Abstract
Background
Failure to maintain a patent airway can result in brain damage or death. In patients with mandibular prognathism or retrognathism, intubation is generally thought to be difficult. We determined the degree of difficulty of airway management in patients with mandibular deformity using anatomic criteria to define and grade difficulty of endotracheal intubation with direct laryngoscopy.
Methods
Measurements were performed on 133 patients with prognathism and 33 with retrognathism scheduled for corrective esthetic surgery. A case study was performed on 89 patients with a normal mandible as the control group. In all patients, mouth opening distance (MOD), mandibular depth (MD), mandibular length (ML), mouth opening angle (MOA), neck extension angle (EXT), neck flexion angle (FLX), thyromental distance (TMD), inter-notch distance (IND), thyromental area (TMA), Mallampati grade, and Cormack and Lehane grade were measured.
Results
Cormack and Lehane grade I was observed in 84.2%, grade II in 15.0%, and grade III in 0.8% of mandibular prognathism cases; among retrognathism cases, 45.4% were grade I, 27.3% grade II, and 27.3% grade III; among controls, 65.2% were grade I, 26.9% were grade II, and 7.9% were grade III. MOD, MOA, ML, TMD, and TMA were greater in the prognathism group than in the control and retrognathism groups (P < 0.05). The measurements of ML were shorter in retrognathism than in the control and prognathism groups (P < 0.05).
The failure of airway maintenance is the most common cause of anesthetic-related mortality in dental anesthesiology [1]. Orthognathic surgery involves the correction of musculoskeletal, dento-osseous, and soft tissue deformities of the jaws and surrounding structures. Patients who request orthognathic surgery may have severe anatomical anomalies of airway anatomy such as mandibular prognathism or retrognathism. Safe and secure airway management by the anesthesiologist is essential, and preoperative airway evaluation is critical in those patients [2]. Mandibular prognathism in acromegalic patients is recognized as one cause of difficulty in airway management and tracheal intubation [3]. However, there are few data regarding the incidence of difficult intubation in mandibular anomaly patients who request orthognathic surgery.
Preoperative screening to identify patients in whom tracheal intubation may be difficult or impossible may reduce mortality and morbidity [4]. Predictors of difficult intubation such as the modified Mallampati classification, measurement of the thyromental distance, and head and neck movement, have been used to predict a difficult airway with some acceptable accuracy [5678].
We hypothesized that these airway evaluation parameters would aid in identifying difficult airway cases in patients with mandibular deformities. The purpose of this study was to enable prediction of the Cormack and Lehane laryngeal grade in dentofacial patients who may have abnormal airway evaluation parameters because of anomalous mandibular anatomy.
This prospective, single-blinded study was performed at Seoul National University Dental Hospital after approval from the hospital institutional review board (L0605-09). Written informed consent was obtained from 255 patients aged > 18 years scheduled for elective surgical procedures to treat malocclusion or oral problems requiring endotracheal intubation. Patients were excluded if they had a documented history of difficult intubation, a potentially difficult airway suggested by physical examination, obstructive sleep apnea, recurrent epistaxis, bleeding diathesis, a history of taking anticoagulant drugs, or risks for aspiration.
To divide patients into 3 groups, i.e., prognathism, normal, or retrognathism, lateral cephalometric radiographs were used. The ANB angle made by the sella (S), nasion (N) and A point of the maxilla, and B point of the mandible was used by an orthodontist (Fig. 1) Classification of patient groups was defined by orthodontists; ANB angle below -1 (prognathism group), above 4 (retrognathism group), and between -1 and 4 (normal group). Of 255 patients, 133 had mandibular prognathism, 33 had mandibular retrognathism, and 89 had a normal mandible relationship (Table 1).
Preoperative evaluation was performed in all patients using the following protocol. A modified Mallampati classification [9], mouth opening distance (MOD), mandibular depth (MD), mandibular length (ML), mouth opening angle (MOA), neck extension angle (EXT), neck flexion angle (FLX), thyromental distance (TMD), internotch distance (IND), and thyromental area (TMA) were determined before general anesthesia (Fig. 2) [10].
Pre-anesthetic medication was not administered. Routine monitoring was performed with an electrocardiogram, pulse oximetry, capnograph, and a noninvasive blood pressure cuff. Patients were placed in the supine position with the head on an approximately 8 cm-high pillow. After anesthesia induction using propofol 1.5 mg/kg intravenous (IV) following lidocaine 30 mg IV, and neuromuscular blockade with vecuronium 0.1 mg/kg IV, patients were ventilated with 7-8 vol% sevoflurane in 100% O2 via a facial mask. We monitored the train-of-four ratio, and intubation was performed at 0/4. A #3 Macintosh blade was used for women and #4 for men. Cormack and Lehane laryngeal view grades were measured during laryngoscopy [11].
Demographic data are reported as mean values with standard deviation (SD) and range. The Kruskal-Wallis test was used to compare the level of laryngeal view, and multiple comparisons among groups were analyzed using the Wilcoxon rank-sum test and Bonferroni correction. For comparison of criteria for airway evaluation in the 3 groups, analysis of variance (ANOVA) was used; multiple comparisons among groups were analyzed by the SNK test. SPSS software (version 22.0; SPSS Inc., Chicago, IL, USA) was used. A P-value < 0.05 was regarded as significant.
There were no significant differences in age, gender, height, and weight among the 3 groups. The ANB values were -5.4 ± 3.4 for prognathism, 1.2 ± 1.1 for normal, and 5.7 ± 1.7 for retrognathism groups. The Mallampati grades, which were assessed while the patients opened their mouths before anesthesia, were grade I in 84.2%, grade II in 15%, grade III in 0.8%, and grade IV in 1.5% for prognathism; grade I in 46.1%, grade II in 41.6%, grade III in 10.1%, and grade IV in 2.2% for controls; and grade I in 33.3%, grade II in 36.4%, grade III in 24.2%, and grade IV in 6.1% for retrognathism; the grades were significantly different between the groups (Table 2). The measurements of MOD, MOA, ML, TMD, and TMA were greater in prognathism than in the control and retrognathism groups (P < 0.05). The measurements of ML were shorter in retrognathism than in the control and prognathism groups (P < 0.05) (Table 3).
Laryngeal grades based on laryngoscopic views were as follows. Cormack and Lehane grade I was observed in 84.2%, grade II in 15.0%, and grade III in 0.8% of the mandibular prognathism cases; grade I in 45.4%, grade II in 27.3%, and grade III in 27.3% of the retrognathism cases; and grade I in 65.2%, grade II in 26.9%, and grade III in 7.9% of the control group (Table 4).
Failure of airway maintenance during general anesthesia increases the risk of serious complications such as brain damage and death; therefore, proper airway maintenance is critical [11213]. Deformities of various anatomical structures related to airway are more common in oral and maxillofacial patients than in normal individuals, and airway maintenance is difficult for these patients in most cases [14]. Despite its importance, few systematic studies have attempted to predict which patients would have difficulty with airway maintenance before anesthesia. Although there are a number of evaluation parameters, such as mouth opening distance, Mallampati grade, and Cormack and Lehane grade, they are not easily applicable to prognathism and retrognathism patients [34581516171819].
Prognathism and retrognathism are conditions in which the maxilla protrudes more than the mandible, or vice versa. Airway maintenance using a mask is difficult in patients with these conditions, and airway evaluation parameters may be different from those of normal individuals. Evaluation parameters inadequately predict a difficult airway in prognathism and retrognathism patients, and previous studies have mostly focused on changes in airway anatomy after corrective jaw surgery [20212223]. The aim of this study was to identify factors that affect the difficulty of tracheal intubation by evaluating various airway parameters that have been commonly used, or have not been used before. Retrognathism patients, in whom tracheal intubation is known to be difficult [24], prognathism patients, in whom tracheal intubation is relatively easy [10], and a control group with normal patients were compared.
In this study, Mallampati grades III and IV were more common in the retrognathism group than in the prognathism and control groups (Table 2). The prognathism group had greater MOD, ML, TMD, MOA, and TMA measurements, compared to the retrognathism and normal groups. The ML in the retrognathism group was statistically significantly shorter than in the normal and prognathism groups (Table 3). Cormack and Lehane grade 1 was more common in the prognathism group than in the normal group, and grade III was common in the retrognathism group; both values were statistically significant (Table 4).
The results of airway evaluation in this study showed that prognathism patients had normal airways, predicting easy tracheal intubation using a laryngoscope in these patients. When they were actually observed through a laryngoscope, most airways were Cormack and Lehane grade I and II and tracheal intubation was relatively easy, as had been predicted during airway evaluation before anesthesia. However, in some prognathism patients with relatively developed mandibles, airway maintenance using a mask after anesthetic administration was difficult. A relatively large number of retrognathism patients had Mallampati grades III and IV, and a short ML, leading to a prediction that intubation might be difficult in these patients. When their vocal cords were observed under a laryngoscope, there were more Cormack and Lehane grade III patients, compared with the normal and prognathism patients, and intubation was relatively difficult in grade III patients.
In this study, we predicted difficult intubation in retrognathism patients through physical examination, and confirmed this prediction. Our finding that Mallampati grade and ML can be used to predict difficult intubation in retrognathism patients is meaningful; by taking preparative measures based on this prediction, one may prevent dangerous situations such as failure of airway maintenance. Anatomical structures related to the mandible were used as airway evaluation parameters in this study to predict the difficulty of tracheal intubation. These parameters should be helpful in predicting the difficulty of tracheal intubation not only in prognathism and retrognathism patients, but also in other patients who require intubation for common general anesthetic procedures.
Small sample size is one of the limitations of this study. While a larger overall sample size would have provided better results, the especially small sample size of the retrognathism group with only 33 patients was a major limiting factor. However, because there were few cases of retrognathism, a prolonged period would have been required to obtain a larger sample size for this group. Another limitation was the relationship between ML and the Cormack and Lehane grade. Although Cormack and Lehane grade III was significantly more common in retrognathism patients with shorter ML in our study, more research on this relationship is needed.
In conclusion, intubation by laryngoscopy is easier in prognathism patients than in patients with normal mandibles. However, patients with retrognathism of the mandible have poor Cormack and Lehane grades, making intubation by laryngoscopy difficult, possibly because of the ML in such cases.
Figures and Tables
Fig. 1
To divide patients into 3 groups, i.e., prognathism, normal, and retrognathism, lateral cephalometric radiographs were used. Orthodontists decided which patients had an ANB angle below -1 in the prognathism group, above 4 in the retrognathism group, and between -1 and 4 in the normal group (Table 1).
1. Prognathism, 2. Normal, 3. Retrognathism.
A (A point or subspinale): deepest point on maxillary alveolus, B (B point or supramentale): deepest point on mandibular alveolus.

Fig. 2
In all patients, mouth opening distance (MOD), mandibular depth (MD), mandibular length (ML), mouth opening angle (MOA), neck extension angle (EXT), neck flexion angle (FLX), thyromental distance (TMD), inter-notch distance (IND), thyromental area (TMA).

Table 1
Demographic characteristics
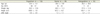
Table 2
Mallampati grade

Table 3
Criteria for airway evaluation

References
1. Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990; 72:828–833.

2. Krohner RG. Anesthetic considerations and techniques for oral and maxillofacial surgery. Int Anesthesiol Clin. 2003; 41:67–89.

3. Schmitt H, Buchfelder M, Radespeil-Troger M, Fahlbusch R. Difficult intubaton in acromegalic patients. Incidence and predictability. Anesthesiology. 2000; 93:110–114.

4. Voyagis GS, Kyriakis KP, Dimitriou V, Vrettou I. Value of oropharyngeal mallampati classification in predicting difficult. Eur J Anaesthesiol. 1998; 15:330–334.

5. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Liu PL, et al. A clinical sign to predict difficult tracheal intubation: A prospective. Can Anaesth Soc J. 1985; 32:429–434.
6. Frerk CM. Predicting difficult intubation. Anaesthesia. 1991; 46:1005–1008.
7. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988; 61:211–216.

8. Lee A, Fan LTY, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the mallampati. Anesth Analg. 2006; 102:1867–1878.

9. Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987; 42:487–490.

10. Lee SJ, Kim HJ, Yum KW. Airway evaluation for endotracheal intubation of mandibular prognathic patient. J Korean Dent Soc Anesthesiol. 2003; 3:28–33.

11. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984; 39:1105–1111.

12. Julien F, Biebuyck MB, Phil D. Management of the difficult adult airway. Anaesthesiology. 1991; 75:1087–1110.

13. Tiret L, Desmonts JM, Hatton F, Vourc'h G. Complications associated with anaesthesia--a prospective survey in france. Can Anaesth Soc J. 1986; 33:336–344.

14. Bavitz JB, Collicott PE. Bilateral mandibular subcondylar fractures contributing to airway obstruction. Int J Oral Maxillofac Surg. 1995; 24:273–275.

15. Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Perdicting difficult intubation. Br J Anaesth. 1988; 61:211–216.
16. Oates JDL, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. Br J Anaesth. 1991; 66:305–309.
17. Tham EJ, Gildersleve CD, Sanders LD, Mapleson WW, Vaughan RS. Effects of posture, phonation and observer on mallampati classification. Br J Anaesth. 1992; 68:32–38.
18. Savva D. Prediction of difficult tracheal intubation. Br J Anaesth. 1994; 73:149–153.
19. Ochroch EA, Hollander JE, Kush S, Shofer FS, Levitan RM. Assessment of laryngeal view: Percentage of glottic opening score vs cormack and lehane grading. Can J Anaesth. 1999; 46:987–990.

20. Katakura N, Umino M, Kubota Y. Morphologic airway changes after mandibular setback osteotomy for prognathism with and without cleft palate. Anesth Pain Control Dent. 1993; 2:22–26.

21. Enacar A, Aksoy AU, Sencift Y, Haydar B, Aras K. Changes in hypopharyngeal airway space and in tongue and hyoid bone positions following the surgical correction of mandibular prognathism. Int J Adult Orthodon Orthognath Surg. 1994; 9:285–290.

22. Kawamata A, Fujishita M, Ariji Y, Ariji E. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular setback osteotomy for prognathism. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000; 89:278–287.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download