Abstract
Lidocaine, a local anesthetic commonly used in dental treatments, is capable of causing allergies or adverse effects similar to allergic reactions. However, the frequency of such occurrences in actual clinical settings is very rare, and even clinical tests on patients with known allergies to local anesthetics may often show negative results. When adverse effects, such as allergy to lidocaine, are involved, patients can be treated by testing other local anesthetics and choosing a local anesthetic without any adverse effects, or by performing dental treatment under general anesthesia in cases in which no local anesthetic without adverse effects is available. Along with a literature review, the authors of the present study report on two cases of patients who tested positive on allergy skin tests for lidocaine and bupivacaine and subsequently underwent successful dental treatments with either general anesthesia or a different local anesthetic.
Local anesthesia plays an important role in dentistry. For example, extraction of the mandibular third molar is impossible without inferior alveolar nerve block, while local infiltration or intrapulpal anesthesia is mandatory during root canal treatments to reduce pain and allow continuation of the treatment. As these examples demonstrate, local anesthesia is an indispensable part of dentistry, and yet, lidocaine, a local anesthetic commonly used in dentistry, can cause allergies or other adverse effects [12]. Allergic reactions may include mild symptoms, such as urticaria, erythema, and intense itching, as well as severe reactions in the form of angioedema and/or respiratory distress. Even more severe life-threatening anaphylactic responses include symptoms of apnea, hypotension, and loss of consciousness [23].
Allergic reactions to local anesthetics are known to involve two types of reactions: immunoglobulin E (IgE)-mediated type I and T-cell-mediated type IV reactions. Meanwhile, delayed type IV reactions are caused mostly by topical anesthetics and are characterized by localized edema. The incidence of adverse effects from local anesthetics is generally reported as 0.1–1% [4], and actual known cases of allergic reactions among these cases of adverse effects account for less than 1%, indicating that allergic reactions are extremely rare [1]. Ester-type local anesthetics tend to be relatively more allergenic. Consequently, amide-type anesthetics are widely used, among which lidocaine is the most common and is used for dental anesthesia in a form that contains epinephrine. Epinephrine is a vasoconstrictor that is usually added to extend the duration of local anesthetics. Because it can cause symptoms of pallor, tachycardia, anxiety, headache, tremor, and hypertension [4], such symptoms must be distinguished from allergic reactions caused by the local anesthetic itself.
The objective of the present case report was to examine two cases of positive skin allergy tests performed as a result of the occurrence of adverse effects associated with the use of lidocaine as local anesthesia, and to report on dental treatments under such circumstances, along with a literature review.
A 54-year-old female patient, weighing 77 kg, experienced various symptoms such as clouding of consciousness, hearing impairment, and chills during dental treatment for periodontal disease using a local anesthetic. Under the assumption that these adverse effects were attributable to the use of lidocaine, the patient was transferred to the Department of Allergy to determine whether local anesthesia with bupivacaine would be possible.
The Department of Allergy performed skin prick and intradermal tests to test for reactivity to bupivacaine, and the patient tested negative in the skin prick test. In the skin provocation test, when administered an intradermal injection of 0.1 cc bupivacaine diluted to 1:100, the patient complained of listlessness and drowsiness beginning 30 s after the injection. Following an intradermal injection of 0.1 cc bupivacaine diluted to 1:10, the patient's symptoms of listlessness and drowsiness became more severe from 30 s after the injection. When administered an intradermal injection of 0.1 cc of undiluted bupivacaine, the patient was placed in a recumbent position on a bed owing to complaints of listlessness and heavy eyes at approximately 50 s after the injection. Subsequently, the patient showed symptoms of shivering, which eventually became uncontrollable, and she had difficulty keeping her eyes open. As a result, the patient was given 2 doses of 0.5 mg Ativan. Afterward, the patient appeared to be more stable, but began showing symptoms of shaking her chin and one of her arms, for which 0.5 ampule of Demerol™ was administered, after which her condition began to improve. The testing was completed within 20 min and the patient was discharged after a 5 h observation period. The patient was diagnosed with bupivacaine intolerance, meaning the appearance of adverse effects even with small amounts of the medication, and the dental treatment was subsequently performed under general anesthesia since local anesthesia was determined to be impossible.
A 41-year-old female patient received an injection of lidocaine containing epinephrine for root canal treatment, and then, about 30 min later, symptoms of dizziness and systemic urticaria appeared. The patient was determined to be hypersensitive to lidocaine and transferred to the department of allergy.
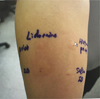
Skin prick testing was performed using lidocaine, procaine, bupivacaine, mepivacaine, chirocaine (levobupivacaine), ropivacaine, and articaine, and the patient tested positive to lidocaine, ropivacaine, and articaine (Fig. 1). Among the drugs to which she had tested negative, lidocaine, procaine, mepivacaine, and bupivacaine were used for a skin test, in which a positive reaction was seen only with lidocaine.
Restorative treatment was performed using procaine, to which the patient had tested negative in the skin test, but it was ineffective as a result of its shorter duration of activity than lidocaine, resulting in the appearance of adverse effects, such as increased anxiety in the patient. Subsequent treatments were performed using levobupivacaine, with which satisfactory treatment effects, in terms of pain reduction and duration, were achieved.
Lidocaine and other local anesthetics, drugs commonly used in dentistry, may cause various adverse effects, although these are low in frequency [5]. Such adverse effects include immune response-mediated allergic reactions and others that are unrelated to the immune response [1]. In actuality, immune response-mediated allergic reactions are extremely rare, and adverse effects that are not allergic reactions may include toxic reactions and autonomic responses [467].
First of all, allergic reaction to local anesthetic is very rare, with a rate of occurrence of less than 1% [1]. Allergic reaction to local anesthetic involves two major types: IgE-mediated type I and T-cell-mediated type IV reactions [8910]. Type I reaction occurs as a result of the release of mediators, such as histamine from mast cells and basophils, which leads to the binding of IgE antibodies to antigens [6]. The typical type I reaction appears immediately, within a few sec to a few min, but it may take 1–4 h for symptoms to appear. Type IV reaction is mediated by T cells that are exposed to the antigens expressed by the Langerhans cells, and the reaction occurs when the sensitized memory T cells are exposed again to the same antigens [6]. This typically takes 24–72 h to appear, but may appear within 2 h in some cases. In fact, the clinical differentiation of type I and type IV reaction can be viewed as impossible.
Anesthetics for local anesthesia are structurally connected by lipophilic aromatic rings and hydrophilic amine groups, with intermediary groups as the mediator [9]. Local anesthetics can be classified according to such intermediary groups–ester, amide, ketone, and others [7]. Type I and IV reactions occur mostly in association with ester-type anesthetics. This is because para-aminobenzoic acid (PABA), a metabolite of the ester group, possesses strong allergenic potential [8]. Methyl-paraben and propylparaben, widely used as preservatives of local anesthetics, can also induce allergic reactions as a result of their metabolism, which produces compounds similar to PABA [38].
One of the adverse effects of local anesthetics, other than allergic reaction, is toxic reaction, which can appear following intravascular injection of local anesthetic, manifesting as cardiovascular and central nervous system toxicity [6]. Symptoms of toxic reaction include convulsions, hypotension, and bradycardia, and in some cases, it may lead to cardiovascular collapse, coma, and even death.
Among the adverse effects of local anesthetics, autonomic responses include sweating, dizziness, nausea, and mild tachycardia [6]. These symptoms may appear as a result of the dental treatment itself or due to fear and nervousness regarding injections, while in rare cases, they may be attributed to vasoconstrictors contained in the local anesthetic.
Moreover, there may be adverse effects from sulfite antioxidant, which is added to local anesthetic as an antioxidant. Asthma-like symptoms, such as tachycardia, wheezing, bronchospasm, dyspnea, tachypnea, dizziness, and weakness have been reported. Severe flushing, generalized urticaria, angioedema, tingling, pruritis, rhinitis, conjunctivitis, dysphagia, nausea, and diarrhea may also appear [2].
The skin prick test is the most universally accepted method for diagnosing allergies [6]. When skin prick test results are determined to be negative, intradermal testing is performed. Intradermal tests are performed by beginning with the lowest concentration of the potential allergen and gradually increasing its concentration. Meanwhile, drug provocation testing is performed only in cases in which the patient has an existing history of allergies.
For patients who have a history of allergy to local anesthetics, careful and thorough history taking regarding the history of allergies is important, and allergy tests, such as skin prick and/or intradermal tests become mandatory [8]. In subsequent treatments, local anesthetics to which the patient had tested negative in the allergy tests should be used, and when such an option is unavailable, treatment under general anesthesia should be considered.
In the first case reported above, dental treatment was performed on the patient under general anesthesia since she showed adverse effects to lidocaine and also showed adverse effects when bupivacaine was used, based on which it was determined that the use of local anesthetic might be dangerous. The general anesthesia or sedation may be a useful alternative to avoid the critical allergic reaction of local anesthetics. In the second case, the patient was found to be allergic to lidocaine, and thus, another drug to which the patient did not have a positive allergy test was used in performing dental treatments.
Although rare, adverse effects from local anesthetic may be encountered at any time in clinical settings. In these cases, it is important to determine whether the patients actually have allergies, and if a local anesthetic that does not cause adverse effects can be identified, then that drug should be used for local anesthesia in performing dental treatments. However, if no such drug is available, then the use of general anesthesia might be unavoidable.
References
1. Batinac T, Sotosek Tokmadzic V, Peharda V, Brajac I. Adverse reactions and alleged allergy to local anesthetics: Analysis of 331 patients. J Dermatol. 2013; 40:522–527.

2. Finder RL, Moore PA. Adverse drug reactions to local anesthesia. Dent Clin North Am. 2002; 46:747–757.

3. Speca SJ, Boynes SG, Cuddy MA. Allergic reactions to local anesthetic formulations. Dent Clin North Am. 2010; 54:655–664.

4. Fisher MM, Bowey CJ. Alleged allergy to local anaesthetics. Anaesth Intensive Care. 1997; 25:611–614.

5. Ping B, Kiattavorncharoen S, Durward C, Im P, Saengsirinavin C, Wongsirichat N. Hemodynamic changes associated with a novel concentration of lidocaine hcl for impacted lower third molar surgery. J Dent Anesth Pain Med. 2015; 15:121–128.

6. Noormalin A, Shahnaz M, Rosmilah M, Mujahid SH, Gendeh BS. Ige-mediated hypersensitivity reaction to lignocaine - a case report. Trop Biomed. 2005; 22:179–183.
7. González-Delgado P, Anton R, Soriano V, Zapater P, Niveiro E. Cross-reactivity among amide-type local anesthetics in a case of allergy to mepivacaine. J Investig Allergol Clin Immunol. 2006; 16:311–313.
8. Grzanka A, Wasilewska I, Sliwczynska M, Misiolek H. Hypersensitivity lo local anesthetics. Anaesthesiol Intensive Ther. 2016; 48:128–134.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download