INTRODUCTION
Total thyroidectomy is the procedure of choice for treating several disorders of the thyroid gland. Total resection of glandular tissue, including the embryologic remnants is crucial for preventing the recurrence of goitre. Therefore, the completeness of thyroidectomy depends on total anatomical knowledge of the gland including anatomical variations, embryologic remnants, and ectopic tissue. The thyroid gland has the following 3 main embryologic remnants: pyramidal lobe (PL), Zuckerkandl's tubercle (ZT), and thyrothymic (TT) remnant. The thyroid remnant at the TT tract is sometimes entirely separate from the main lobe. The separate thyroid remnant is often overlooked or misidentified during surgery if it is inadequately explored. This embryologic structure involving the thyroidal tissue needs to be excised for total thyroidectomy. Small thyroidal tissue at the TT area is often misidentified as inferior parathyroid glands and lymph nodes [
12]. Sackett and Reeve [
2] have classified TT thyroidal extensions as grades I, II, III, and IV, of which grade IV small TT rests are frequently overlooked during thyroid surgery. Appropriate identification and excision of all remnants ensures the completeness of thyroidectomy and prevents recurrence of goitre [
1]. We observed some cases of an entirely separate remnant of the thyroid gland that was easily overlooked during thyroid surgery owing to nonmeticulous dissection at the TT tract. These remnants sometimes possess a considerable amount of thyroid tissue. Significant anatomical variations of embryologic origin threaten the completeness of thyroidectomy and cause recurrent disease.
In this prospective study, we aimed to determine TT thyroidal rests during thyroid surgery, particularly the separate remnant tissue of the thyroid gland.
Go to :

METHODS
The present study was approved by Institutional Review Board of Medical Faculty of Duzce University (IRB No. 2018-07-01). Our series was comprised of 134 consecutive patients who presented to our surgical clinic for primary thyroid surgery between January 2018 and June 2019. The patients with recurrent goitre who underwent redo-thyroid surgery were excluded. We routinely performed the exploration of the substernal area adjacent to the lower poles of thyroid lobes to identify separate embryologic remnants of the thyroid at the TT tract. In 134 patients who underwent primary thyroid surgery, 88 total thyroidectomies, and 30 left and 16 right hemithyroidectomies were performed. Therefore, 222 sides (118 left and 104 right sides) of the gland were examined, and 222 TT tracts were explored. The presence of separate thyroid remnants at the TT area was determined for patients undergoing primary thyroid surgery. According to the classification by Sackett and Reeve [
2], only grade IV thyroidal rests were evaluated in this study. Grade IV thyroid remnants are not attached to the thyroid gland and are an entirely separate thyroid tissue situated within the TT area. At the end of lateral lobe dissection, the TT region was carefully explored for the presence of separate thyroid remnants. All structures analogous to thyroid tissue were identified as separate thyroid remnants. All suspected remaining masses larger than 10 mm were dissected, surgically removed, and sent for histological examination. Histologically confirmed TT thyroid tissues were accepted as separate TT thyroid remnants.
Regarding the presence of PL at the pretracheal region and that of ZT, posterior embryologic appendages were also determined to establish the incidence of these embryologic remnants besides the TT rests. All the patients participating in this study signed an informed consent form.
Go to :

RESULTS
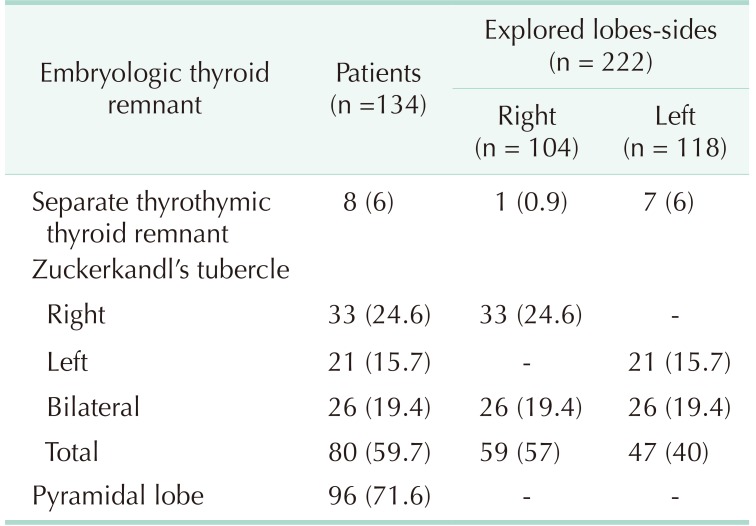
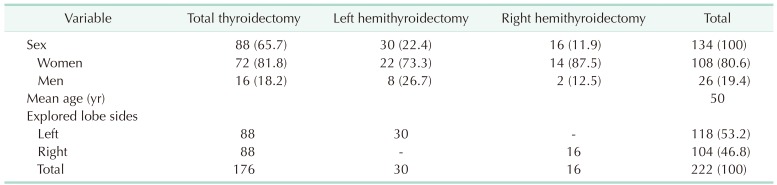
Of the 134 primary thyroid surgeries, 88 were for total resection and 46 were hemithyroidectomies. In 134 patients, 222 sides and lateral lobes were examined, and 222 TT areas were explored for separate thyroid remnants. There were 108 female patients (80.6%). The mean age of patients in the series was 50 years (range, 24–77 years) (
Table 1).
Table 1
Demographic features of patients, thyroid surgery technique, and explored sides
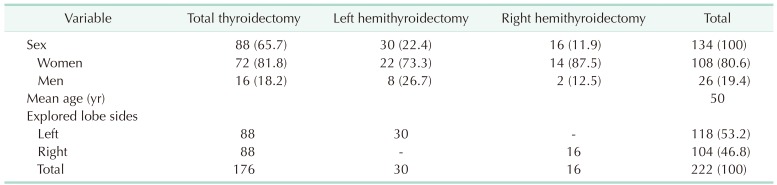

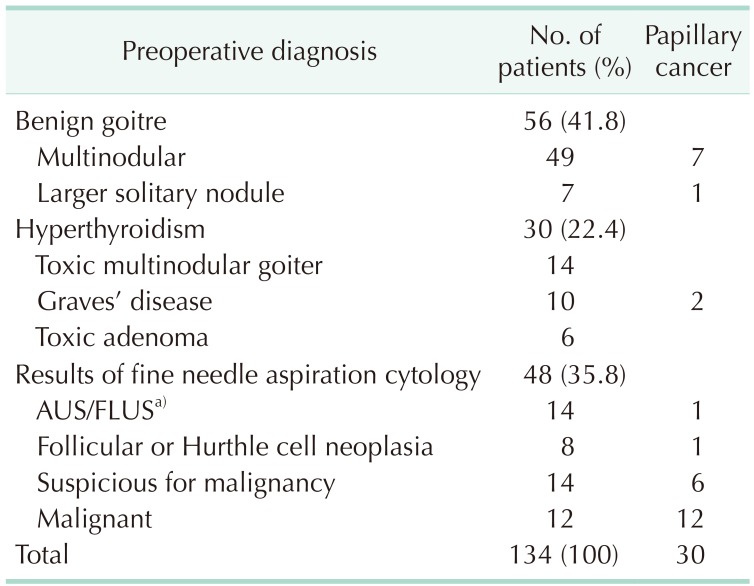
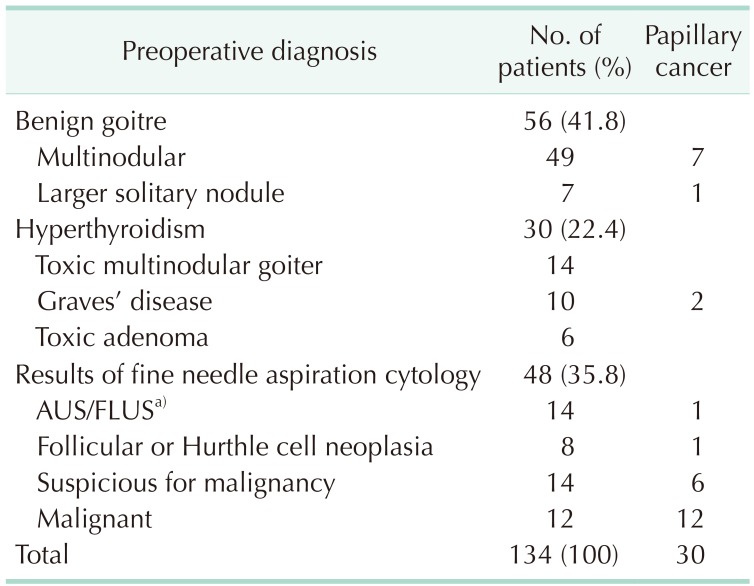
Indications for thyroid surgery were multinodular goitre and large solitary nodule in 56 patients (41.8%). In the remaining patients, the surgical indications were hyperthyroidism and indeterminate, suspicious, or malignant cytological results. Postoperative pathological examination revealed papillary cancer in 30 patients (22.4%) (
Table 2).
Table 2
Indications for thyroid surgery

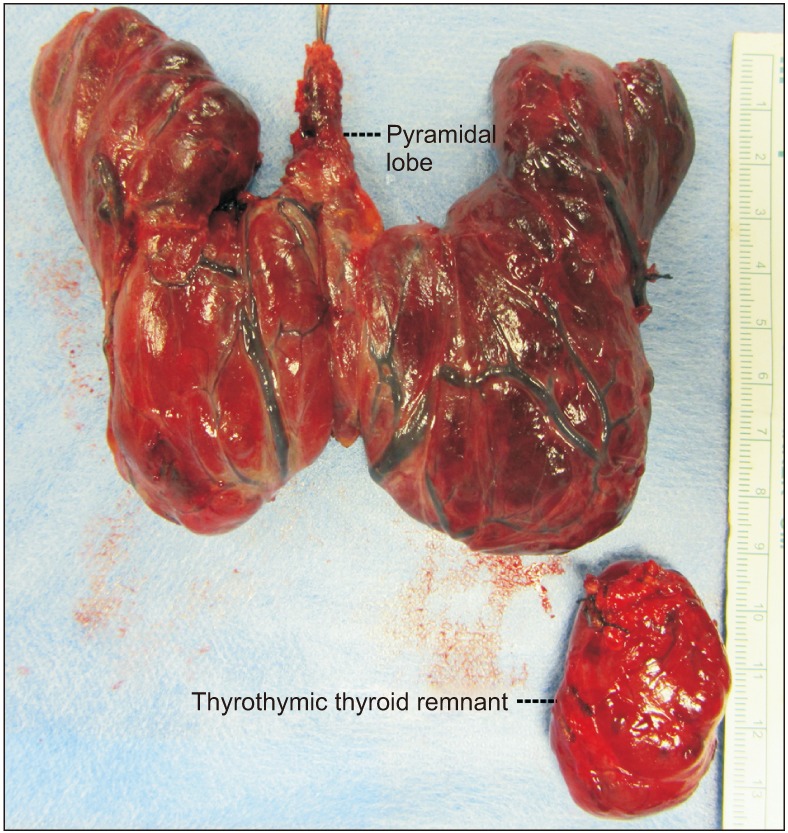
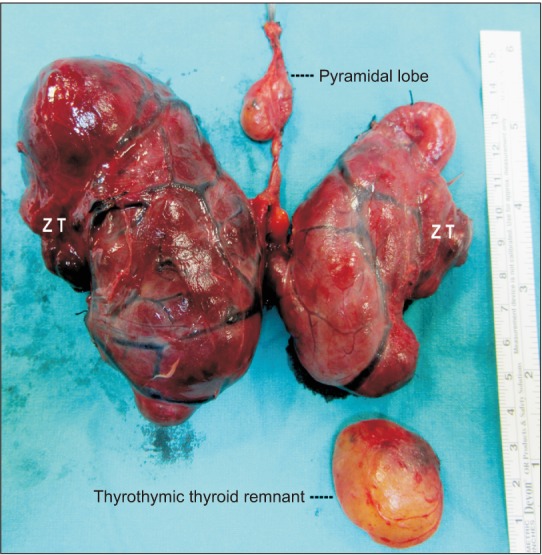
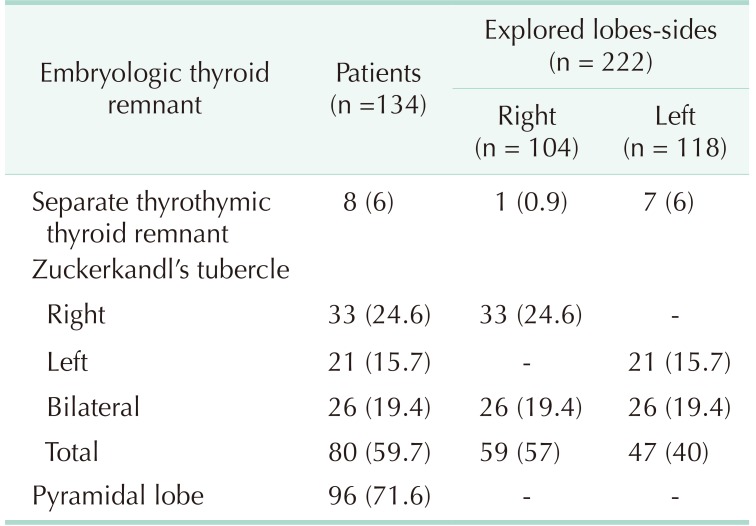
We explored 222 TT areas in 134 patients. Entirely separate thyroid remnants were identified and excised in 8 patients (6%). All embryologic remnants were unilateral—7 remnants were found on the left side and one on the right. The incidence of separate remnant was 6% at the left side (
Table 3). The mean size of excised remnants was 36.4 mm (range, 29–45 mm) with the largest remnant being 45 mm in diameter (
Fig. 1). In the present series, 96 patients (71.6%) had PL at the pretracheal region and 80 patients (59.7%) had ZTs. Overall, 106 ZTs (47.7%) were excised with 222 lobes of the thyroid gland. The incidence of ZT was 57% on the right and 40% on the left side (
Table 3). In addition, 4 patients with a separate TT thyroid remnant also had PLs (
Fig. 1). Four patients with separate thyroid remnant had both PLs and bilateral ZTs (
Fig. 2).
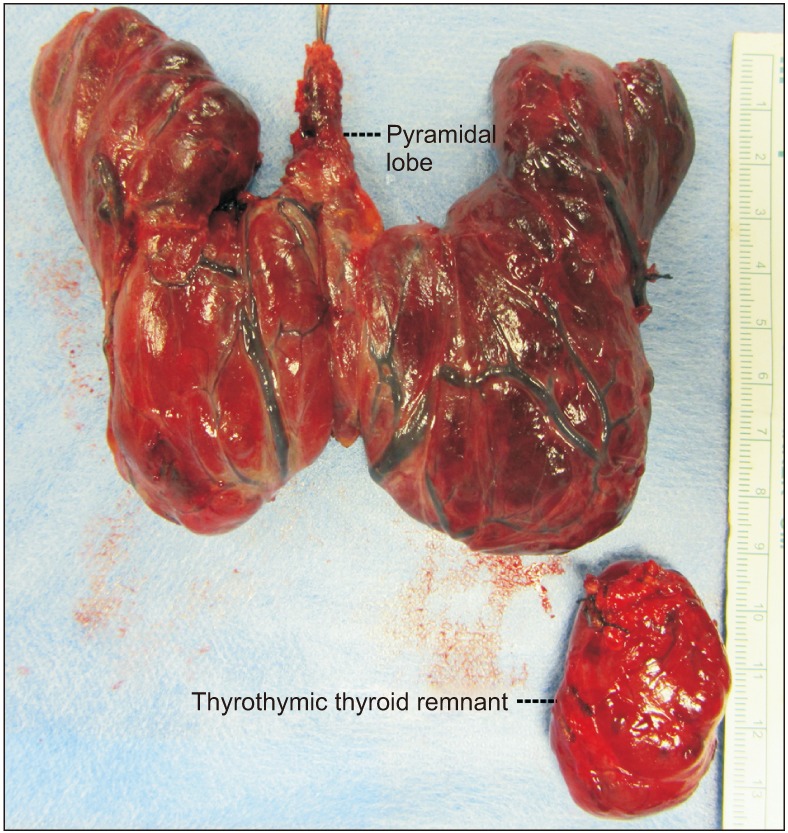 | Fig. 1Total thyroidectomy specimen with 2 embryologic remnants; the thyroid gland with pyramidal lobe and thyrothymic thyroidal remnant adjacent to lower pole of the left lobe. Largest separate thyroidal remnant at left thyrothymic tract.
|
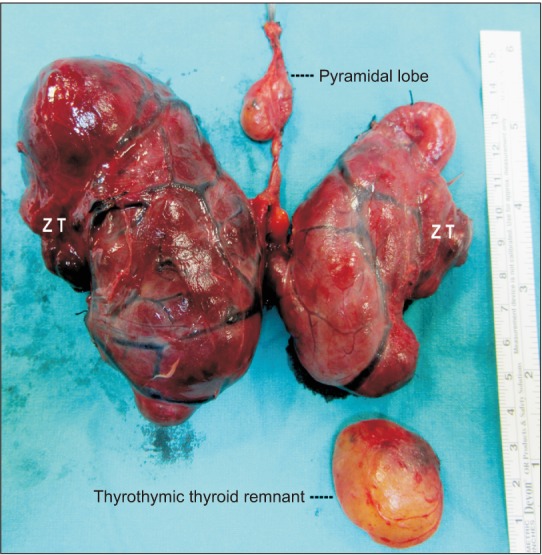 | Fig. 2Total thyroidectomy specimen with all 3 embryologic remnants; the thyroid gland with pyramidal lobe and bilateral Zuckerkandl's tubercles (ZT), and separate thyroidal remnant at left thyrothymic tract.
|
Table 3
Embryologic remnants in patients with thyroid surgery and in explored sides

Go to :

DISCUSSION
Some embryologic remnants of the thyroid gland such as PL, ZT, and TT remnants may complicate thyroid surgery. Sackett and Reeve [
2] have classified TT thyroidal extensions as grades I to IV. Notably, the grades I, II, and III extensions are attached to lower poles of thyroid lobes, but grade IV remnant has no connection with the main lobe of the thyroid. Typically, the identification, dissection, and removal of the attached extensions are not challenging when en bloc excision of lateral lobes is performed. On the contrary, entirely separate thyroid remnant at the TT tract can be disregarded during thyroidectomy. Separate rests may be overlooked if the surgeon is unaware of the potential presence of such remnants and if the TT area is not dissected properly. In the present series of thyroid surgeries, we routinely explored the TT area to detect separate embryologic remnants of the thyroid.
In this study, the incidence rate of 6% revealed the significance of such embryologic rests and validated that the presence of separate thyroidal remnant is not a rarity. Sackett and Reeve [
2] reported the presence of grade IV thyroidal remnants in 9 of 100 patients (9%), which again confirms the significance of this embryologic variation. Contrarily, Sheahan and O'Duffy [
3] reported only 1 case of separate rest at the TT region in a series of 262 patients. The presence of an ectopic thyroid, below its normal position and beyond the lower pole, may presumably be because of excessive migration during development [
134]. On the basis of our results and previous reports, we can comment that separate embryologic remnants at the TT tract may threaten completeness of thyroidectomy. Complete resection is not ensured if its significance is underestimated. Therefore, awareness of the inferior embryologic extension is critical to ensure total removal of thyroid tissue. The separate remnant may not be identified if the TT region is not explored [
34]. Its incidence in our series reveals the significance of separate thyroidal remnant in achieving “total” thyroidectomy. Delbridge [
5] noted that completeness of resection could be assured by considering an embryologically based approach rather than an anatomically based approach.
Larger remnants in our series reiterate our opinion regarding the significance of embryologic rests in achieving complete thyroidectomy when overlooked during surgery. In the literature, TT thyroid remnants larger than 10 mm in diameter are relatively uncommon. In the series of Sackett and Reeve [
2], 14% of TT thyroid rests were larger than 10 mm. Sheahan and O'Duffy [
3] reported marked nodular enlargement of the TT extension in a small number (<5%) of cases. In our series, the amount of thyroidal tissue in large remnants increases significance of separate rests in the TT region for total removal of glandular tissue. All embryologic remnants of the thyroid are critical for total thyroidectomy. The incidences of PL (71.6%) and ZT (59.7%) in this study were significantly higher than that of separate thyroid remnant at the TT area. On the basis of the frequency of PL, we suggest exploration of the pretracheal region up to the upper border of the thyroid cartilage or hyoid bone during surgery to achieve en bloc resection of the gland with PL. Notably, overlooked embryologic remnants may lead to recurrence. Considering the potential risk of recurrence from PL, its intraoperative identification and excision may decrease the risk of recurrence [
678]. ZT should be excised after careful dissection on the posterior side of the gland considering the proximity of the tubercle to the recurrent laryngeal nerve [
9]. The 2 embryologic remnants, PL and ZT, are attached to the gland, which makes it easier to excise these remnants during thyroid surgery if the surgeon is aware of their presence. In contrast, the separate TT thyroid rest in the retrosternal area is often overlooked owing to not being connected to the gland. Our series discovered some coexistence of embryologic remnants of the thyroid gland wherein relatively uncommon separate remnants at TT region coexist with other common remnants, PL and ZT.
The recurrence of goitre is a critical surgical problem if all thyroidal tissue, including the anatomic variations, is not removed during the initial surgery. Typically, some recurrences are associated with the embryologic remnants. Snook et al. [
10] reported the results of 3,044 total thyroidectomies performed for multinodular goitre, of which 10 patients developed recurrent goitre requiring reoperation despite previous “total” thyroidectomy. Of these, only one was a true local recurrence in the thyroid bed. The other 9 recurrences were related to the embryologic remnants of the thyroid gland, 4 in the pyramidal tract, and 5 in the TT tract. Failure to remove the embryologic remnants, such as TT residue or pyramidal remnants, during total thyroidectomy is the primary cause of recurrence [
10]. If the surgeon leaves the PL behind after total thyroidectomy, the leftover tissue has the potential to cause recurrence [
78]. Sackett and Reeve [
2] have reported 12 patients with retrosternal recurrence after previous total thyroidectomy. They presumed the retrosternal recurrences were related to forgotten TT rests during initial surgery. Recurrent goitre is often a rare occurrence after an initial total thyroidectomy and related to undetected embryologic remnants in the pyramidal tract, ZT, or TT region [
11]. Previous reports have established the role of TT thyroid rest on recurrent goitre. Cunha et al. [
12] reported a case of Graves' disease in a mediastinal thyroid mass presenting 7 years after total thyroidectomy for nontoxic goitre. Nuclear scan demonstrated increased intrathoracic uptake of radioiodine and a 60 × 40-mm mediastinal mass was confirmed through computer tomography. Therefore, we firmly believe that an embryologic remnant or ectopic thyroid tissue overlooked during initial surgery may lead to recurrence. Persistence of disease is yet another clinical complication after total thyroidectomy. Normal, nonelevated thyroid-stimulating hormone (TSH) level after total removal of the thyroid indicates persistent disease in the overlooked ectopic tissue during surgery. Sadacharan et al. [
13] reported a normal TSH level in a patient after total thyroidectomy with subsequent thyroid scintigraphy and chest MRI confirming thyroid tissue. Sahbaz et al. [
14] reported a normal serum TSH level a month following total thyroidectomy for papillary cancer with the thyroid nuclear scan revealing a mediastinal thyroid mass. Subsequent CT confirmed forgotten thyroid at the mediastinum. Therefore, we reiterate the significance of separate TT thyroid remnant in goitre recurrence or persistence after total thyroidectomy.
In conclusion, even though the literature has scant information regarding TT extension, the incidence of 6% in our series indicates that the presence of a separate TT thyroid remnant is not a rare variation. Large separate remnants often occur like a retrosternal third lobe of the thyroid gland. Such remnants may be easily overlooked if the TT area is inadequately explored during thyroid surgery. An overlooked remnant could lead to goitre recurrence or persistence. Awareness, identification, and excision of the embryologic remnants and the separate remnant at the TT area are critical to ensure completeness of thyroidectomy and prevent recurrences. We recommend routine exploration of the TT region during thyroid surgery owing to the relatively common presence of retrosternal unattached remnants.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download