Abstract
PURPOSE
The aim of the current study was to analyze treatment concepts of a cohort of German dentists for planning, fabrication, and maintenance of implant-supported fixed and removable restorations.
MATERIALS AND METHODS
A questionnaire including queries about experiences with implant-supported restorations as well as prosthetic and maintenance treatment concepts for supplying patients with fixed and removable implant-supported prosthetic restorations was developed and sent to 350 dental offices registered in the municipal area of Leipzig, Germany.
RESULTS
An overall total of 62 returned questionnaires were included in the analyses, which relates to a response rate of 17.7%. Participating dentists were more involved in the prosthetic aspects of implant dentistry rather than surgery, while prosthetic concepts such as backward planning, digital processing, and application of all-ceramic materials were not commonly performed. Simple attachments were preferred over complex retention systems in removable implant-supported restorations. Tooth/implant-supported fixed denture prostheses as well as removable denture prostheses with supporting posterior implants were not regarded as a favorable treatment option.
CONCLUSION
Within the limitations of the study, the data indicate that dentists favor simple and conventional treatment approaches in implant prosthetics. Prosthetic aspects in the planning of implant-supported restorations are often neglected. Prosthetic treatment guidelines and aspects should commonly be considered in the planning phase of implant-supported prosthetic restorations, and awareness should be increased in postgraduate education.
Implant-supported prosthetic restorations play an important role in contemporary prosthetic dentistry. According to the American Academy of Implant Dentistry (AAID), about three million people in the US wear dental implants and this number is increasing by 500,000 people every year.1 In Germany, the German Society for Implant Dentistry (DGI) estimates about one million dental implants inserted every year.2
Dental implants feature a very high rate of success, which means that survival rates for dental implants range more than 90% after 10 years of clinical service.345 Nevertheless, technical and biological complications are regularly observed in implant-supported restorations. Technical complications include fractures of the implant or abutment or problems with the associated prosthetic superstructure such as chipping of the veneering, loosening or fracture of abutment screws, or wear and loss of retention in attachment systems. For both fixed and removable implant-supported denture prostheses, numerous prosthetic treatment options are available. Those include the attachment system for removable restorations (bars, double crowns, studs) or, for fixed restorations, abutment design (conventional vs. individualized), abutment material (titanium, zirconia, hybrid, cast), or the restoration (material, veneering). While it has recently been highlighted that technical complications in implant-supported prosthetic restorations cannot be completely avoided,6 it is clear that the frequency of technical complications depends on the individual treatment concept as well as the materials and components used for the fabrication of the restorations.
Biological complications include periimplant mucositis and periimplantitis. Periimplant mucositis is defined as an inflammation of the mucosa surrounding an implant with no sign of loss of supporting bone, whereas periimplantitis is characterized by loss of supporting bone in addition to mucosal inflammation.7 Both diseases are associated with biofilms on the surface of the implant or the prosthetic components as several studies identified a relation between discontinued oral hygiene in patients with implants and the onset of periimplant mucositits.89 A recent review reported a prevalence of periimplant mucositis ranging around 43% and of periimplantitis around 22%.10 These data underline the relevance of regular removal of biofilms by means of dental prophylaxis. With regard to this aspect, a recent meta-analysis highlighted that lacking prophylaxis may substantially increase the risk for periimplantitis.11 Thus, the maintenance concepts employed in the dental practice play an important role for avoiding biological complications.
Currently, there are no scientific data available on the concepts German dentists employ for supplying patients with implant-supported restorations. Thus, the aim of the current study was to investigate the treatment concepts applied by a cohort of German dentists in patients requiring implant-supported prosthetic restorations as well as to investigate concepts applied for prosthetic follow-up care and maintenance.
The study was performed in accordance with the Standards for Reporting Qualitative Research (SRQR) guidelines. A questionnaire was developed by three dentists experienced in implant prosthetics and scientific surveys to identify the treatment concepts dentists employ in patients requiring implant-supported fixed and removable denture prostheses. The questionnaire comprised three sections and included almost entirely closed questions; in some cases, multiple answers were possible.
The first section dealt with general characteristics, including age of the participating dentists, the estimated number of implants supplied with prosthetic restorations every quarter of a year, and whether the dentists had completed postgraduate education in implant surgery and/or prosthodontics. Dentists were also asked to indicate which steps in implant restorations are performed by themselves and whether they regularly adhere to a backward planning concept.
The second section of the questionnaire included three pictograms displaying different clinical settings, including a single-tooth gap in the anterior upper jaw (Fig. 1). The dentists were asked to select their preferred treatment options for an implant-supported restoration in regio 21 from a variety of offered options regarding type of abutment, type of prosthetic superstructure, as well as their preferred option for inserting the final restoration. Another pictogram included the setting of a bilaterally shortened dental arch in the lower jaw (Fig. 2) with fixed opposing dentition. Dentists should indicate treatment concepts as favored or non-favored (i.e. restoration with implant-supported single crowns, implant supported fixed partial dentures, tooth-/implant-supported fixed partial dentures, removable denture with supporting posterior implant). In the last setting, dentists were questioned about how many implants they would insert in edentulous upper jaw with a fixed opposing dentition for supplying the patient with an implant-supported restoration and which type of attachment system (i.e. Locator, ball, double crown, bar) they would preferably use in this setting.
The third part of the questionnaire addressed procedures associated with follow-up care, including recall intervals, associated X-ray examinations, measurement of pocket depths, and methods applied for biofilm removal.
One questionnaire and an information sheet were sent to all dental practices in the municipal area of Leipzig, which were registered in the index of the regional dentists' association. Leipzig is a major city in Saxony, Germany, with an overall population of approximately 595,000 inhabitants. The participants were asked to complete the questionnaire and to return it anonymously in an enclosed stamped and addressed return envelope in a single round; no reminders were sent. Due to the design of the study, no approval by an ethics committee was required.
Data were extracted from the completed questionnaires, transferred into an electronic file for data exploration, and checked by an independent dentist. Frequencies were calculated using IBM SPSS Statistics 24.0.0.0 (IBM, Armonk, NY, USA).
Questionnaires were sent to all 350 registered dental offices in the municipal area of Leipzig, Germany. 62 questionnaires were returned, which relates to a response rate of 17.7%.
Dentists participating in the survey had a mean age of 50.1 ± 10.3 years (no response: 4.8%) and 68.3% had completed postgraduate training courses in implant dentistry and/or implant prosthetics (no response: 3.2%). 3.2% of the participating dentists indicated that they never took part in postgraduate courses in implant prosthetics, while 35.5% indicated that they completed a course annually and 11.3% biannually. 41.9% issued that they occasionally take part in postgraduate courses dealing with implant prosthetics (no response: 8.1%). Quarterly, each dentist supplied a mean of 12.6 ± 18.4 implants with prosthetic restorations (no response: 6.5%). 61.3% indicated that they performed the planning of implant restorations themselves (no response: 3.2%), and 44.7% of the latter regularly used backward planning approaches. 29.0% of the participating dentists responded that they performed implant placement (no response: 3.2%), and 24.2% that they performed mucogingival surgery (no response: 3.2%). 91.9% issued that they supply dental implants with prosthetic restorations themselves (no response: 4.8%). A total of 64.5% reported that they adhered to a conventional therapeutical approach in their dental office, 22.6% responded that they used both conventional and digital methods, and 8.1% specified that they were working completely digitally (no response: 4.8%).
Regarding the choice of abutments in implant restorations in a single-tooth gap in the anterior upper jaw (regio 21), 14.5% of the participating dentists issued that they used titanium abutments, 4.8% abutments fabricated from precious alloys, 38.7% zirconia abutments, and 12.9% hybrid abutments (Table 1; no response: 29.4%). 45.2% indicated that they employed individually fabricated abutments and 4.8% conventional abutments (no response: 50.0%). Abutments were supplied with porcelain-fused-to-metal crowns (9.7%), crowns fabricated from lithium disilicate ceramic that had been painted (3.2%) or veneered (19.4%), monolithic zirconia (11.3%), or veneered zirconia (46.8%) (Table 2; no response: 9.7%). Regarding the insertion of the single crowns, 59.7% preferred cementation procedures, 16.1% screw-retained restorations, and 14.5% employed both approaches with a similar frequency (no response: 9.7%). Those who preferred cementation used conventional dental cements (37.5%) rather than provisional (33.3%) and adhesive cements (29.2%), and those who favored screw-retained restorations preferred an oral localization of the screw (63.2%) rather than an occlusal localization (36.8%).
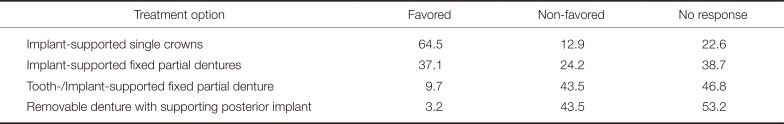
Regarding the bilaterally shortened dental arch in the lower jaw (Table 3), 64.5% indicated a restoration with implant-supported single crowns as favored treatment option (non favored: 12.9%, no response: 22.6%). 37.1% issued restoration with implant-supported fixed partial dentures as favored treatment option (non favored: 24.2%, no response: 38.7%), and 9.7% regarded tooth-/implant-supported fixed partial dentures as a favorable treatment option (non favored: 43.5%, no response: 46.8%). 3.2% indicated a removable denture with supporting posterior implant as a favorable treatment option (non favored: 43.5%, no response: 53.2%).
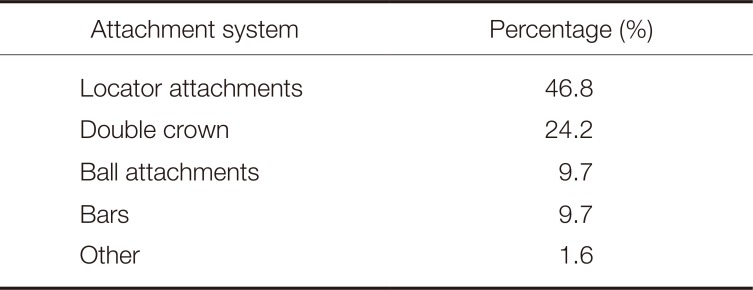
With regard to rehabilitation of an edentulous upper jaw with implant-supported restorations, the majority of participating dentists would preferably insert four implants (62.9%), followed by six implants (11.3%), two implants (3.2%), and three/eight (1.6%) implants (no response: 21.0%). 46.8% preferred attachments such as the Locator system as retentive element, while 24.2% favored double crowns and 9.7% preferred bars and ball attachments, respectively (other: 1.6%, no response: 8.1%; Table 4).
85.5% of the participating dentists stated that they offered a follow-up care program for patients with implant-supported restorations (no response: 4.8%). From these dentists, 84.9% responded that they controlled the implant-supported restorations twice/year, while 11.3% indicated that controls were performed once/year and 1.9% quarterly (no response: 1.9%). 58.0% of the participating dentists reported that they performed X-ray examinations of implant-supported restorations at least biannually and 38.7% only occasionally (no response: 3.2%). 82.3% indicated that they probed periimplant tissues (no response: 3.2%), using either polymeric probes (46.8%), WHO probes (35.5%), or pressure-calibrated probes (1.6%) (no response: 16.1%).
Professional cleaning of implants and implant-supported restorations was performed either by dental nurses (48.3%), dental nurses specialized in prophylaxis (44.8%), dental hygienists (3.4%), or dentists (3.4%). Most frequently, chlorhexidine was employed during prophylaxis (58.3%), followed by application of air-abrasive powder (33.3%), ultrasonic scalers (28.3%), sonic scalers (5.0%), and manual instruments (3.3%) (no response: 3.2%, multiple answers possible).
The data of the current study help outline the concepts and procedures that are currently applied in dental offices regarding planning, fabrication, and insertion of implant-supported prosthetics as well as their maintenance. Nevertheless, the authors are aware that data gathered in a single major city are not fully representative, as regional differences may exist in treatment concepts depending on different education programs in universities and socioeconomic discrepancies within different areas of Germany. In addition to that, the response rate of 17.7% was rather low, which suggests that a vast number of dentists were not interested in taking part in the survey. A recent study of the authors that had been performed in a district of Bavaria featured a slightly higher response rate of 22.7%,12 which might be due to the fact that in the latter study the questionnaire was sent to each registered dentist rather than each registered dental office. However, due to the recent modifications in data privacy laws, it was not possible to address the dentists directly. Moreover, the questionnaire was sent to all registered dental offices in the municipal area of Leipzig, and it might be possible that colleagues specialized in orthodontics or maxillofacial surgery did not return the questionnaire at all. In previous investigations, many returned questionnaires were not fully completed,12 indicating that the questionnaires might have been too extended or complex to answer. Thus, the authors of the present investigation decided to include only a selection of potential prosthetic settings to be supplied with implant-supported restorations and to illustrate the settings with pictograms. Nevertheless, the authors received several questionnaires which were only partially completed.
Data indicated that the vast majority of the participating dentists regularly supply patients with implant-supported restorations. Surprisingly, the number of dentists who performed planning of implant placement and used backward planning approaches was markedly lower. This observation suggests that dentists do not commonly adhere to the current scientific concept that the position of an implant should be planned in accordance with prosthetic principles.13 With regard to this aspect, it has recently been addressed that dental technicians play a crucial role in decision making, suggesting that the prosthetic knowledge of dentists should be steadily increased.14 More than 40% of the participating dentists indicated that they never or only occasionally took part in postgraduate courses in implant prosthetics, which underlines that prosthetic aspects might still be neglected in implant dentistry. The mean age of the participating dentists was higher than 50 years, indicating that the outcome of the current study might be different in younger dentists who have a more detailed education in implant prosthetics at an undergraduate level. These observations and considerations coincide with the results from other trials, which reported that particularly residents, dentists specialized in prosthodontics, and general dentists with a professional experience of less than 15 years applied modern prosthetic concepts in implant dentistry.15 While - to the knowledge of the authors - modern prosthetic concepts in implant dentistry are an important part of the curriculum in German universities and are taught in an extensive number of different postgraduate education courses, researchers from other countries highlighted that education in implant dentistry in both undergraduate and postgraduate courses is not satisfying.16 With regard to this aspect, recent studies support the thesis that decision-making in dentistry is relevantly impacted by experience and education.171819 Furthermore, it has been reported that a large proportion of graduating dental students does not feel prepared or well-prepared in implant dentistry,20 and other researchers underline that clinical experience with implants and implant-supported restorations should be implemented in the curricula.21
Moreover, the data of the current study highlighted that the application of digital treatment approaches was not common, although a recent study concluded that digital workflows have a promising future.22 Current scientific evidence highlights that the application of digital techniques such as computer-aided implant surgery may be beneficial and optical impressions for the fabrication of implant-supported prosthetic restorations with a limited number of units can be reliably performed.23 However, as digital impression techniques are not recommended for restorations with large spans and in edentulous jaws,23 it might be possible that dentists are still reluctant to integrate these approaches into their daily dental routine. Regarding the high mean age of the dentists participating in the current study, it might also be possible that digital approaches are more common among younger dentists.
Regarding replacement of an upper central incisor with an implant-supported single crown, the majority of participating dentists used either zirconia or hybrid abutments. However, while all-ceramic or hybrid abutments feature advantages in the esthetic appearance of the prosthetic restoration, surprisingly many dentists favored titanium abutments or abutments fabricated from precious alloys. A recently published systematic review highlighted that both metal and ceramic abutments supporting single crowns feature high clinical survival rates, with significantly lower abutment fractures in metal abutments.24 Surprisingly, zirconia abutments were favored more frequently than hybrid abutments, which show higher fracture resistance in laboratory studies.25 With regard to the implant-supported single crown, the majority of participating dentists favored the use of all-ceramic materials, and the majority of dentists issued that they preferred veneered restorations rather than monolithic ones. With regard to this aspect, recent meta-analyses underlined that both porcelain-fused-to-metal and veneered zirconia can be reliably used for the fabrication of implant-supported single crowns.26 Most of the participating dentists preferred cementation of implant-supported single crowns rather than screw-retention. This observation was surprising, as recent recommendations support the application of screw retention in implant-supported restorations in the anterior area.27 While 5-year clinical survival rates are similar for both screw-retained and cemented implant-supported restorations, screw-retained restorations feature less technical and biological complications.28 However, for employing screw-retained approaches in implant dentistry, an ideal prosthetic position of the implant is required. As only a minority reported that they regularly employed backward planning techniques, it might be possible that screw-retention was regularly not possible. Again, these considerations underline that the position of an implant should be planned in strict accordance with prosthetic principles. With regard to the choice of cement, Korsch and co-workers identified a relevant impact of excess cement in patients with cemented implant-retained restorations on the prevalence of periimplant inflammations,29 also observing that the application of acrylic cements regularly coincides with an excess of cement.30 The majority of dentists in the current study used conventional or provisional dental cements; however, approximately one third used adhesive materials which can be critically discussed against this scientific background.
In bilaterally shortened dental arches, rehabilitation with implant-supported single crowns was the option of choice for the majority of participating colleagues, followed by implant-supported fixed partial dentures. Tooth-/implant-supported fixed partial dentures were favored by merely 10%, suggesting that participating dentists doubt the clinical success of these restorations. This observation might be explained by the conventional wisdom that deformation of the mandibular during excursive movements, resulting in strain on combined tooth-/implant-supported restorations. However, recent reviews indicate that tooth-/implant-supported fixed dental prostheses have a survival rate of 90.8% after five years and 82.5% after ten years of clinical service, underlining that these constructions are a treatment option that can be recommended in partial dentition.31
Current guidelines and scientific evidence stress that implant-supported restorations of edentulous upper jaws require a minimum of four supporting implants.1332 The data gathered in the current study indicate that the vast majority of dentists adheres to these guidelines and only few colleagues would prefer to insert less than four implants. Regarding prosthetic rehabilitation, simple attachment systems such as the Locator system were preferred over more complex attachments such as double crowns or bars. Although several studies underline that the attachment system selected for retention of implant-supported overdentures has only little influence on patient satisfaction,3334 these observations were surprising as overdentures with more complex retention elements can be fabricated in a more gracile manner. Previous studies have also highlighted that simple attachment systems feature extensive wear and degradation and may require extensive maintenance procedures.3536
Treatment guidelines demand regular control of implants in implant-supported prosthetic restorations, which is particularly relevant in patients with periodontitis and in patients with implant placed in augmented areas.37 Data of the current investigation suggest that follow-up care programs are regularly offered and almost 85% of the dentists control implant-supported restorations twice/year within follow-up programs. In contrast, less than 60% of the participating dentists performed biannual X-ray analyses in implant-supported restorations. A recent review recommends regular and - unless shorter periods are required for specific requirements - biannual radiographic control.38 Besides, it was suggested that participation in postgraduate education programs on current concepts in the maintenance of implant restorations might be appropriate.
Within the limitations of the current study, it can be concluded that dentists do not regularly adhere to prosthetic principles in implant dentistry. Fostering the participation of experienced colleagues in postgraduate courses dealing with implant prosthetics might help improve the clinical performance of implant-supported restorations inserted in dental offices.
References
1. American Academy of Implant Dentistry (AAID). What are dental implants? 2019. Accessed January 25, 2020. Available at: https://www.aaid-implant.org/dental-implants/what-are-dental-implants/.
2. German Society for Implant Dentistry (DGI). Implants. 2019. Accessed January 25, 2020. Available at: https://www.dginet.de/web/dgi/warum.
3. Paquette DW, Brodala N, Williams RC. Risk factors for endosseous dental implant failure. Dent Clin North Am. 2006; 50:361–374. PMID: 16818020.

4. Norowski PA Jr, Bumgardner JD. Biomaterial and antibiotic strategies for peri-implantitis: a review. J Biomed Mater Res B Appl Biomater. 2009; 88:530–543. PMID: 18698626.

5. Bumgardner JD, Adatrow P, Haggard WO, Norowski PA. Emerging antibacterial biomaterial strategies for the prevention of peri-implant inflammatory diseases. Int J Oral Maxillofac Implants. 2011; 26:553–560. PMID: 21691602.
6. Assaf A, Daas M, Boittin A, Eid N, Postaire M. Prosthetic maintenance of different mandibular implant overdentures: A systematic review. J Prosthet Dent. 2017; 118:144–152.e5. PMID: 28385441.

7. Lindhe J, Meyle J. Group D of European workshop on periodontology. Peri-implant diseases: Consensus report of the sixth European workshop on periodontology. J Clin Periodontol. 2008; 35:282–285. PMID: 18724855.

8. Pontoriero R, Tonelli MP, Carnevale G, Mombelli A, Nyman SR, Lang NP. Experimentally induced peri-implant mucositis. A clinical study in humans. Clin Oral Implants Res. 1994; 5:254–259. PMID: 7640340.

9. Zitzmann NU, Berglundh T, Marinello CP, Lindhe J. Experimental peri-implant mucositis in man. J Clin Periodontol. 2001; 28:517–523. PMID: 11350518.

10. Salvi GE, Cosgarea R, Sculean A. Prevalence of periimplant diseases. Implant Dent. 2019; 28:100–102. PMID: 30762625.

11. Dreyer H, Grischke J, Tiede C, Eberhard J, Schweitzer A, Toikkanen SE, Glöckner S, Krause G, Stiesch M. Epidemiology and risk factors of peri-implantitis: A systematic review. J Periodontal Res. 2018; 53:657–681. PMID: 29882313.

12. Mayer E, Klapper HU, Nitschke I, Hahnel S. Observations, knowledge, and attitude towards treatment options in patients with dry mouth: a survey among German dentists. Clin Oral Investig. 2019; 23:4189–4194.

13. Morton D, Gallucci G, Lin WS, Pjetursson B, Polido W, Roehling S, Sailer I, Aghaloo T, Albera H, Bohner L, Braut V, Buser D, Chen S, Dawson A, Eckert S, Gahlert M, Hamilton A, Jaffin R, Jarry C, Karayazgan B, Laine J, Martin W, Rahman L, Schlegel A, Shiota M, Stilwell C, Vorster C, Zembic A, Zhou W. Group 2 ITI Consensus Report: Prosthodontics and implant dentistry. Clin Oral Implants Res. 2018; 29:215–223.
14. Al Dosari AAF, Habib SR, Alnassar T, Alshihri A, Kamalan R. The current considerations in the fabrication of implant prostheses and the state of prosthetic complications: A survey among the dental technicians. Saudi Dent J. 2018; 30:299–305. PMID: 30202166.

15. Harel N, Ormianer Z, Zecharia E, Meirowitz A. Consequences of experience and specialist training on the fabrication of implant-supported prostheses: A survey. J Prosthet Dent. 2017; 117:743–748. PMID: 27836146.

16. Jayachandran S, Bhandal BS, Hill KB, Walmsley AD. Maintaining dental implants-do general dental practitioners have the necessary knowledge? Br Dent J. 2015; 219:25–28. PMID: 26159981.
17. Junges R, Zitzmann NU, Walter C, Rösing CK. Dental care providers' decision making regarding maintenance of compromised teeth and implant therapy indication: an analysis of gender and enrollment in teaching positions. Clin Oral Implants Res. 2014; 25:1027–1033. PMID: 23786485.

18. Bishti S, Lautensack J, Türp JC, Wolfart S. Does professional experience save teeth? A survey among prosthodontists. Clin Oral Investig. 2018; 22:1001–1008.

19. Dragan IF, Pirc M, Rizea C, Yao J, Acharya A, Mattheos N. A global perspective on implant education: Cluster analysis of the “first dental implant experience” of dentists from 84 nationalities. Eur J Dent Educ. 2019; 23:251–265. PMID: 30710398.

20. Katsaros T, Allareddy V, Elangovan S. Dental students' exposure to periodontal and implant placement surgeries in U.S. dental schools. J Dent Educ. 2019; 83:953–958. PMID: 31085689.

21. Chin JS, Addy LD, Rees J, Locke M. Teaching of implant dentistry in dental hygiene and therapy schools in the UK and Ireland. Br Dent J. 2019; 226:692–696. PMID: 31076702.

22. Sanz M, Noguerol B, Sanz-Sanchez I, Hammerle CHF, Schliephake H, Renouard F, Sicilia A, Cordaro L, Jung R, Klinge B, Valentini P, Alcoforado G, Ornekol T, Pjetursson B, Sailer I, Rochietta I, Manuel Navarro J, Heitz-Mayfield L, Francisco H. Steering Committee. European association for osseointegration delphi study on the trends in implant dentistry in Europe for the year 2030. Clin Oral Implants Res. 2019; 30:476–486. PMID: 31033047.

23. Wismeijer D, Joda T, Flügge T, Fokas G, Tahmaseb A, Bechelli D, Bohner L, Bornstein M, Burgoyne A, Caram S, Carmichael R, Chen CY, Coucke W, Derksen W, Donos N, El Kholy K, Evans C, Fehmer V, Fickl S, Fragola G, Gimenez Gonzales B, Gholami H, Hashim D, Hui Y, Kökat A, Vazouras K, Kühl S, Lanis A, Leesungbok R, van der Meer J, Liu Z, Sato T, De Souza A, Scarfe WC, Tosta M, van Zyl P, Vach K, Vaughn V, Vucetic M, Wang P, Wen B, Wu V. Group 5 ITI Consensus Report: Digital technologies. Clin Oral Implants Res. 2018; 29:436–442. PMID: 30328201.

24. Pjetursson BE, Zarauz C, Strasding M, Sailer I, Zwahlen M, Zembic A. A systematic review of the influence of the implant-abutment connection on the clinical outcomes of ceramic and metal implant abutments supporting fixed implant reconstructions. Clin Oral Implants Res. 2018; 29:160–183. PMID: 30306682.

25. Elsayed A, Wille S, Al-Akhali M, Kern M. Comparison of fracture strength and failure mode of different ceramic implant abutments. J Prosthet Dent. 2017; 117:499–506. PMID: 27769518.

26. Pjetursson BE, Valente NA, Strasding M, Zwahlen M, Liu S, Sailer I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin Oral Implants Res. 2018; 29:199–214. PMID: 30328190.

27. Wittneben JG, Joda T, Weber HP, Brägger U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontol 2000. 2017; 73:141–151. PMID: 28000276.

28. Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions-a systematic review. Int J Oral Maxillofac Implants. 2014; 29:84–98. PMID: 24660192.

29. Korsch M, Robra BP, Walther W. Cement-associated signs of inflammation: retrospective analysis of the effect of excess cement on peri-implant tissue. Int J Prosthodont. 2015; 28:11–18. PMID: 25588166.

30. Korsch M, Obst U, Walther W. Cement-associated peri-implantitis: a retrospective clinical observational study of fixed implant-supported restorations using a methacrylate cement. Clin Oral Implants Res. 2014; 25:797–802. PMID: 23600620.

31. von Stein-Lausnitz M, Nickenig HJ, Wolfart S, Neumann K, von Stein-Lausnitz A, Spies BC, Beuer F. Survival rates and complication behaviour of tooth implant-supported, fixed dental prostheses: A systematic review and meta-analysis. J Dent. 2019; 88:103167. PMID: 31306691.

32. Schwarz F, Sanz-Martín I, Kern JS, Taylor T, Schaer A, Wolfart S, Sanz M. Loading protocols and implant supported restorations proposed for the rehabilitation of partially and fully edentulous jaws. Camlog Foundation Consensus Report. Clin Oral Implants Res. 2016; 27:988–992. PMID: 26748679.

33. Stoumpis C, Kohal RJ. To splint or not to splint oral implants in the implant-supported overdenture therapy? A systematic literature review. J Oral Rehabil. 2011; 38:857–869. PMID: 21480943.

34. Brandt S, Brandt J, Ketabi AR, Lauer HC, Kunzmann A. Locator® versus ceramic/electroplated double-crown attachments: a prospective study on the intraindividual comparison of implant-supported mandibular prostheses. Clin Oral Investig. 2019; 23:763–770.

35. Engelhardt F, Zeman F, Behr M, Hahmel S. Prosthetic complications and maintenance requirements in locator-attached implant-supported overdentures: A retrospective study. Eur J Prosthodont Restor Dent. 2016; 24:31–35. PMID: 27039476.
36. Hahnel S, Alamanos C, Schneider-Feyrer S, Stöckle M, Rosentritt M. Investigation of clinical and laboratory wear in locator-supported, implant-retained overdentures. Int J Prosthodont. 2018; 31:334–337. PMID: 29953562.

37. Heitz-Mayfield LJ, Aaboe M, Araujo M, Carrión JB, Cavalcanti R, Cionca N, Cochran D, Darby I, Funakoshi E, Gierthmuehlen PC, Hashim D, Jahangiri L, Kwon Y, Lambert F, Layton DM, Lorenzana ER, McKenna G, Mombelli A, Müller F, Roccuzzo M, Salvi GE, Schimmel M, Srinivasan M, Tomasi C, Yeo A. Group 4 ITI consensus report: Risks and biologic complications associated with implant dentistry. Clin Oral Implants Res. 2018; 29:351–358. PMID: 30328181.
38. Del Fabbro M, Nevins M, Venturoli D, Weinstein RL, Testori T. Clinically oriented patient maintenance protocol: A clinical consensus of experts. Int J Periodontics Restorative Dent. 2018; 38:281–288. PMID: 29447323.

Table 1
Survey of the abutments used by participating dentists in implant restorations in a single-tooth gap in the anterior upper jaw (regio 21) (no response: 29.4%)
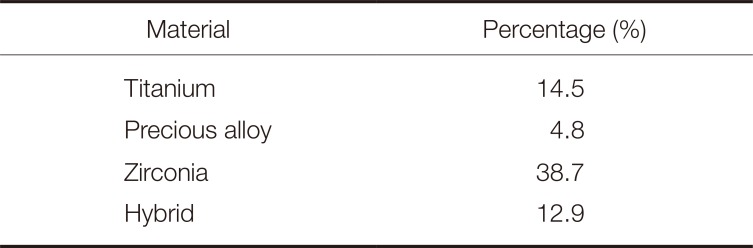
| Material | Percentage (%) |
|---|---|
| Titanium | 14.5 |
| Precious alloy | 4.8 |
| Zirconia | 38.7 |
| Hybrid | 12.9 |
Table 2
Survey of the type of crowns used by participating dentists in implant restorations in a single-tooth gap in the anterior upper jaw (regio 21) (no response: 9.7%)
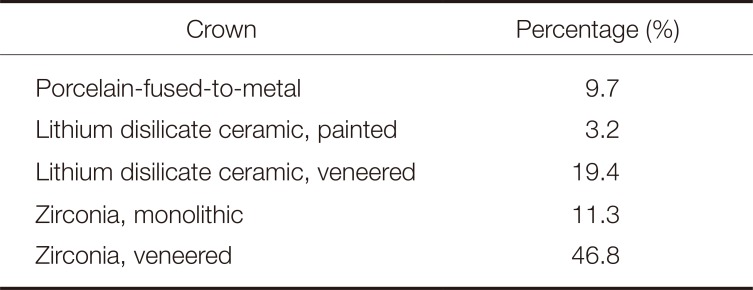
| Crown | Percentage (%) |
|---|---|
| Porcelain-fused-to-metal | 9.7 |
| Lithium disilicate ceramic, painted | 3.2 |
| Lithium disilicate ceramic, veneered | 19.4 |
| Zirconia, monolithic | 11.3 |
| Zirconia, veneered | 46.8 |
Table 3
Favored and non-favored treatment options in settings with a bilaterally shortened dental arch in the lower jaw (in %)




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download