Abstract
Purpose
This study aimed to identify the factors explaining the performance of health behaviors among adults with metabolic syndrome based on the theory of planned behavior.
Methods
A total of 218 adults with metabolic syndrome were recruited for the study from September to December, 2017. Data were analyzed using SPSS/WIN 22.0 and AMOS 24.0.
Results
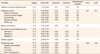
The hypothetical model appeared to fit the data with χ2/df=2.65, SRMR (Standardized Root Mean Residual)=.07, PNFI (Parsimonious Normed Fit Index)=.67. Attitude toward health behavior, subjective norm and perceived behavioral control explained 32.3% of variance in intention toward health behavior. Perceived behavioral control showed significant direct effects and mediating effect through intention on health behavior (γ=.57, t=5.85). Family support also had significant direct effects on health behavior (γ=.38, t=4.75). Attitude toward health behavior, subjective norm, perceived behavioral control, and family support were the significant factors explaining 56.3% of variance in the performance of health behaviors among patients with metabolic syndrome.
Conclusion
Health promotion programs for behavioral modification in this population should focus on these factors to lead to better health outcomes. Further studies are warranted to test the health promotion strategies based on theory of planned behavior for long-term change toward a healthy lifestyle among individuals with metabolic syndrome.
Figures and Tables
ACKNOWLEDGEMENT
This article is a revision of the first author's doctoral dissertation from Chungnam National University.
References
1. Opie LH. Metabolic syndrome. Circulation. 2007; 115(3):e32–e35. DOI: 10.1161/CIRCULATIONAHA.106.671057.

2. National Health Insurance Service (NHIS). 2016 Annual report on the statistics of physical examination [Internet]. Kangwondo: NHIS;c2018. cited 2018 April 27. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=342900.
3. Korea Health Statistics 2014; Korea National Health and Nutrition Examination Survey. 2015.
4. Shim JY, Kang HT, Kim SY, Kim JS, Kim JW, Kim JY, et al. Clinical practice guideline of prevention and treatment for metabolic syndrome. Korean Journal of Family Practice. 2015; 5(3):375–420.
5. Sun F, Tao Q, Zhan S. Metabolic syndrome and the development of chronic kidney disease among 118 924 non-diabetic Taiwanese in a retrospective cohort. Nephrology. 2010; 15(1):84–92. DOI: 10.1111/j.1440-1797.2009.01150.x.

6. Dalle Grave R, Calugi S, Centis E, Marzocchi R, El Ghoch M, Marchesini G. Lifestyle modification in the management of the metabolic syndrome: achievements and challenges. Diabetes, Metabolic Syndrome and Obesity : Targets and Therapy. 2010; 3:373–385. DOI: 10.2147/DMSOTT.S13860.


7. National Institutes of Health, and National Heart, Lung, and Blood Institute. Third report of the expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). Circulation. 2002; 3143–3421.
8. Grundy S. Diagnosis and management of the metabolic syndrome: an American heart association/national heart, lung, and blood institute scientific statement. Circulation. 2005; 112:2735–2752. DOI: 10.1161/CIRCULATIONAHA.105.169404.

9. Lee HJ, Jo B. Factors affection intentions for health behaviors among male office workers: an analysis based on the theory of planned behavior. Korean Journal of Occupational Health Nursing. 2002; 11(1):31–43.
10. Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991; 50(2):179–211. DOI: 10.1016/0749-5978(91)90020-T.

11. Rich A, Brandes K, Mullan B, Hagger MS. Theory of planned behavior and adherence in chronic illness: a meta-analysis. Journal of Behavioral Medicine. 2015; 38(4):673–688. DOI: 10.1007/s10865-015-9644-3.


12. Park S, Yang SJ. Factors Affecting health promotion behavior among workers with high risk of metabolic syndrome: based on theory of planned behavior. Journal of Korean Academy of Community Health Nursing. 2015; 26(2):128–139. DOI: 10.12799/jkachn.2015.26.2.128.

13. Costa V, Graça Pereira M, Pedras S. Partner support, socialcognitive variables and their role in adherence to self-monitoring of blood glucose in type 2 diabetes. European Diabetes Nursing. 2012; 9(3):81–86. DOI: 10.1002/edn.212.

14. Ferreira G, Pereira MG. Physical activity: the importance of the extended theory of planned behavior, in type 2 diabetes patients. Journal of Health Psychology. 2017; 22(10):1312–1321. DOI: 10.1177/1359105315626787.


15. Blue CL. Does the theory of planned behavior identify diabetes-related cognitions for intention to be physically active and eat a healthy diet. Public Health Nursing. 2007; 24(2):141–150. DOI: 10.1111/j1525-1446-2007.00618.x.


16. Peters RM, Templin TN. Theory of planned behavior, self-care motivation, and blood pressure self-care. Research and Theory for Nursing Practice. 2010; 24(3):172–186. DOI: 10.1891/1541-6577.24.3.172.



17. Plotnikoff RC, Lubans DR, Costigan SA, McCargar L. A test of the theory of planned behavior to predict physical activity in an overweight/obese population sample of adolescents from Alberta, Canada. Health Education & Behavior. 2013; 40(4):415–425. DOI: 10.1177/1090198112455642.


18. Lash DN, Smith JE, Rinehart JK. Can the Theory of Planned Behavior predict dietary intention and future dieting in an ethnically diverse sample of overweight and obese veterans attending medical clinics? Appetite. 2016; 99:185–192. DOI: 10.1016/j.appet.2016.01.013.



19. Monds LA, MacCann C, Mullan BA, Wong C, Todd J, Roberts RD. Can personality close the intention-behavior gap for healthy eating? An examination with the HEXACO personality traits. Psychology, Health & Medicine. 2016; 21(7):845–855. DOI: 10.1080/13548506.2015.1112416.

20. Chevance G, Caudroit J, Romain AJ, Boiché J. The adoption of physical activity and eating behaviors among persons with obesity and in the general population: the role of implicit attitudes within the Theory of Planned Behavior. Psychology, Health & Medicine. 2017; 22(3):319–324. DOI: 10.1080/13548506.2016.1159705.

21. Hagger MS, Hardcastle SJ, Hingley C, Strickland E, Pang J, Watts GF. Predicting self-management behaviors in familial hypercholesterolemia using an integrated theoretical model: the impact of beliefs about illnesses and beliefs about behaviors. International Journal of Behavioral Medicine. 2016; 23(3):282–294. DOI: 10.1007/s12529-015-9531-x.


22. Gilliss CL, Pan W, Davis LL. Family involvement in adult chronic disease care: reviewing the systematic reviews. Journal of Family Nursing. 2019; 25(1):3–27. DOI: 10.1177/1074840718822365.


23. Fleetwood S. A definition of habit for socio-economics. Review of Social Economy. 2019; 1–35. DOI: 10.1080/00346764.2019.1630668.

24. Oh SW. Metabolic syndrome; get it right prevent it right. Seoul: Chungrimlife;2012. p. 1–286.
25. Trief PM, Sandberg J, Greenberg RP, Graff K, Castronova N, Yoon M, et al. Describing support: a qualitative study of couples living with diabetes. Families, Systems, & Health. 2003; 21(1):57–67. DOI: 10.1037/h0089502.

26. Chesla CA, Fisher L, Skaff MM, Mullan JT, Gilliss CL, Kanter R. Family predictors of disease management over one year in Latino and European American patients with type 2 diabetes. Family Process. 2003; 42(3):375–390. DOI: 10.1111/j.1545-5300.2003.00375.x.


27. Fisher L. Family relationships and diabetes care during the adult years. Diabetes Spectrum. 2006; 19(2):71–74. DOI: 10.2337/diaspect.19.2.71.

28. Lee SY, Park HS, Kim SM, Kwon HS, Kim DY, Kim DJ, et al. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. The Korean Journal of Obesity. 2006; 15(1):1–9.
29. Bae BR. Structural equation modeling with Amos 19. Seoul: Chenngram Books;2011. p. 1–668.
30. Boudreau F, Godin G. Participation in regular leisure-time physical activity among individuals with type 2 diabetes not meeting Canadian guidelines: the influence of intention, perceived behavioral control, and moral norm. International Journal of Behavioral Medicine. 2014; 21(6):918–926. DOI: 10.1007/s12529-013-9380-4.

31. Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Medical Care. 2005; 43(5):436–444.


32. Song RY, Lee HJ. Effects of the inpatient cardiac rehabilitation program on behavioral modification and quality of life in patients with coronary artery disease. Journal of Korean Academy of Nursing. 2000; 30(2):463–475. DOI: 10.4040/jkan.2000.30.2.463.

33. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988; 52(1):30–41.

34. Song R, June KJ, Kim CG, Jeon MY. Comparisons of motivation, health behaviors, and functional status among elders in residential homes in Korea. Public Health Nursing. 2004; 21(4):361–371. DOI: 10.1111/j.0737-1209.2004.21410.x.


35. Kang KJ, Yu SJ. Health behavior and influencing factors in patients with coronary artery disease admitted to hospital. Journal of Korean Academy of Fundamentals of Nursing. 2010; 17(1):16–25.
36. Yu JP. The concept and understanding of structural equation modeling. Seoul: Hannarae Publishing Co.;2012. p. 1–567.
37. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986; 51(6):1173.


38. Conner M, Sparks P. Theory of planned behaviour and health behaviour. Predicting Health Behaviour. 2005; 2(1):121–162.
39. Bassi N, Karagodin I, Wang S, Vassallo P, Priyanath A, Massaro E, et al. Lifestyle modification for metabolic syndrome: a systematic review. The American Journal of Medicine. 2014; 127(12):1242.e1–1242.e10. DOI: 10.1016/j.amjmed.2014.06.035.
40. Araújo-Soares V, McIntyre T, Sniehotta FF. Predicting changes in physical activity among adolescents: the role of self-efficacy, intention, action planning and coping planning. Health Education Research. 2009; 24(1):128–139. DOI: 10.1093/her/cyn005.


41. Kim TK, Min HS. A structural model of alcohol abstinence behavior among patients with chronic liver diseases. Korean Journal of Adult Nursing. 2018; 30(1):30–40. DOI: 10.7475/kjan.2018.30.1.30.

42. Lakerveld J, Bot SD, Chinapaw MJ, Knol DL, de Vet HC, Nijpels G. Measuring pathways towards a healthier lifestyle in the Hoorn Prevention Study: the Determinants of Lifestyle Behavior Questionnaire(DLBQ). Patient Education and Counseling. 2011; 85(2):e53–e58. DOI: 10.1016/j.pec.2011.01.014.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download