Abstract
Background
The objective of the present study was to examine the status of patients who had received dental treatment under intravenous (IV) sedation at Chungnam Dental Clinic for the Disabled in Korea from its inception to the present time, and to review the analysis results.
Methods
Retrospective analysis was performed on 305 cases of patients who had received dental treatments under IV sedation between January 2011 and May 2016. The analysis examined the patient's sex, age, primary reason for IV sedation, duration of anesthesia and dental treatment, type of dental treatment performed, number of clinical departments involved in the dental treatment and level of multidisciplinary cooperation, and annual trends.
Results
Most dental treatments using intravenous sedation were performed on medically disabled patients or dentally disabled patients with an extreme gag reflex or dental phobia. The mean duration of IV sedation was 72.5 min, while the mean duration of treatment was 58.0 min. The types of dental treatments included surgical treatment (n = 209), periodontal treatment (n = 28), prosthodontic treatment (n = 28), restorative treatment (n = 23), implant surgery (n = 22), endodontic treatment (n = 9), reduction of temporomandibular joint dislocation (n = 1), and treatment of traumatic injuries (n = 1), with treatments mostly performed on adult patients.
Dentally disabled patients include not only medically disabled patients with diminished ability to cooperate with or tolerate dental treatments, but also those with severe dental phobia and young children with limited ability to communicate. Various methods are needed to reduce the anxiety and phobias felt by these patients, and general anesthesia or sedation can be a proactive method. Considering the cost or hospitalization associated with general anesthesia, sedation can be a desirable alternative for controlling the anxiety and phobias associated with dental treatments, expanding the scope of dental treatments in some cases, and reducing the duration of hospitalization [1].
Among the various sedation methods that can reduce pain and anxiety, intravenous (IV) sedation has the advantage of rapid onset, allowing an appropriate sedated state to be maintained and drugs to be administered immediately under emergencies, since an IV line has already been secured. In addition, an IV central nervous system (CNS) depressant can control anxiety and induce amnesia [23].
Socioeconomic advancements, along with increased demand for oral health care and medical care for the disabled, have also led to increased demand for anesthetics to treat the dentally disabled [4]. In keeping with this trend, Chungnam Dental Clinic for the Disabled (CDCD) was established in December 2010 as part of the Dankook University Dental Hospital and the clinic has been providing the community with dental treatments for disabled patients and those who require general anesthesia or sedation.
The present study investigated the status of patients who had received dental treatments under IV sedation at CDCD since its inception to the present time, and herein reports the results of retrospective analysis of various factors.
The present study obtained the approval of the Institutional Review Board (IRB) of Dankook University Dental Hospital. The study retrospectively analyzed 305 cases by examining the medical records of patients who received dental treatments under IV sedation at CDCD between January 2011 and May 2016.
The procedures for performing IV sedation were as follows. A target controlled infusion (TCI) device (Orchestra Infusion Workstation, Fresenius Vial, France) was used for IV injection of propofol and remifentanil, at target concentration of 0.5 µg/mL and 1.0 µg/mL, respectively. First, remifentanil was administered at serum concentration controlled to 1.0 µg/mL, after which propofol at serum concentration of 0.5 µg/mL was injected under neuroleptanalgesia. In most of the adult patients, an IV line was secured using conventional venipuncture; for patients with difficulty in securing an IV line, a facial mask was used in the beginning to administer oxygen and nitrous oxide, each at a rate of 4 L/min for 2-3 min, to induce sedation and neuroleptanalgesia, after which the IV line was secured. After achieving adequate sedation, additional 2 L/min of oxygen was supplied using a nasal cannula, while also monitoring end-tidal carbon dioxide.
The medical records of patients who underwent dental treatments using IV sedation by these processes were collected for retrospective analysis of sex, age, primary reason for IV sedation, duration of anesthesia and dental treatment, type of dental treatment performed, number of clinical departments involved in the dental treatment and level of multidisciplinary cooperation, and annual trends.
Ages ranged between 5 and 85 years and most were adults: none in the 0-4 group (0%), 3 in the 5-9 group (1.0%), 16 in the 10-14 group (5.2%), 16 in the 15-19 group (5.2%), 66 in the 20-29 group (21.6%), 5 in the 30-39 group (18.4%), 67 in the 40-49 group (22.0%), 56 in the 50-59 group (18.4%), 17 in the 60-69 group (5.6%), 5 in the 70-79 group (1.6%), and 3 in the 80-89 group (1.0%).
The mean duration of IV sedation was 72.5 min and mean duration of dental treatment was 58.0 min.
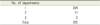
A total of 321 cases used IV sedation, and the types of dental treatments included surgical treatment (n = 209), periodontal treatment (n = 28), prosthodontic treatment (n=28), restorative treatment (n = 23), implant surgery (n = 22), endodontic treatment (n=9), reduction of temporomandibular joint (TMJ) dislocation (n = 1), and treatment of traumatic injuries (n = 1), with most treatments performed on adult patients.
Clinical departments that participated in the dental treatments were oral surgery (205 cases), advanced general dentistry (59 cases), periodontics (19 cases), prosthodontics (16 cases), restorative dentistry (16 cases), and oral medicine (1 case).
With respect to level of multidisciplinary cooperation during IV sedation, there were 11 cases of 2 departments cooperating together, while the remaining 294 cases were performed by a single department.
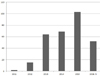
Since 2011, the number of cases involving IV sedation increased gradually up to May 2016.
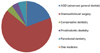
The reasons for choosing IV sedation included normal circumstances (n=151, 49.5%), gag reflex (n=49, 16.1%), dental phobia and/or anxiety (n = 36, 11.8%), dental phobia and/or anxiety and gag reflex (n = 3, 1%), mental retardation (n = 19, 6.2%), cardiovascular disease (n = 15, 4.9%), and multiple disabilities (n = 10, 3.3%). Other reasons are also listed in Table 5.
Dentally disabled patients include not only medically disabled patients with diminished ability to cooperate with or tolerate, but also those with severe dental phobia and young children with limited ability to communicate. For patients who are difficult to treat with general dental methods, behavior management with drugs can be selectively utilized. Drug-induced sedation can manage anxiety, phobias, and pain; since it can relax the muscles, it is used to provide safe, high-quality dental treatments in an efficient manner.
Among the various sedation methods that can reduce pain and anxiety, IV sedation has the advantage of rapid onset, allowing an appropriate state of sedation to be achieved, and drugs to be administered immediately under emergency situations since an IV line has already been secured [123]. Moreover, compared to general anesthesia, IV sedation also has the advantages of rapid recovery after treatment with fewer complaints of nausea and vomiting since the dosage can be titrated as needed, and there are less respiratory complications since intubation is not required.
In the present study, there were relatively more males (n=156) than females (n=149).
Patient ages ranged between 5 and 85 years and most were adults: none in the 0-4 group (0%), 3 in the 5-9 group (1.0%), 16 in the 10-14 group (5.2%), 16 in the 15-19 group (5.2%), and 270 in the ≥20 group (88.5%). The present study was able to confirm that IV sedation can be useful for dentally disabled patients who are of normal intelligence, but have severe anxiety over dental treatments [5].
For titration of effective depth of sedation, TCI equipment was used. In actual clinical settings, many changes can appear according to drug dosage due to pharmacological and pharmacokinetic variability. The use of TCI can prevent adverse effects from oversedation, while controlling anxiety and pain. TCI supplies a low dose of anesthetic that can be controlled during sedation, which reduces the risk of oversedation, and is able to maintain a steady concentration of drug and a consistent level of effect with rapid onset [678].
Although IV sedation has an advantage of rapid onset, its duration of effect is short; thus, it is an appropriate method for outpatient surgeries and treatments that require less than 2 h [9]. The present study showed mean IV sedation and treatment times of 72.5 and 58.0 min, respectively.
Among the drugs used for IV sedation, propofol is used most often, as it induces rapid sedation owing to rapid redistribution and metabolism, while having the benefit of recovery without residual effects [1011]. A burning sensation, which is an adverse effect of propofol, can be reduced by co-administering remifentanil, and adverse effects that can inhibit the cardiovascular system may be minimized through proper titration and use of TCI [12]. Remifentanil has a minimal residual effect and is a very fast-acting opioid analgesic [13]; combined use with propofol can shorten the recovery time by reducing the dose of propofol required to maintain sedation depth [14]. The combination of these two drugs is safe and effective, but since they may cause respiratory insufficiency, it is important to secure the airway [15].
A total of 321 dental treatments were performed under IV sedation, mostly on adults, and included: surgical treatment (n = 209), periodontal treatment (n = 28), prosthodontic treatment (n = 28), restorative treatment (n = 23), implant surgery (n=22), endodontic treatment (n = 9), reduction of TMJ dislocation (n = 1), and treatment of traumatic injuries (n = 1). The results showed that IV sedation was used mostly in highly-invasive procedures, such as extraction of wisdom or impacted teeth, implantation accompanied by bone grafts or maxillary sinus floor elevation, removal of cysts inside the oral cavity, and cases requiring a biopsy, where conscious sedation was needed for the purpose of reducing anxiety in normal adult patients [16].
In relation to the treatments provided, the clinical departments that participated included oral surgery (205 cases), advanced general dentistry (59 cases), periodontics (19 cases), prosthodontics (16 cases), restorative dentistry (16 cases), and oral medicine (1 case), with the highest participation rate for the department of oral surgery. The department of advanced general dentistry, which is responsible for general dental treatments and regular dental care of disabled patients, also accounted for a large portion, followed by the departments of periodontics, prosthodontics, and restorative dentistry, which were also involved in the treatment of dentally disabled patients.
With respect to level of multidisciplinary cooperation during IV sedation, there were 11 cases in which 2 departments cooperated, while 294 cases were performed by a single department. Few cases required multidisciplinary cooperation because the treatment in most cases aimed to complete the procedure within 2 h.
The number of IV sedation cases increased gradually from 2011 to May 2016. With increasing demand for minimally painful dental care, there is a trend of continued increase in the number of IV sedation cases, which is expected to continue as an alternative to general anesthesia [5]. Although priority candidates for IV sedation are those with American Society of Anesthesiologists physical status Class I, II, or above, the recent trend has been to broaden the candidate base for sedation to include patients with more severe systemic disorders, and to reduce physiological and mental stress. Therefore, to perform safe and satisfactory sedation, it is essential to be prepared with facilities, equipment, and personnel necessary to respond to emergency situations, as well as standardized patient monitoring devices and operators with clinical knowledge and experience [17].
IV sedation was performed in normal patients with dental anxiety (n = 151, 49.5%), and those with a gag reflex (n = 49, 16.1%), dental phobia and/or anxiety (n = 36, 11.8%), dental phobia and/or anxiety and gag reflex (n = 3, 1%), mental retardation (n = 19, 6.2%), cardiovascular disease (n = 15, 4.9%), and multiple disabilities (n = 10, 3.3%). Gagging can be classified as somatic or neurogenic. Somatic gagging occurs with physical stimulation of the area inside the mouth where gagging is triggered, while neurogenic gagging can be triggered by the dental treatment itself without a direct stimulus. In most dentally disabled patients, neurogenic factors plays a larger role, and sedation can be helpful [1819].
Pain and anxiety affect patients undergoing dental treatment. A study in the USA found that 6-14% of the population avoided going to the dentist due to dental phobia [20], while Murray et al. reported that anticipation and anxiety are the most important factors affecting the threshold for pain response [21]. Patients with much anxiety have a very low threshold for pain, and reducing anxiety significantly reduces the subjective sense of pain [22]. Therefore, it is necessary for dentists to minimize the stress that can be induced during treatment to reduce any risks the patient may face and to make the patient more comfortable [23]. Sedation used for such purposes can not only reduce anxiety, but can also maintain comfortable and safe conditions, while also reducing any unexpected movement or response by the patient during treatment [24].
Because IV sedation can induce anterograde amnesia that can erase memories of the negative experience of a difficult surgical process, it can also raise the threshold for phobia of dental treatment and the gag reflex in patients who successfully complete treatment under IV sedation [25].
CDCD has been selectively using appropriate sedation methods to provide high quality dental services to disabled patients, as well as to children and dentally disabled patients. In particular, for patients with anxiety and phobia of dental treatments, IV sedation can reduce the need for general anesthesia, while also providing a comfortable treatment environment.
The results of the present study analyzed patients who received dental treatments under IV sedation at CDCD over the past 6 years, and suggested that in anticipation of a further increase in demand in the future, methods for safer and more efficient IV sedation are needed.
Figures and Tables
Table 2
Duration of anesthesia and dental treatment (min.)
| Duration (min.) | |
|---|---|
| Duration of anesthesia | 72.5 |
| Duration of dental treatment | 58.0 |
Table 3
Dental treatment

Table 4
Number of clinical departments involved in dental treatment
| No. of departments | |
|---|---|
| 1 | 294 |
| 2 | 11 |
| 3 | 0 |
| Total | 305 |
Table 5
Primary reason for IV sedation

References
1. Dionne RA, Yagiela JA, Moore PA, Gonty A, Zuniga J, BEIRNE OR, et al. Comparing efficacy and safety of four intravenous sedation regimens in dental outpatients. J Am Dent Assoc. 2001; 132:740–751.

2. Kwak HJ, Kim JY, Kwak YL, Park WS, Lee KC. Comparison of a bolus of fentanyl with an infusion of alfentanil during target-controlled propofol infusion in third molar extraction under conscious sedation. J Oral Maxillofac Surg. 2006; 64:1577–1582.

3. Whitwam J. Co-induction of anaesthesia: Day-case surgery. Eur J Anaesthesiol Suppl. 1995; 12:25–34.
4. You YS, Kim JS, Kim SO. A survey of the outpatient general anesthesia and dental treatment in chungnam dental clinic for the disabled. J Korean Dent Soc Anesthesiol. 2011; 11:133–140.

5. Kim SO. A survey of general anesthesia, sevoflurane sedation and intravenous sedation in chungnam dental clinic for the disabled. J Korean Acad Pediatr Dent. 2013; 40:28–39.

6. McMurray T, Johnston J, Milligan K, Grant I, Mackenzie S, Servin F, et al. Propofol sedation using diprifusortm target-controlled infusion in adult intensive care unit patients. Anaesthesia. 2004; 59:636–641.

7. De Castro V, Godet G, Mencia G, Raux M, Coriat P. Target-controlled infusion for remifentanil in vascular patients improves hemodynamics and decreases remifentanil requirement. Anesth Analg. 2003; 96:33–38.

8. O JE, Kim JS, Kim SO. A study of intravenous sedation in dankook university dental hospital. J Korean Dent Soc Anesthesiol. 2013; 13:1–7.

9. O SR, Lee J. Intravenous sedation using propofol and midazolam in the exaggerated gag reflex patient's dental implant treatment. J Korean Dent Soc Anesthesiol. 2010; 10:27–33.

10. Sebel PS, Lowdon JD. Propofol: A new intravenous anesthetic. Anesthesiology. 1989; 71:260–277.
11. Tesniere A, Servin F. Intravenous techniques in ambulatory anesthesia. Anesthesiol Clin North America. 2003; 21:273–288.

12. Barash PG, Cullen BF, Stoelting RK. Clinical anesthesia. 5th ed. Lippincott Williams Willkins;2006. p. 269p. 270p. 341–342. p. 371p. 375
13. Glass PS, Dyar OJ, Jacobs JR, Reves JG. Intravenous anesthetic drugs: Infusion regimens. Int Anesthesiol Clin. 1991; 29:73–82.

14. Keidan I, Berkenstadt H, Sidi A, Perel A. Propofol/remifentanil versus propofol alone for bone marrow aspiration in paediatric haemato-oncological patients. Paediatr Anaesth. 2001; 11:297–301.

15. Dar AQ, Shah ZA. Anesthesia and sedation in pediatric gastrointestinal endoscopic procedures: A review. World J Gastrointest Endosc. 2010; 2:257–262.

16. Craig DC, Boyle CA, Fleming GJ, Palmer P. A sedation technique for implant and periodontal surgery. J Clin Periodontol. 2000; 27:955–959.

17. Pirwitz B, Schlender M, Enders A, Knauer O. [risks and complications anesthesia with intubation during dental treatment]. Rev Stomatol Chir Maxillofac. 1998; 98:387–389.
18. Saunders RM, Cameron J. Psychogenic gagging: Identification and treatment recommendations. Compend Contin Educ Dent. 1997; 18:430–433.
19. Kramer RB, Braham RL. The management of the chronic or hysterical gagger. ASDC J Dent Child. 1977; 44:111–116.
20. Weinstein P. Treating fearful dental patients: a patient management handbook. 2nd ed. University of Washington;1996.
21. Hodgkiss A. The puzzle of pain. Med Hist. 1996; 40:114–115.
22. Jones A, Bentler P, Petry G. The reduction of uncertainty concerning future pain. Journal of abnormal psychology. 1966; 71:87.

23. van Wijk AJ, Hoogstraten J. Reducing fear of pain associated with endodontic therapy. Int Endod J. 2006; 39:384–388.

24. Holzman RS, Cullen DJ, Eichhorn JH, Philip JH. Guidelines for sedation by nonanesthesiologists during diagnostic and therapeutic procedures. The risk management committee of the department of anaesthesia of harvard medical school. J Clin Anesth. 1994; 6:265–276.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download