1. Subjects
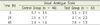
This study was approved by the Institutional Review Board of the hospital in which this research took place. Informed consent was obtained from all of the study participants. Patients aged 18-74 years who had previously undergone orthognathic surgery, discectomy, or total hip arthroplasty, who were classified as American Society of Anesthesiologists (ASA) I or II in the physical status classification system developed by the ASA, and who wished to control postoperative pain through PCA were included in this study. However, these patients had: a history of hypersensitivity to drugs; a body mass index (BMI) ≤ 20 or ≥ 30; serious kidney, liver, or cardiac diseases; been taking narcotic analgesics or sedatives for a long time; used drugs or alcohol; or respiratory diseases were excluded. The patients were fully informed about analgesia and pain assessment devices to be used before they underwent the operation.
2. Method
All patients were premedicated with glycopyrrolate 0.2 mg, and monitored using an electrocardiogram, pulse oximetry, noninvasive blood pressure, end-tidal carbon dioxide monitoring device, and bispectral index (BIS). For anesthetic induction, propofol 2 mg/kg and rocuronium bromide 0.6 mg/kg were administered, and intubation was performed. Anesthesia was maintained at BIS ≥ 40 and ≤ 60, and within 20% of the normal blood pressure and pulse using nitrous oxide along with sevoflurane 0.7~1.3 volume% and remifentanil. Then, palonosetron 0.075 mg was administered to prevent postoperative nausea and vomiting. After the operation was completed, all drug administration was stopped, and pyridostigmine 0.2 mg/kg and glycopyrrolate 0.4 mg were administered to reverse muscle relaxation. Extubation was performed after patients opened their eyes and were able to take a deep breath. The patients were moved to the postanesthetic care unit (PACU). Once the patients regained consciousness and began feeling postoperative pain, they were divided into two groups, and their PCA devices were installed.
The patients were randomly assigned into either the control group or the test group. A PCA infuser (Accumate, Wooyoung Medical Corp., Seoul, Korea), which infuses at a fixed rate, was used for the control group, and a PCA infuser (PS-1000, Unimedics Medical Corp., Seoul, Korea), which makes time-scheduled background infusion, was used for the test group. Postoperative pain was controlled using PCA for 48 hours after the operation. Morphine 1 mg/ml was used. In the control group, the background infusion rate was set to 0.5 ml/h for 48 hours. The amount of PCA bolus was set to 1.0 ml and the filling time was set to 15 min so that the patients could self-administer the drug in times of need. In the test group, the background infusion rate was set at 1 ml/h at 0-24 hours after the operation and 0.5 ml/h at 24-48 hours after the operation. The amount of PCA bolus was 1.0 ml and the filling time was 15 min, similar to the control group.
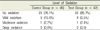
The level of pain was measured on the basis of patients' scores on the visual analogue scale (VAS), which range from 0-10, in the recovery room. PCA devices were connected to the veins of patients who scored 4 or more on the VAS. Patients whose VAS scores were 4 or more even after performing PCA were administered ketorolac 30 mg as a rescue analgesic, and this infusion was recorded.
After the patients were moved to their wards, their VAS scores at 6 h, 24 h, and 48 h after the operation, the number of rescue analgesic injections, side effects (nausea, vomiting, itching, sedation, dyspnea), and satisfaction with analgesia on a scale of five (5 = excellent, 4 = good, 3 = adequate, 2 = poor, 1 = awful) were recorded.
The sample size was calculated with α = 0.05 and β = 0.2 by comparing patient satisfaction and assuming that a mean difference of two or more was clinically meaningful. The calculated sample size was 50 patients in each group. Therefore, this study was conducted with a total of 100 patients.
Statistical analyses were performed with Statistical Package for Social Sciences 17.0 for Windows (SPSS Inc., Chicago, IL, USA). All data were expressed as mean ± standard deviation. A Student's T-test was used to compare the demographic data (not including gender) and doses of morphine infused between the test and the control groups. A Mann-Whitney U-test was performed to compare VAS scores, and a Pearson's Chi-square test or Fisher's exact test was performed to compare the rate of side effects and patient satisfaction. The level of statistical significance was set at P < 0.05.







 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download