1. Mecall RA, Rosenfeld AL. Influence of residual ridge resorption patterns on implant fixture placement and tooth position. 1. Int J Periodontics Restorative Dent. 1991; 11:8–23.

2. Drake RL, Vogl W, Mitchell AWM. Gray's anatomy for students. 2nd ed. Philadelphia (PA): Elsevier Health Sciences;2009.
3. Sarandha DL. Textbook of complete denture prosthodontics. 1st ed. New Delhi: Jaypee Brothers Medical Publishers;2008.
4. Glickman GN. Preparation for treatment. In : Cohen S, Burns RC, editors. Pathways of the pulp. St. Louis (MO): Mosby;2002. p. 77–109.
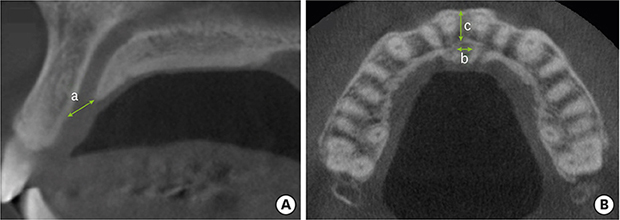
5. Mraiwa N, Jacobs R, Van Cleynenbreugel J, Sanderink G, Schutyser F, Suetens P, et al. The nasopalatine canal revisited using 2D and 3D CT imaging. Dentomaxillofac Radiol. 2004; 33:396–402.


6. Song WC, Jo DI, Lee JY, Kim JN, Hur MS, Hu KS, et al. Microanatomy of the incisive canal using three-dimensional reconstruction of microCT images: an
ex vivo study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:583–590.


7. Keith DA. Phenomenon of mucous retention in the incisive canal. J Oral Surg. 1979; 37:832–834.

8. Liang X, Jacobs R, Martens W, Hu Y, Adriaensens P, Quirynen M, et al. Macro- and micro-anatomical, histological and computed tomography scan characterization of the nasopalatine canal. J Clin Periodontol. 2009; 36:598–603.


9. Jacobs R, Lambrichts I, Liang X, Martens W, Mraiwa N, Adriaensens P, et al. Neurovascularization of the anterior jaw bones revisited using high-resolution magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:683–693.


10. Carlsson GE, Bergman B, Hedegård B. Changes in contour of the maxillary alveolar process under immediate dentures. A longitudinal clinical and X-ray cephalometric study covering 5 years. Acta Odontol Scand. 1967; 25:45–75.


11. Pietrokovski J. The bony residual ridge in man. J Prosthet Dent. 1975; 34:456–462.


12. Jahangiri L, Devlin H, Ting K, Nishimura I. Current perspectives in residual ridge remodeling and its clinical implications: a review. J Prosthet Dent. 1998; 80:224–237.

13. Asumi M, Yamaguchi T, Saito K, Kodama S, Miyazawa H, Matsui H, et al. Are serum cholesterol levels associated with silent brain infarcts? The Seiryo Clinic Study. Atherosclerosis. 2010; 210:674–677.


14. Filippi A, Pohl Y, Tekin U. Sensory disorders after separation of the nasopalatine nerve during removal of palatal displaced canines: prospective investigation. Br J Oral Maxillofac Surg. 1999; 37:134–136.


15. Edwards CB, Marshall SD, Qian F, Southard KA, Franciscus RG, Southard TE. Longitudinal study of facial skeletal growth completion in 3 dimensions. Am J Orthod Dentofacial Orthop. 2007; 132:762–768.


17. Hämmerle CH, Tarnow D. The etiology of hard- and soft-tissue deficiencies at dental implants: a narrative review. J Periodontol. 2018; 89 Suppl 1:S291–303.

18. Kraut RA, Boyden DK. Location of incisive canal in relation to central incisor implants. Implant Dent. 1998; 7:221–225.


19. Salemi F, Moghadam FA, Shakibai Z, Farhadian M. Three-dimensional assessment of the nasopalatine canal and the surrounding bone using cone-beam computed tomography. J Periodontol Implant Dent. 2015; 8:1–7.

20. Mardinger O, Namani-Sadan N, Chaushu G, Schwartz-Arad D. Morphologic changes of the nasopalatine canal related to dental implantation: a radiologic study in different degrees of absorbed maxillae. J Periodontol. 2008; 79:1659–1662.


21. Jia X, Hu W, Meng H. Relationship of central incisor implant placement to the ridge configuration anterior to the nasopalatine canal in dentate and partially edentulous individuals: a comparative study. PeerJ. 2015; 3:e1315.

22. Bornstein MM, Balsiger R, Sendi P, von Arx T. Morphology of the nasopalatine canal and dental implant surgery: a radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Implants Res. 2011; 22:295–301.


23. Fernández-Alonso A, Suárez-Quintanilla JA, Rapado-González O, Suárez-Cunqueiro MM. Morphometric differences of nasopalatine canal based on 3D classifications: descriptive analysis on CBCT. Surg Radiol Anat. 2015; 37:825–833.


24. Tözüm TF, Güncü GN, Yıldırım YD, Yılmaz HG, Galindo-Moreno P, Velasco-Torres M, et al. Evaluation of maxillary incisive canal characteristics related to dental implant treatment with computerized tomography: a clinical multicenter study. J Periodontol. 2012; 83:337–343.







 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download