Abstract
Dentists often sedate patients in order to reduce their dental phobia and stress during dental treatment. Sedatives are administered through various routes such as oral, inhalation, and intravenous routes. Intravenous administration has the advantage of rapid onset of action, predictable duration of action, and easy titration. Typically, midazolam, propofol or dexmedetomidine are used as intravenous sedatives. Administration of these sedatives via infusion by using a syringe pump is more effective and successful than infusing them as a bolus. However, during intravenous infusion of sedatives or opioids using a syringe pump, fatal accidents may occur due to the clinician's carelessness. To prevent such risks, smart syringe pumps have been introduced clinically. They allow clinicians to perform effective sedation by using a computer to control the dose of the drug being infused. To ensure patient safety, various alarm features along with a drug library, which provides drug information and prevents excessive infusion by limiting the dose, have been added to smart pumps. In addition, programmed infusion systems and target-controlled infusion systems have also been developed to enable effective administration of sedatives. Patient-controlled infusion, which allows a patient to control his/her level of sedation through self-infusion, has also been developed. Safer and more successful sedation may be achieved by fully utilizing these new features of the smart pump.
A large number of patients experience pain-related fear and anxiety during dental treatment, which prevent patients from receiving proper treatment [1]. As a result, dentists often sedate patients to reduce this stress during dental treatment [2]. During the sedation, sedatives are administered to depress the patient's consciousness to a certain level. Depending on the depth of sedation, suppression of cardiovascular functions, breathing reduction and airway obstruction may occur [3]. Depending on the degree of invasiveness of the dental treatment and the level of the patient's anxiety, the target sedation depth may be modified, and the patient's response to the sedatives may vary. In some cases, patients are not able to reach an appropriate level of sedation, leaving both the patients and dentists feeling dissatisfied with the result [4]. Since sensitivity to sedatives varies depending on the level of anxiety, pain, and stress experienced by the patient, uniform administration of sedatives is impossible in most cases. Therefore, the appropriate dose as well as the type of sedatives should be determined before administration.
Commonly used routes of administration include oral, inhalation, and intravenous routes. Intravenous administration has the advantage of fast onset of action, predictable duration of action, easy titration, and applicability during emergencies (through the secured vein passage). Drugs used in dental sedation include midazolam, propofol, ketamine, dexmedetomidine, alfentanil, and remifentanil. Although dentists intermittently administer these drugs by hand, it is more common to administer them using a syringe pump owing to the pharmacodynamics of these drugs [5].
Proper use of the syringe pump is important. Injecting an excessive amount of the drug, or not realizing that the full amount has been infused due to the absence of an alarm can create complications. Therefore, the concept of computer-controlled smart pumps that safely control the amount of drug administered intravenously was introduced [6]. In addition, smart pumps have an internal drug library that provides dentists with important information regarding drug safety. They also help dentists in determining the right dose of a drug and in controlling the infusion amount to prevent excessive injection. Therefore, smart pumps perform error-free intravenous infusion of high-risk drugs [7].
With the advent of smart pumps, dentists can go beyond continuous infusion, and perform programmed infusion and target-controlled infusion. Recently, patient-controlled infusion, which allows patients to infuse sedatives into themselves to control their level of sedation, has also been introduced. Patient-controlled sedation has been known to require a relatively small amount of drug, and it has a fast recovery rate [8].
A syringe pump used in dental sedation should be sufficiently accurate. The actual amount of drug infused into the patient should not differ from the pre-set target infusion amount during long-term use. Moreover, the pump must be light, easy, and electrically and physically stable to use.
A syringe pump must be designed in a way that does not allow back-flow of the fluid within the syringe or outward flow due to the movement of a siphon. Small syringes (10 ml) used for infusion in pediatric patients, as well as large syringes (50 ml) used in adults should be amenable to be attached to the pump. In addition, since syringes of an identical capacity may still differ in their diameters and lengths depending on their manufacturers, a syringe pump must be able to adapt to different syringe sizes.
The unit of infusion rate is typically ml/h. The syringe pump should be able to perform micro infusion (1 ml/h) as well as fast infusion (over 1,000 ml/h) for patient-controlled sedation. The total infusion amount and rate should be displayed on an LCD screen. Infusion rates expressed as µg/kg/min (patient's body mass is taken into account) are easier to control [9].
A syringe pump should have a proper alarm device associated with drug infusion. The alarm should ring during unstable power supply and upon infusion completion, improper infusion due to and other operational errors [10].
In addition, the pump should be able to operate on batteries in order to keep the saved data in case the main power supply is out. It should also be compatible with computers so that it can be operated through an external computer and the information regarding the infused drug and the action of the pump can be saved within the internal memory of the pump. The saved data can then be exported to the computer. Features such as automatic syringe size recognition and drug databases are also very useful [4].
When infusion pumps were first introduced in the 1970s, they were used for cardiovascular drug infusions in intensive care units (ICUs). Since then, the infusion rate, accuracy, and dose range of these pumps have increased, enabling their use in many areas of treatment. In the field of anesthesia, syringe pumps with higher drug infusion accuracy have been used for infusion of anesthetics and cardiovascular drugs during surgery, as well as for infusion of sedatives during dental treatment.
With the increasing use of infusion pumps, reports of medical accidents due to pump malfunction or carelessness of doctors or nurses have also increased in number. Consequently, the national boards for approval of medical devices compelled the medical device companies to add alarms to their pumps in order to increase their safety. As a result, an alarm within the syringe pump now rings in case of not only pump malfunction, but also infusion needle occlusion, empty container, and even broken connecting tube [9]. Infusion pumps are now being used in circumstances that require precise drug infusion, scheduled infusion, and in patient-controlled infusion.
Despite this protective feature, imprecise general-purpose infusion pump settings have incurred tragic results. According to the Institute of Medicine's (IOM) report, Preventing Medication Errors, on the cases of medical accidents due to errors in drug infusion, 1,500,0000 patients suffered damage from infusion errors every year, and inpatients were prone to at least one medication error (IOM, 2006) [11]. Among the drugs that are administered intravenously, anticoagulants, thrombolytic drug, narcotics, hormones, and sedatives pose a high level of danger, and their use often causes serious medical accidents. When infusion errors of these drugs were evaluated, more than one error was identified in 67% of the drugs [12].
As a result, smart pumps were introduced to increase the safety of drug administration using an infusion pump. They are controlled by a computer with a dose error reduction system (DERS), which stops the infusion when the infused dose crosses the safe level. The advanced features of smart pumps are listed in Table 1 [13].
In traditional infusion pumps, the user determines the infusion method based on the information provided by the clinician and the drug type. Information regarding drug infusion such as the rate of infusion, dose, and infusion time is entered into the infusion pump. During manual input of information into the computer, prescription, dosage, and typing errors may occur, leading to erroneous infusion.
The drug library is a profile or a list of drugs that are listed by medical institutions or medical staff and saved into the infusion pump. It provides administration parameters specific for a certain patient. The drug library software that functions within the pump requires patient information and the drug name to be provided before the pump is used. In addition, it provides information regarding drug dose, and helps determine the right dose of the medication [14].
For instance, once a medication name is chosen, information related to the medication (standard concentration, infusion rate, maximum dose, etc.) is displayed on the LCD screen. When the infusion dose is increased, the pump differentiates the limit of infusion as either soft alerts limit or hard alerts limit through its drug library. A soft alert limit allows the dentist (who performs the infusion) to override the limit and continue the infusion, whereas a hard alert limit does not allow this unless the drug library parameters within the pump are changed and re-written [13].
In clinical settings, these drug library requirements may be ignored; in other words, the step of entering the drug name can be bypassed, and a high dose of drug can be infused into the patient only after setting the infusion rate (ml/hour). However, this method does not consider patient safety. A valuable resource for dentists using smart pumps is the Institute for Safe Medication Practices (ISMP, 2009) online publication "Proceedings from the ISMP Summit on the use of Smart Infusion Pumps: Guidelines for Safe Implementation and Use" available at www.ismp.org/tools/guidelines/smartpumps/printerversion.pdf.
The drug library includes information about drug name, type, standard concentration, continuous infusion concentration, bolus dose, bolus infusion rate, etc. The standard units for dose are g, mg, and µg. They can also be expressed as mg/ml or µg/kg, which takes into account the patient's body mass or drug concentration. The units of infusion rate are mg/kg/h, and µg/kg/min. A standard sample of a drug library is shown in Table 2. Figure 1 shows a program that creates a drug library list. A drug library made from such a program is saved into the syringe pump.
The smart pumps were integrated with computerized software, which can be used to create a profile of infusion time and dose in the form of a program. The software can make use of pharmacokinetic and pharmacodynamic characteristics of a drug to determine the most appropriate drug concentration for the purpose of infusion. For instance, it can make the pump infuse a certain amount of insulin every 12 hours, or stop the infusion after a certain amount of time has passed. During the administration of anesthetics or sedatives, infusion of a high volume loading dose, followed by a low volume continuous dose is necessary. Under such circumstances, the computerized intelligent software creates a profile of infusion stages in which the drug is initially infused rapidly for a certain period of time, and the infusion rate is altered afterwards. Dexmedetomidine is one of the most commonly used sedatives in dental sedation. A dose of 0.25-1 µg/kg of this sedative is infused for 10 minutes, after which the dose is subsequently reduced. This example is shown in Figure 2 [15].
Since its introduction in 1986, propofol has been used as the classic intravenous anesthetic agent. It has a fast onset of action in addition to a short recovery time. It can also be easily administered intravenously without the need for anesthetic equipment and does not contaminate the operation room with its anesthetic gas, as in the case of inhalation-based anesthetics. More importantly, propofol can be administered through target-controlled infusion (TCI) [16].
The basic principle of TCI is to universally set the depth of sedation, i.e. the target blood concentration, and to adjust the dose based on the patient's condition. An individualized infusion rate is calculated by a computer based on a pharmacokinetic model, as the infusion rate automatically reaches a set point by predicting the sedative concentration in the blood [17].
Infusion of propofol through TCI is possible because propofol has a rapid and wide distribution within the body and shows fast clearance. Remifentanil, which also shows fast clearance, can be infused through TCI as well. Initially, infusion was based on a 3-compartmet pharmacokinetic model and focused on the concentration of the drug in the blood. However, reaching the effect site concentration, which reflects drug effects due to distribution throughout the blood and time delay, does not necessarily mean that optimal sedation has been achieved. Consequently, one may adjust the settings of a virtual effect site compartment that can predict the effect site concentration of propofol, and build a 4-compartment model in which the effect site concentration is set as the target concentration, prior to performing propofol infusion (Fig. 3) [18].
From the smart pump perspective, TCI is advantageous in that, 1) it is easy to manipulate, 2) it allows for easy control of sedation depth, 3) it shows an estimated drug concentration in the blood, 4) it has compensatory actions in case infusion is hindered, 5) no time-consuming calculations are necessary, and 6) sedation induction and maintenance can be performed continuously. Moreover, it also decreases the risk of accidents that arise due to confusion among clinicians due to different target concentrations used during sedation.
TCI systems have been developed for propofol, alfentanil, and remifentanil so far. Their target patients are 16-100 years of age, weigh 30-150 kg, and require target concentrations of 0.1-15 µg/ml. Although TCI has been used in anesthesia induction and maintenance in adults, development of TCI systems of a greater diversity such that they can be used in various age groups may be possible in the future.
In patient-controlled sedation, a patient can set the bolus dose and lock-out time, and press a delivery button to infuse the drug into himself/herself whenever necessary [19]. Data related to clinical experience with patient-controlled sedation indicate that patients are very satisfied with this sedation method because they were given the right to control the level of their anxiety or pain on their own [202122].
However, if a patient loses consciousness during patient-controlled sedation, he/she loses the ability to control himself/herself, and the feedback system falls apart [23]. Only well-designed drug infusion plans can help patients regain consciousness within a short period of time and restore the feedback system. This system always poses a risk of emergency situations such as airway obstruction upon excessive drug infusion. Therefore, patient-controlled sedation should be properly performed to assure patient safety. For effective sedation with little side effects, careful drug selection as well as determination of dose and lock-in time is necessary.
Sedatives used in patient-controlled sedation should have a fast onset of sedation, with an easily adjustable depth of sedation and duration of action. In addition, they should not cause any adverse effects such as cardiovascular inhibition or respiratory depression. A sedative is considered effective in patient-controlled sedation if it is able to bring about sedation soon after the patient presses a delivery button. For this reason, propofol is preferred over midazolam given its faster time to reach peak action [24]. Repeated pressing of the delivery button to reach the peak effect poses a risk of over-sedation due to repeated infusion [24]. Garip et al. administered 2 ml of midazolam (0.5 mg/ml) for 5 min by using the lock-out time method, and the result was more satisfactory than that of midazolam and remifentanil (12.5 µg/ml) mixed together [25]. However, midazolam is known to have a long recovery time, and may frequently cause sleepiness and mental derangement. Recently, cases in which dexmedetomidine is used have also been reported [2627].
A syringe pump used for patient-controlled sedation should infuse a fluid when a delivery button is pressed. The number of times the button was pressed and the actual infused amount should be displayed on the screen. Adjusting the settings of various features of the infusion pump is necessary for effective patient-controlled sedation. Therefore, the settings related to the single dose amount, infusion rate, and lock-out time should be adjustable. A single dose can be infused in a fixed amount (e.g. 2 ml, 10 mg, etc.). However, setting the infusion amount per kg of body mass by taking into account the drug concentration and the patient's body mass is also necessary. The maximum infusion rate of a single dose should be at least 1000 ml/h and must be adjustable. This feature that can set the infusion rate helps ensure patient safety. Since a delivery button may fall off of a patient's hand if he/she loses consciousness, a device that fixes the button to the patient's hand is also necessary. The alarm should produce a sound when the delivery button is pressed, in order to notify the patient and the medical staff alike.
The display screen should display the time elapsed since the delivery button was pressed, the number of times the button was pressed, the number of infusions, the remaining lock-out time, the total amount of drug infused, and the infusion rate, so that the patient has a good understanding of the situation.
1) Bolus dose refers to the dose that is infused when the delivery button is pressed. Typically, the infusion amount can be set as a fixed amount, or as the amount per kg of body mass (mg/kg or µg/kg).
2) Lock-out time starts after the infusion of a single dose is completed. During this time, no infusion occurs even when the delivery button is pressed. Many studies have performed patient-controlled sedation without setting the lock-out time. However, setting the lock-out time according to the drug's onset of action is important to ensure safety. For small doses, the lock-out time is adjusted to a short time window (0-1 minutes), and for large doses, it is adjusted to a long time window (3-5 minutes)
3) Basal infusion rate refers to the rate of continuous infusion. Additional amounts of the drug can be infused as a single dose. The basal infusion rate is rarely set in a patient-controlled sedation. However, setting the infusion rate may be helpful in preventing fluctuations in sedation depth [28].
4) Bolus dose infusion rate refers to the rate at which a single dose is infused when the delivery button is pressed. A recently developed pump boasts of an infusion rate of over 1500 ml/h. While it is believed that faster infusion rates allow for faster onset of sedative effects, infusion rates of over 1500 ml/h are not favorable due to complications such as breathing depression and other side effects caused by constraint in arm-brain time and increased drug concentration in the blood.
5) Initial loading dose: It can take a long time to reach the target sedation depth initially. By infusing an initial loading dose, the target sedation depth can be achieved sooner. In most sedation practices, an initial loading dose is not infused. Instead, patients are premedicated with analgesics or sedatives.
6) Maximum dose: This feature stops the drug infusion even when the lock-out time has passed and the patient has pressed the delivery button several times. This feature is necessary for ensuring patient safety.
Various features have been added to smart pumps used in dental sedation to increase patient safety. They include an alarm and a drug library, which provides drug information and prevents excessive infusion by limiting the infusion dose. In addition, programed infusion systems, target-controlled infusion systems, and patient-controlled infusion systems have been developed so that dentists can administer sedation more effectively. By fully utilizing the new features of smart pumps, more effective and safer dental sedation may be performed.
Figures and Tables
 | Fig. 1The user interface of the drug library editor program. The standard drug concentration and the soft and hard limits of the drug dose are entered here. A drug library of each drug made in this program is saved into the syringe pump and limits the drug dose during infusion. |
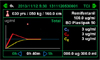
 | Fig. 2This is the LCD screen of the syringe pump control panel. The bolus dose (5 µg/kg), which is the loading dose, is infused for 10 minutes, and the infusion rate is decreased to 1.0 µg/kg/min. The VTBI (volume to be infused) is limited to 50 ml. |
 | Fig. 3An illustration of drug infusion by using target-controlled infusion (TCI). Once the target concentration (Ct) has been set, the infusion rate is automatically adjusted to reach the effect site concentration (Ce). By showing the change in concentration with time on a graph, one can also observe the pattern of changes in the plasma concentration (Cp). |
Table 1
Advanced features of smart pumps

Table 2
Drug library sample

Acknowledgments
This study was supported by the industrial innovation projects grant funded by the Ministry of Trade, Industry & Energy, Republic of Korea (No. 10049726).
References
1. Shim YS, Kim AH, Jeon EY, An SY. Dental fear & anxiety and dental pain in children and adolescents; a systemic review. J Dent Anesth Pain Med. 2015; 15:53–61.

2. Bae CH, Kim H, Cho KA, Kim MS, Seo KS, Kim HJ. A survey of sedation practices in the korean dentistry. J Korean Dent Soc Anesthesiol. 2014; 14:29–39.

4. Korean Society for Intravenous Anesthesia. Sedation. Seoul: Eui-hak Publishing & Printing Co;2004.

5. Kaufman E, Davidson E, Sheinkman Z, Magora F. Comparison between intranasal and intravenous midazolam sedation (with or without patient control) in a dental phobia clinic. J Oral Maxillofac Surg. 1994; 52:840–843.
6. Wilson K, Sullivan M. Preventing medication errors with smart infusion technology. Am J Health Syst Pharm. 2004; 61:177–183.
7. Larsen GY, Parker HB, Cash J, O'Connell M, Grant MC. Standard drug concentrations and smart-pump technology reduce continuous-medication-infusion errors in pediatric patients. Pediatrics. 2005; 116:e21–e25.

8. Mandel JE, Lichtenstein GR, Metz DC, Ginsberg GG, Kochman ML. A prospective, randomized, comparative trial evaluating respiratory depression during patient-controlled versus anesthesiologist-administered propofol-remifentanil sedation for elective colonoscopy. Gastrointest Endosc. 2010; 72:112–117.

9. Dohgomori H, Arikawa K, Kubo H. The accuracy and reliability of an infusion pump (stc-3121; terumo inst., japan) during hyperbaric oxygenation. Anaesth Intensive Care. 2000; 28:68–71.

10. Deckert D, Buerkle C, Neurauter A, Hamm P, Lindner KH, Wenzel V. The effects of multiple infusion line extensions on occlusion alarm function of an infusion pump. Anesth Analg. 2009; 108:518–520.

11. Murdoch LJ, Cameron VL. Smart infusion technology: A minimum safety standard for intensive care? Br J Nurs. 2008; 17:630–636.
12. Husch M, Sullivan C, Rooney D, Barnard C, Fotis M, Clarke J, et al. Insights from the sharp end of intravenous medication errors: Implications for infusion pump technology. Qual Saf Health Care. 2005; 14:80–86.
13. Goulding C, Bedard M. Safety implications of the dose change alert function in smart infusion pumps on the administration of high-alert medications. Can J Crit Care Nurs. 2015; 26:23–27.

14. Rothschild JM, Keohane CA, Cook EF, Orav EJ, Burdick E, Thompson S, et al. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Crit Care Med. 2005; 33:533–540.

15. Wakita R, Kohase H, Fukayama H. A comparison of dexmedetomidine sedation with and without midazolam for dental implant surgery. Anesth Prog. 2012; 59:62–68.

16. Chaudhri S, White M, Kenny GN. Induction of anaesthesia with propofol using a target-controlled infusion system. Anaesthesia. 1992; 47:551–553.

18. Struys MM, De Smet T, Depoorter B, Versichelen LF, Mortier EP, Dumortier FJ, et al. Comparison of plasma compartment versus two methods for effect compartment-controlled target-controlled infusion for propofol. Anesthesiology. 2000; 92:399–406.

19. Rudkin GE, Osborne GA, Curtis NJ. Intra-operative patient-controlled sedation. Anaesthesia. 1991; 46:90–92.
20. Osborne GA, Rudkin GE, Curtis NJ, Vickers D, Craker AJ. Intra-operative patient-controlled sedation. Comparison of patient-controlled propofol with anaesthetist- administered midazolam and fentanyl. Anaesthesia. 1991; 46:553–556.
21. Oei-Lim VL, Kalkman CJ, Makkes PC, Ooms WG. Patient-controlled versus anesthesiologist-controlled conscious sedation with propofol for dental treatment in anxious patients. Anesth Analg. 1998; 86:967–972.

22. Lok IH, Chan MT, Chan DL, Cheung LP, Haines CJ, Yuen PM. A prospective randomized trial comparing patient-controlled sedation using propofol and alfentanil and physician-administered sedation using diazepam and pethidine during transvaginal ultrasound-guided oocyte retrieval. Hum Reprod. 2002; 17:2101–2106.

23. Thorpe SJ, Balakrishnan VR, Cook LB. The safety of patient-controlled sedation. Anaesthesia. 1997; 52:1144–1150.
24. Rudkin GE, Osborne GA, Finn BP, Jarvis DA, Vickers D. Intra-operative patient-controlled sedation. Comparison of patient-controlled propofol with patient-controlled midazolam. Anaesthesia. 1992; 47:376–381.
25. Garip H, Gurkan Y, Toker K, Goker K. A comparison of midazolam and midazolam with remifentanil for patient-controlled sedation during operations on third molars. Br J Oral Maxillofac Surg. 2007; 45:212–216.

26. Chlan LL, Weinert CR, Skaar DJ, Tracy MF. Patient-controlled sedation: A novel approach to sedation management for mechanically ventilated patients. Chest. 2010; 138:1045–1053.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download