-0.49 ng/ml, 0.5-1.99 ng/ml, 2-9.99 ng/ml, and > 10 ng/ml. Diagnostic utility was analyzed by receiver operating characteristic (ROC) curves.
Results
Mean CRP levels varied among the five PCT categories at 0.31 ± 2.87, 5.65 ± 6.26, 13.78 ± 8.01, 12.15 ± 10.16, and 17.77 ± 10.59, respectively (P < 0.05). PCT and CRP differed between positive and negative blood culture groups (PCT: 15.9 vs. 4.78 mg/dl; CRP: 11.5 ng/ml vs. 9.57 ng/ml; P < 0.05). The areas under the ROC curves (PCT, 95% confidence interval [CI]: 0.743, range: 0.698-0.789 at a threshold of 0.5 ng/ml; CRP, 95% CI: 0.540, range: 0.478-0.602 at a threshold of 8 mg/l) differed for PCT and CRP (P < 0.05).
Infection is a major complication in hospitalized and post-surgical patients that greatly impacts patient outcome and increases healthcare costs for society. However, the clinical distinction between minor infection and sepsis is not always apparent, making diagnosis difficult at early stages. For example, systemic inflammatory response syndrome (SIRS) with fever frequently occurs in hospitalized patients in the absence of an infection. SIRS can be self-limiting or may progress to severe sepsis or septic shock in some cases [1]. As such, an accurate and timely diagnosis of infection vs. sepsis and the implementation of adequate treatment are essential. The identification of early specific and sensitive biomarkers of SIRS or sepsis can aid in this regard. Although blood cultures are currently the best method for diagnosing an infection, they are not universally informative. Furthermore, cytokines such as interleukin (IL)-6 and -8 have been shown to be associated with sepsis severity and patient outcome, but are not established tools for diagnosis and clinical decision-making [23]. On the other hand, C-reactive protein (CRP) is a commonly used marker for detecting infection that is highly sensitive and convenient forclinical follow-up, but has only limited specificity.
Procalcitonin (PCT) is a recently identified marker of inflammation and infection. The The 116-amino acid PCT protein issynthesized and secreted by thyroid C cells as a precursor of calcitonin in humans; however, PCT levels are increased in sepsis from an extrathyroidal origin [45] and are markedly elevatedduring severe infection and endotoxemia [67]. PCT is detectable after infection following an increase in the levels of proinflammatory cytokines such as tumor necrosis factor-α or IL-6, with high levels maintained from 8 to 24 h, after which levels return to baseline values more rapidly than that of CRP [8].
This study evaluatedthe diagnostic value of PCT as an early marker of infection and compared PCT and CRP in terms of their ability to predict sepsis based on the results of blood cultures.
We retrospectively analyzed 2,697 consecutive blood samples obtained from hospitalized patients at a Dankook University Hospital between January 2014 and December 2014 who had undergone laboratory tests for the measurement PCT and CRP levels. This study was approved by our hospital ethics committee,and informed consent was waived owing to the nature of retrospective data collection. PCT and CRP were measured from the same sample in all patients, and in some cases sampling was performed multiple times. PCT and CRP values were measured by enzyme-linked fluorescent assay using the VIDAS system (bioMerieux Co., Lyon, France) and by nephelometry with the IMMAGE system (Beckman Coulter Co., Fullerton, CA, USA), respectively. Clinical and laboratory data were obtained from computerized databases.
PCT values were divided into five categories according to clinical status as follows: Group 1, normal state (PCT values < 0.05 ng/ml); Group 2, local infection (PCT value of 0.05-0.49 ng/ml); Group 3, sepsis (PCT value of 0.5-1.99 ng/ml); Group 4,severe sepsis (PCT value of 2-9.99 ng/ml); and Group 5, septic shock (PCT value > 10 ng/ml). Blood cultures were carried out for 1,010 of the 2,697 samples using the Cobas e601 system (Roche Diagnostics, Mannheim, Germany), which has a detectable range of 0.02-100 ng/ml, sensitivity of 0.06 ng/ml, and specificity of < 0.02 ng/ml.
Samples were further divided into positive and negative blood culture groups. For the former, Bacillus spp., Corynebacterium spp., Propionibacterium spp., or coagulase-negative staphylococci identified in a single culture flask were treated as contaminants; however, if present in at least two culture flasks they were treated as possible pathogens, as were all other detected species. Samples with contaminants were excluded and only the results pertaining to pathogenic bacteria were analyzed in this study.
Values are expressed as mean ± standard deviation (SD), median and interquartile range, or number and percentage. Results of the five PCT categories were compared and the mean ± SD of CRP was compared among the five categories. PCT and CRP values were also compared with respect to positive/negative blood culture groups. The area under the curve (AUC) of PCT and CRP receiver operating characteristic (ROC) curves forpredicting sepsis (thresholds: PCT > 0.5 ng/ml and CRP > 8 mg/dl) were calculated. Sensitivity, specificity, and positive/negative predictive values were also determined to assess the clinical significance of PCT test results and to evaluate threshold values for predicting sepsis based onblood culture results. AUC values were compared using a previously described method [9]. CRP values of the five PCT groups were compared byanalysis of variance. The Student's t test was used to compare mean PCT and CRP values based on blood culture results. Differences with a P value < 0.05 was considered statistically significant. Statistical analyses were performed using MedCalc 13.1.1.0 (Mariakerke, Belgium) and SPSS 20.0 for Windows (SPSS Inc., Chicago, IL, USA).
The distribution of the sampled population according to PCT categories is shown in Table 1. CRP values increased from Group 1 through 5 as a function of PCT level and the differences between groups were statistically significant (P < 0.05 Fig. 1). Mean CRP concentrations in the five PCT categories were 0.13 ± 2.88, 4.93 ± 6.27, 13.85 ± 8.03, 12.70 ± 10.18, and 18.70 ± 10.61mg/dl, respectively (P < 0.01).
Blood cultures were established for 1010 samples 118 were positive whereas the remaining 892 were negative. Median PCT values were 2.55 and 0.35 ng/ml (Fig. 2) andmedian CRP values were 7.41 and 7.49 mg/dl (Fig. 3) in the positive and negative blood culture groups, respectively. Thus, both CRP and PCT levels were higher in the positive than in the negative blood culture group; however, the difference was only statistically significant for PCT (P < 0.01) and not for CRP (P = 0.07).An analysis of ROC curves to assess the predictive value of PCT and CRP for sepsis found that the AUC of PCT was higher than that of CRP (P < 0.01 Fig. 4).
The results of this study demonstrate that CRP value increased proportionately with increases in PCT level in hospitalized patients. In Group 5, which hadthe highest PCT levels, CRP levels were higher than those in Group 1, which hadthe lowest PCT levels. Furthermore, both PCT and CRP values were higher in the positive than in the negative blood culture group. Previous studies have compared biomarkers in patient groups categorized according to PCT level [1011]. Our measurements could therefore be useful for predicting clinically relevant sepsis in hospitalized patients. In this regard, PCT was found to be a more accurate marker than CRP to predict postoperative sepsis.
The early identification of hospitalized patients who may develop sepsis can enable more timely intervention. Decision-making based on symptoms of infection is often subjective, as these may be attenuated or nonspecific. As such, detecting an infection or sepsis in hospitalized patients remains a challenge, and there is a need for reliable biomarkers for this purpose however, currently available clinical and biological parameters such as leukocyte count and CRP cannot always distinguish between sepsis and SIRS. Furthermore, routine laboratory tests lack sensitivity and specificity, and confirmatory results of microbiological studies are not immediately available.
Biomarkers such as PCT, CRP, and erythrocyte sedimentation rate are known indicators of bacterial infection [12]. In our study, CRP and PCT levels were higher in the positive than in the negative blood culture group. These results underscore the importance of combining biochemical information from biomarkers and clinical statusfor diagnosing sepsis. Moreover, the observed increases in PCT and CRP levels imply that these biomarkers are clinically useful for predicting sepsis, although their levels were also elevated in some patients in the negative blood culture group these may be non-microbiologically confirmed cases, which represent about one third of all sepsis patients [13].
PCT is one of the most accurate biomarkers for diagnosing sepsis and infection [6]. In the present study, we found that a serum PCT concentration > 10 ng/ml was highly suggestive of sepsis with good sensitivity (75.0%), specificity (56.5%), and predictive value. This is consistent with previous studies demonstrating the usefulness of PCT as a marker for infection for instance, high serum PCT was detected in patients with severe bacterial infection, whereas in those without sepsis serum PCT was undetectable [6].
CRP levels have been widely used to diagnose and track infections. Aserum CRP level > 50 mg/l in intensive care unit patients was found to be highly suggestive of sepsis, with a sensitivity of 98.5% and a specificity of 75% [14], although it did not predict disease outcome or severity. CRP is also inadequate for immediate diagnosis and prognosis because of the time taken for a reaction to occur and the limited duration of increased serum levels [91516]. In our study, CRP sensitivity was 47.3% and specificity was 53.1% moreover, the AUC of PCT was higher than that of CRP (0.701, 0.511), suggesting that PCT is superior to CRP as a marker for identifying and diagnosing sepsis. However, it is still unclear whether PCT is more specific than cytokines for infection; although this point remains controversial [17], several studies have provided evidence for the usefulness of PCT as a predictive biomarker in clinical settings [513].
Our study had some limitations. Firstly, given that it was a retrospective and single-center study there may have been observational and selection biases for example, the heterogeneous nature of patient blood samples may have obscured greater differences in the results. Secondly, the influence of disease time course must be taken into consideration, since some studies have shown that the PCT level increases at an earlier time point than that of CRP after sepsis onset and also decreases sooner during the course of controlled sepsis [1819]. Therefore, follow-up studies may be needed for patients with clinically suspected sepsis.
In conclusion, PCT is a reliable and specific sepsis biomarker in critically ill patients, and may be a useful predictive tool. Accurate determination of PCT levels in a clinical setting can improve the treatment of hospitalized patients by enabling a timely diagnosis and avoiding potentially unnecessary treatment.
Figures and Tables
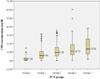 | Fig. 1Comparison of C-reactive protein levels in accordance with the five categorized groups of patients based on procalcitonin levels as follows: Group 1: 10 ng/mL. The box plot shows the lower quartile, mean, and upper quartile value. |
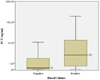 | Fig. 2Procalcitonin levels in the blood culture-positive group and blood culture negative-group. The boxes show the lower quartile, median, and upper quartile values. |
 | Fig. 3C-reactive protein levels between the blood culture-positive group and blood culturenegative group. The boxes show the lower quartile, median, and upper quartile values. |
References
1. Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (sirs). A prospective study. JAMA. 1995; 273:117–123.

2. Biffl WL, Moore EE, Moore FA, Peterson VM. Interleukin-6 in the injured patient. Marker of injury or mediator of inflammation. Ann Surg. 1996; 224:647–664.
3. Mokart D, Capo C, Blache JL, Delpero JR, Houvenaeghel G, Martin C, et al. Early postoperative compensatory anti-inflammatory response syndrome is associated with septic complications after major surgical trauma in patients with cancer. Br J Surg. 2002; 89:1450–1456.

4. Ghillani PP, Motte P, Troalen F, Jullienne A, Gardet P, Le Chevalier T, et al. Identification and measurement of calcitonin precursors in serum of patients with malignant diseases. Cancer Res. 1989; 49:6845–6851.
5. Maruna P, Nedelnikova K, Gurlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000; 49:Suppl 1. S57–S61.
6. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518.

7. Karzai W, Oberhoffer M, Meier-Hellmann A, Reinhart K. Procalcitonin--a new indicator of the systemic response to severe infections. Infection. 1997; 25:329–334.

8. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994; 79:1605–1608.

9. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–843.

10. Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, et al. Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001; 164:396–402.

11. Muller B, Becker KL, Schachinger H, Rickenbacher PR, Huber PR, Zimmerli W, et al. Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med. 2000; 28:977–983.

12. Chalupa P, Beran O, Herwald H, Kasprikova N, Holub M. Evaluation of potential biomarkers for the discrimination of bacterial and viral infections. Infection. 2011; 39:411–417.

13. Hur M, Moon HW, Yun YM, Kim KH, Kim HS, Lee KM. [comparison of diagnostic utility between procalcitonin and c-reactive protein for the patients with blood culture-positive sepsis]. Korean J Lab Med. 2009; 29:529–535.

14. Povoa P, Almeida E, Moreira P, Fernandes A, Mealha R, Aragao A, et al. C-reactive protein as an indicator of sepsis. Intensive Care Med. 1998; 24:1052–1056.

15. Haupt W, Fritzsche H, Hohenberger W, Zirngibl H. Selective cytokine release induced by serum and separated plasma from septic patients. Eur J Surg. 1996; 162:769–776.
16. Martin C, Boisson C, Haccoun M, Thomachot L, Mege JL. Patterns of cytokine evolution (tumor necrosis factor-alpha and interleukin-6) after septic shock, hemorrhagic shock, and severe trauma. Crit Care Med. 1997; 25:1813–1819.

17. Gattas DJ, Cook DJ. Procalcitonin as a diagnostic test for sepsis: Health technology assessment in the icu. J Crit Care. 2003; 18:52–58.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download