Abstract
Background
The aim of this study was to compare the effectiveness and duration of action of two concentrations of bupivacaine with adrenaline for postoperative pain in patients undergoing surgical removal of four third molars under general anesthesia.
Methods
Sixty patients undergoing surgical removal of four wisdom teeth received bupivacaine 0.5% (n = 30) or 0.25% (n = 30). The severity of pain in the immediate recovery period and at 2 and 24 h after surgery was recorded using the visual analogue scale. Differences were assessed by box and whisper plot and the Student's t-test.
Pain is an unpleasant sensation that humans try to avoid. Management of pain has been of the utmost interest in the field of medicine since ancient times, particularly in dentistry. Today, there are many potent, long-acting, local anesthetic agents available to achieve satisfactory pain control during and after dental surgery. Third molar extraction has proven to be a suitable model for randomized controlled trials comparing different pain control agents [1].
A variety of local anesthetics has been developed to satisfy the specific requirements for different clinical procedures. Bupivacaine is often chosen for prolonged surgical procedures, such as removal of four wisdom teeth, due to its extended duration of anesthetic action [2]. Moreover, some authors have credited bupivacaine with the ability to achieve longer postoperative analgesia and to reduce analgesic requirements in the early postoperative hours when pain intensity is at its maximum. This feature is important given that postoperative pain is one of the main concerns for patients when undergoing a surgical procedure.
Bupivacaine is a common choice for pain control after removal of wisdom teeth. One of the amide group of local anesthetic agents, bupivacaine is marketed in several concentrations, the most common of which are 0.5% with 1:200,000 adrenaline and 0.25% with 1:400,00 adrenaline [3456]. Although bupivacaine has been used for a long time, there have been very few comparative studies assessing its analgesic efficacy at different concentrations [789].
The aim of this study was to compare the effectiveness and duration of action of two concentrations of bupivacaine commonly used in combination with adrenaline for pain control after surgical removal of four wisdom teeth under general anesthesia.
Sixty cases were calculated to be a reasonable sample size for a pilot study. Removal of four wisdom teeth under general anesthesia was used as a standard model to compare the different dose strengths of bupivacaine. The randomization method chosen was 60 colored sticks (30 for the 0.5% dose and 30 for the 0.25% dose), to be drawn from a bag by the study participants.
After receiving approval from the ethics committee at Holroyd Private Hospital (institutional review board approval number HPHMAC11082014:4.3), informed consent was obtained from the 60 patients. The patients were aged 16-42 years and scheduled for elective removal of four third molars.
Patients were excluded if they required emergency surgery or had known sensitivity to amide local anesthetics, fentanyl, or propofol; a known history of active renal, hepatic, respiratory, or cardiac disease; a blood disorder; or other reasons considered by the investigator to be grounds for exclusion.
Patients were randomized to receive 30 ml of bupivacaine 0.5% with adrenaline 1:200,000 or bupivacaine 0.25% with adrenaline 1:400,000 (Marcain®, AstraZeneca, Wilmington, DE, USA). The surgeon and anesthetist were blinded to dose allocation until the start of the procedure. The surgeon performed a bilateral inferior alveolar nerve block for each patient with local infiltration around the 18, 28, 38, and 48 areas. The same surgeon and anesthetist were involved in every case.
All patients were fasted and received no premedication. Peripheral intravenous access was used and intravenous induction was achieved with midazolam 1.5 mg, propofol 2 mg/kg, fentanyl 1 µg/kg, and atracurium 0.5 mg/kg. All patients underwent general anesthesia via nasotracheal intubation.
Patient age, American Society of Anesthesiologists status, body weight, operating time, amount of fentanyl given in recovery, and the postoperative visual analogue scale (VAS) pain score at 30 min, 2 h, and 24 h were recorded. Nurses in recovery and on the ward were also blinded to the dose allocation.
The VAS was used to document pain on three separate occasions. The VAS measures subjective pain between 1 and 100, 1 being no pain and 100 being severe.
It was not possible to standardize the degree of surgical difficulty preoperatively so operating time was used as a proxy measure.
Pain was measured during the immediate postoperative recovery period along with the requirement for supplementary analgesia. The second pain reading was taken before discharge 2 h after surgery and by telephone 24 h after surgery.
Four patients from the bupivacaine 0.25% group were lost to follow-up at 24 h. In the immediate postoperative recovery period, patients in the bupivacaine 0.5% group required marginally less supplemental analgesia than those in the bupivacaine 0.25% group (Table 1). There was no significant difference in intensity of pain between the groups 2 h postoperatively. Patients in both groups complained of variable levels of pain and use of oral analgesics. There was no statistically significant difference in mean patient age or duration of surgery between the groups, although the 0.5% group had a slightly longer operative time (Table 2). Similarly, there was no statistically significant difference in pain intensity at 24 h postoperatively.
The results of this study suggest the higher concentration of bupivacaine 0.5% provides better analgesia than the lower concentration of 0.25% (Fig. 1).
The box and whisker plot shows the 25th quartile, the median quartile (50th), and 75th quartile. When the spread among the 25th, 50th and 75th quartiles is less, the sample has less variance. This method is also used to reduce the impact of outliers in an analysis. In this study, spread among the 25th and 75th quartiles for bupivacaine 0.5% was less than that for bupivacaine 0.25% (Fig. 1).
In addition to the box and whisker plot, the Student's t-test was used to test for a statistically significant difference in ability to control pain between the 0.25% and 0.5% doses of bupivacaine. The Student's t-test is commonly used in medical research to check for statistically significant differences in effect between drug doses (Maeda et al, 2002) [10]. The Student's t-test is a tool for testing the null hypothesis where the means of two samples are equal and gives the probability that this is the case. If this probability is less than 0.05, the null hypothesis is rejected and the two samples are deemed to be significantly different (Table 1).
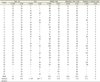
When the P-value is less than 0.05, the difference in effect between two different doses is significant. Therefore, the analgesic effects of the 0.25% and 0.5% doses were significantly different (P = 0.022) at 30 min after surgery but not after 2 and 24 h. The difference in the mean VAS scores for 0.25% and 0.5% was much higher after 0.5 h but less after 2 and 24 h (Fig. 2).
Bupivacaine is a commonly used long-acting amide local anesthetic and is effective in the management of postoperative pain. Its long duration of action and superior ability to decrease pain and discomfort have been reported in published comparisons of lignocaine and articaine. Bupivacaine is therefore the drug of choice for postoperative pain control after removal of the third molars [345678].
There are no comparative studies of two concentrations of bupivacaine reported in the literature especially in cases of wisdom teeth removal under general anesthesia [56].
Published comparisons of carbonated bupivacaine with adrenaline and noncarbonated bupivacaine with adrenaline have reported a significant difference in time to onset of anesthesia; however, this study was performed under local anesthesia and not all the wisdom teeth were removed [9]. A carbonated formulation would be difficult to use in Australia given that such products need regulatory approval and must be supplied in prepackaged vials.
In the present study, the efficacy of bupivacaine 0.5% and 0.25% with adrenaline was evaluated for its ability to reduce postoperative pain at three time points. Significant differences were observed in the immediate postoperative recovery period; patients who received bupivacaine 0.5% required less supplemental analgesia during this time (Fig. 1). This finding justifies the use of an increased concentration of bupivacaine.
It is often difficult to differentiate between anesthesia and pain until the patient is fully conscious and oriented [789]. In this study, the intensity of pain was similar in both the groups after 2 and 24 h, suggesting that patients were fully awake and oriented and could differentiate pain from anesthesia.
There was no difference in mean patient age between the two groups. There were more women in the bupivacaine 0.5% group and more men in the bupivacaine 0.25% group. While comparing body weight between the two groups, the bupivacaine 0.25% group was heavier and the operating time was slightly longer in the bupivacaine 0.5% group. To the best of our knowledge, there have been no reported studies comparing concentrations of bupivacaine for postoperative pain control after removal of four wisdom teeth under general anesthesia. Removal of four wisdom teeth is a very good model for comparing the postoperative effects of two different doses of an analgesic agent.
This study included only a small number of cases in each bupivacaine concentration group, so its findings will need to be confirmed in a larger study, preferably including assessment of patient-related variables potentially influencing the intensity of postoperative pain, such as psychological and socioeconomic status.
This study compared the postoperative analgesic efficacy of two commonly used concentrations of bupivacaine (0.25% and 0.5%) with adrenaline after surgical removal of impacted mandibular third molars under general anesthesia. The results showed that bupivacaine 0.5% provided better pain control immediately after surgery.
Figures and Tables
 | Fig. 1Box and whisker plot (bupivacaine 0.25% on left, bupivacaine 0.5% on right). Abbreviation: VAS, visual analogue scale. |
 | Fig. 2Mean VAS pain scores for bupivacaine 0.25% and bupivacaine 0.5% at 0.5, 2 and 24 h after surgery. Abbreviation: VAS, visual analogue scale. |
Table 1
Clinical findings of patients treated with bupivacaine 0.25% or 0.5%

Table 2
Distribution of age, sex, body weight, operating time, and amount of fentanyl used
Acknowledgments
The authors are grateful to Dr Mark Smith, Miss Mathilde Dacosta, Dr Paul Mackinnon and Mr Roobavanna Mahendran for their assistance with this research.
References
1. Sancho-Puchades M, Vilchez-perez M, Valmaseda-Castellon E, Paredes-Garcia J, Berini-Aytes L, Gay-Escoda C. Bupivacaine 0.5% versus 4% for the removal of lower third molars. A crossover randomized controlled trial. Med Oral Patol Oral Cir Bucal. 2012; 17:e462–e468.

3. Valpato MC, Ranali J, Groppo FC. Anaesthetic efficacy of bupivacaine solutions in inferior alveolar nerve block. Anaesth Prog. 2005; 52:132–135.

4. Moore PA. Bupivacaine: A long-standing local anaesthetic for dentistry. Oral Surg Oral Med Oral Pathol. 1984; 58:369–374.

5. Bouloux GF, Punnia-Moorthy A. Bupivacaine versus lidocaine for third molar surgery: adouble-blind, randomized, crossover study. J Oral Maxillofac Surg. 1999; 57:510–514.

6. Branco FP, Ranali J, Ambrosano GM, Volpato MC. A double-blind comparison of 0.5% bupivacaine with 1:200,000 epinepherine and 0.5% levobupivacaine with 1:200,000 epinepherine for the inferior alveolar nerve block. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:442–447.

7. Gregorio LV, Giglio FP, Sakai VT, Modena KC, Colombini BL, Calvo AM, et al. Comparison of the clinical anaesthtic efficacy of 4% articaine and 0.5% bupivacaine (both with 1:200,000 epinepherine) for lower third molar removal. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:19–28.

8. Nayyar MS, Yates C. Bupivacaine as pre-emptive analgesia in third molar surgery: randomized controlled trial. Br J Oral Maxillofac Surg. 2006; 44:501–503.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download