Abstract
Background
Synovial chondromatosis occurs rarely in the shoulder, and its details remain unclear. The purpose of this study was to clarify the clinical results of surgical resection and the histopathological findings of synovial chondromatosis in the shoulder.
Methods
Ten shoulders with synovial chondromatosis that had been operatively resected were reviewed retrospectively. Osteochondral lesions were present in the glenohumeral joint in six shoulders and in the subacromial space in four shoulders. Two patients had a history of trauma with glenohumeral dislocation without recurrent instability, and the other seven patients (eight shoulders) did not have any traumatic episodes or past illness involving the ipsilateral shoulder girdle. The occurrences of osteochondral lesions, inferior humeral osteophytes, and acromial spurs were assessed on radiographs before resection, just after resection, and at final follow-up. The Constant scores were compared before resection and at final follow-up with Wilcoxon signed-rank tests. Resected lesions were histopathologically differentiated between primary and secondary synovial chondromatosis.
Results
Inferior humeral osteophytes were found in five shoulders with synovial chondromatosis in the glenohumeral joint, and all four shoulders with synovial chondromatosis in the subacromial space had acromial spur formation. Osteochondral lesions appeared to have been successfully removed in all shoulders on postoperative radiographs. At the final follow-up, however, one shoulder with secondary synovial chondromatosis in the subacromial space showed recurrence of osteochondral lesions and acromial spur formation. The mean Constant score improved significantly from 53.0 points before resection to 76.0 points at a mean follow-up of 6.0 years (p = 0.002). On histopathological evaluation, one shoulder was diagnosed as having primary synovial chondromatosis, while nine shoulders had secondary synovial chondromatosis.
Conclusions
The present study showed that resection of shoulder osteochondral lesions successfully relieved the clinical symptoms and that primary synovial chondromatosis is less common than secondary synovial chondromatosis in the shoulder. Although most of the present osteochondral lesions were clinically determined to be primary chondromatosis, only one case was histopathologically categorized as primary synovial chondromatosis. These results suggest that histopathological identification is needed to differentiate between primary and secondary synovial chondromatosis.
Synovial chondromatosis is a rare condition characterized by the presence of osteocartilaginous loose bodies in articular joints, bursae, or tendon sheaths.12) Milgram3) classified excised loose bodies in human joints into three categories: (1) loose bodies due to synovial osteochondromatosis; (2) loose bodies due to osteochondral fracture; and (3) loose bodies due to degenerative arthritis or avascular necrosis leading to fragmentation of the joint surface. Milgram3) also stated that the origins of the loose bodies can be differentiated by an analysis of the history, radiographs, and operative findings, but that histological analysis would be useful to classify particular cases. The terms synovial chondromatosis and synovial osteochondromatosis have been used for the same condition, but the term synovial osteochondromatosis has become less common because the lesions are not only unrelated to osteochondromas, but they are also not ossified.4)
Chondromatosis is a benign metaplastic chondroid proliferation that is distinct from the other causes in that it arises from primary chondrometaplasia of the synovium.56) On the basis of the histopathological characteristics, Villacin et al.7) grouped the cases with synovial chondrometaplasia or osteocartilaginous loose bodies into primary and secondary synovial chondromatosis. In primary synovial chondromatosis, the foci of chondrometaplasia in the synovium and the loose bodies are characterized by a markedly disorganized pattern with many binucleate, plump chondrocytes, and patchy diffuse calcification. On the other hand, secondary synovial chondromatosis has fragments of articular cartilage or subchondral lamellar bone in the loose bodies as a nidus, and the pattern of calcification is zonal and ring-like, with uniform, evenly distributed chondrocytes. Histopathological evaluation of loose bodies can help differentiate between primary and secondary chondromatosis in human joints.
Synovial chondromatosis most often affects the knee,2) while it occurs rarely in the shoulder girdle. Past case reports89101112131415161718192021) and case series6) have shown that synovial chondromatosis could occur both in the glenohumeral joint and in the subacromial space. Although some case reports112223) evaluated the resected osteochondral lesions histopathologically, no case series differentiated between primary and secondary synovial chondromatosis. Thus, differences of incidence, location of occurrence, clinical symptoms, radiographic findings, and results of surgical resection between primary and secondary chondromatosis occurring in the shoulder remain unclear.
The purpose of this study was to clarify the clinical results of surgical resection and the histopathological findings, as well as to review the past reports of synovial chondromatosis in the shoulder. Since chondromatosis cases without any history of shoulder trauma often have glenohumeral osteoarthritis6) or acromial spur formation,9) we hypothesized that primary synovial chondromatosis is less common than secondary synovial chondromatosis in the shoulder.
This study was approved by the Institutional Review Board of Keio University School of Medicine (IRB No. 20130147). Informed consent was waived. During the period between 1991 and 2012, 12 shoulders with pain due to multiple osteochondral loose bodies underwent surgery and were diagnosed with chondromatosis on the basis of histopathological evaluation after surgical resection. Two patients were lost to follow-up, and a total of 10 shoulders from nine patients (five men, four women), who could be followed for more than 2 years (mean ± standard deviation [SD], 6.0 ± 3.8 years; range, 2.3 to 12.3 years), were retrospectively reviewed. All patients complained of shoulder pain and an uncomfortable feeling during movement. Locking with a catching sensation of the shoulder occurred in two patients with lesions in the glenohumeral joint and two patients with lesions in the subacromial space. Since patients with recurrent glenohumeral instability24) and glenohumeral osteoarthritis25) often have loose bodies in the joint, cases with recurrent glenohumeral instability with more than one traumatic episode or severe glenohumeral osteoarthritis with greater than grade 2 on the Kellgren-Lawrence grading system on plain radiographs26) were excluded from this study even if they had loose bodies. At the time of surgery, the patients' average age was 40.7 ± 16.5 years (range, 12 to 65 years). Two patients had a history of trauma with glenohumeral dislocation 15 years (case 2) and 40 years (case 5) earlier, but they did not have recurrent instability. The other eight shoulders did not have any traumatic episodes or past illness involving the ipsilateral shoulder girdle. The average duration of symptoms was 63 ± 77 months (range, 1 to 180 months), and the average visual analog scale pain score graded from 0 (no pain) to 100 mm (maximal pain) was 54.3 ± 11.5 mm (range, 30 to 68 mm) (Table 1).
Osteochondral lesions were found in all cases on the anteroposterior view and the scapular Y view of plain radiographs with the shoulder in neutral rotation. In addition, the localization of osteochondral lesions was identified in three shoulders with computed tomography scans, in one shoulder with magnetic resonance imaging, and in six shoulders with both imaging modalities. Four shoulders had osteochondral lesions in the subacromial space (40%), and six shoulders had them in the glenohumeral joint (60%) (Table 1).
The osteochondral lesions were resected with synovectomy. Open resection was performed in the first eight shoulders (five shoulders with lesions in the glenohumeral joint and three shoulders with lesions in the subacromial space), and arthroscopic surgery was performed in the latter two shoulders (one shoulder with lesions in the glenohumeral joint and one shoulder with lesions in the subacromial space). All operations were performed with the patients in the beach chair position, and an image intensifier was not used. During open resection, the anterior approach between the pectoralis major and deltoid for glenohumeral osteochondral lesions and the lateral approach between the anterior and middle portions of the deltoid muscle for subacromial lesions were used. Osteochondral lesions in the glenohumeral joint were resected through tenotomy of the superior half of the subscapularis tendon. Most cases had multiple lesions in the bicipital groove, and they were evaluated and removed through the glenohumeral joint. After removal of the lesions, the subscapularis tendon was repaired. In cases with osteochondral lesions in the subacromial space, resection of acromial spurs and acromioplasty were performed with partial detachment of the anterior deltoid, and the osteochondral lesions were removed. Two shoulders with subacromial lesions had a small bursal side tear of the supraspinatus tendon, and it was repaired using transosseous technique. During arthroscopic resection, lesions in the glenohumeral joint and in the bicipital groove were removed from the anterior portal through the rotator interval using a posterior viewing portal, and removal of subacromial lesions with subacromial decompression was performed from the lateral portal using a posterior viewing portal. No other surgical treatment, including biceps tenotomy, biceps tenodesis, manipulation of the joint, and rotator interval closure, was performed.
In this study, the differential diagnosis between primary and secondary synovial chondromatosis was made histologically on the basis of the criteria proposed by Villacin et al.7) All patients had been clinically assessed at initial presentation, and histopathological evaluation was performed. Shoulder range of motion (ROM) in forward elevation, external rotation at the side, and internal rotation was evaluated. Internal rotation was measured by the most cephalad vertebral spinous process that could be reached with the extended thumb. Constant scores were scored before resection and at final follow-up for operated shoulders. The occurrences of osteochondral lesions, inferior humeral osteophytes, and acromial spurs were assessed by radiographs before resection, just after resection, and at final follow-up.
Statistical analysis was carried out using IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). ROM in shoulder elevation and external rotation and the Constant score were compared before resection and at final follow-up with Wilcoxon signed-rank tests using a significance level of 0.05.
On histopathological examination, one osteochondral lesion in the glenohumeral joint of a 48-year woman proved to be primary synovial chondromatosis, with numerous osteochondral lesions (more than 20). The osteochondral lesions showed a markedly disorganized pattern with cloning of the cartilage cells (Fig. 1). In the other nine cases, the metaplastic cartilaginous nodules were cellular, and the chondrocytes were uniform in appearance (Fig. 2). Thus, these cases were diagnosed as secondary synovial chondromatosis. Four cases with secondary chondromatosis occurred in the subacromial space, whereas five cases had lesions in the glenohumeral joint. In cases with secondary synovial chondromatosis, three cases with numerous (> 20) osteochondral lesions were present in three shoulders, between 10 and 20 lesions were found in four shoulders, and a small number of lesions was found in two shoulders (the number of osteochondral lesions was five and eight) (Table 1).
Before resection of osteochondral lesions, the patients' average ROM was elevation of 130° ± 25°, external rotation of 32° ± 22°, and internal rotation to the spinous process of the 12th thoracic vertebra. Shoulder ROM at final follow-up improved in elevation (140° ± 24°; p = 0.688) and external rotation (37° ± 23°; p = 0.156), but the differences were not significant. Mean internal rotation at final follow-up was to the spinous process of the 8th thoracic vertebra. The mean preoperative Constant score was 53.0 ± 9.4 points (range, 41 to 65 points). At final follow-up, the mean Constant score was significantly improved to 76.0 ± 12.2 points (range, 60 to 96 points; p = 0.002) (Table 1). The values of the individual parameters of the Constant score (pain, activity, mobility, and strength) were higher after surgery than before surgery: pain, from 5.5 to 11.5; activity, from 2.2 to 5.8; mobility, from 27.8 to 32.4; and strength, from 10.1 to 17.7.
Preoperative imaging showed four shoulders with osteochondral lesions in the subacromial space and six shoulders with osteochondral lesions in the glenohumeral joint. Inferior humeral osteophytes were found in five shoulders (83%) with synovial chondromatosis in the glenohumeral joint. According to the Samilson and Prieto classification, two shoulders (33%) were grade 2, and three shoulders (50%) were grade 3. Grade 3 cases showed large osteophytes greater than 7 mm, but the glenohumeral joint space was maintained in these cases. All four shoulders (100%) with synovial chondromatosis in the subacromial space had acromial spur formation (Table 2).
On postoperative radiographs, osteochondral lesions were successfully removed in all shoulders. At the final follow-up, however, one case of subacromial chondromatosis showed recurrence of new loose bodies at 12.3-year follow-up. In this patient, the resected acromial spur also recurred. There was no evidence of recurrence in the other nine shoulders (Table 1). Inferior humeral osteophytes did not progress in all patients with synovial chondromatosis in the glenohumeral joint. The acromial spur recurred in one shoulder with recurrence even with acromioplasty, but the other nine shoulders did not show progression of spur formation over the follow-up period.
Synovial chondromatosis occurs rarely in the shoulder, and its characteristics remain unclear. This study showed that removal of shoulder osteochondral lesions successfully relieved the clinical symptoms with a relatively low recurrence rate, and the histopathological findings suggest that primary synovial chondromatosis is less common than secondary synovial chondromatosis in the shoulder.
In the present cases, patients with both glenohumeral and subacromial chondromatosis showed similar clinical symptoms of shoulder pain, an uncomfortable feeling during shoulder motion, and locking with a catching sensation,891011272829) and resection of osteochondral lesions successfully relieved the clinical symptoms, both in the glenohumeral and subacromial cases and both in primary and secondary synovial chondromatosis cases. On radiography in the present study, an inferior humeral osteophyte was present in the majority of cases with glenohumeral synovial chondromatosis in the glenohumeral joint, and all four shoulders with synovial chondromatosis in the subacromial space had acromial spur formation. The present results suggest that glenohumeral synovial chondromatosis might be related to glenohumeral arthritis,6) and subacromial synovial chondromatosis might be related to acromial spur formation.
Some cases with secondary synovial chondromatosis were reported to have no definitive traumatic episode or radiographic and arthroscopic evidence of joint disease.112223) In the present cases, two patients had a preceding episode of single glenohumeral dislocation, while the other eight patients did not have any past illness in the shoulder girdle. Although most of the present osteochondral lesions were clinically determined to be primary chondromatosis, only one case was histopathologically categorized as primary synovial chondromatosis. The present results suggest that histopathological identification is needed to differentiate between primary and secondary synovial chondromatosis.
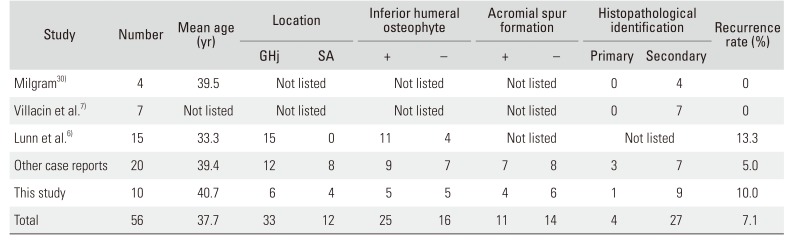
On review of past reported cases67811121314151617181920212223273031) and the present cases with synovial chondromatosis occurring in the shoulder, four shoulders were recognized as having primary synovial chondromatosis, 27 had secondary synovial chondromatosis, and the remaining 25 were not differentiated between primary and secondary synovial chondromatosis on histopathological examination (Table 3). Primary synovial chondromatosis is thought to be less common than secondary synovial chondromatosis in the shoulder. Malignant transformation to chondrosarcoma occasionally occurs in primary synovial chondromatosis.3233) Primary synovial chondromatosis is aggressive and is associated with a high incidence of recurrence, while secondary synovial chondromatosis is nonaggressive.7) Although it is still unclear how important it is to know whether the lesions are primary or secondary and further investigation will be needed, histopathological differentiation might help predict a patient's prognosis.
The present study had several limitations. The first limitation was the small number of cases with various follow-up periods. Since chondromatosis is a rare condition in the shoulder, this retrospective study included surgically resected cases with a minimum 2-year follow-up period. Unfortunately, this study could not show the clinical differences between primary and secondary synovial chondromatosis because only one case of primary synovial chondromatosis was included among the present cases. Furthermore, the period of 2 years would be too short to clarify the recurrence rate of the tumor-like lesion or morphological alterations of arthritic changes. Thus, further investigation is needed to determine the long-term prognosis in patients with synovial chondromatosis in the shoulder. Although histopathological examination was carefully carried out in the present cases, the second limitation was the possibility of misdiagnosis. In cases with numerous osteochondral lesions, at least 10 lesions were evaluated histopathologically to differentiate primary and secondary synovial chondromatosis, and histopathological diagnoses were consistently made. However, all of the loose bodies could not be evaluated in cases with numerous osteochondral lesions, and the existence of unchecked lesions might be a possible limitation of this study.
References
1. Jaffe HL. Synovial chondromatosis and other benign articular tumors. In : Jaffe HL, editor. Tumors and tumorous conditions of the bones and joints. Philadelphia, PA: Lea & Febiger;1958. p. 558–567.
2. Mussey RD Jr, Henderson MS. Osteochondromatosis. J Bone Joint Surg Am. 1949; 31A(3):619–627. PMID: 18153904.

3. Milgram JW. The classification of loose bodies in human joints. Clin Orthop Relat Res. 1977; (124):282–291.

4. Ho YY, Choueka J. Synovial chondromatosis of the upper extremity. J Hand Surg Am. 2013; 38(4):804–810. PMID: 23474166.

5. Apte SS, Athanasou NA. An immunohistological study of cartilage and synovium in primary synovial chondromatosis. J Pathol. 1992; 166(3):277–281. PMID: 1381426.

6. Lunn JV, Castellanos-Rosas J, Walch G. Arthroscopic synovectomy, removal of loose bodies and selective biceps tenodesis for synovial chondromatosis of the shoulder. J Bone Joint Surg Br. 2007; 89(10):1329–1335. PMID: 17957072.

7. Villacin AB, Brigham LN, Bullough PG. Primary and secondary synovial chondrometaplasia: histopathologic and clinicoradiologic differences. Hum Pathol. 1979; 10(4):439–451. PMID: 468226.
8. Xu C, Yang X, Zhao J. Arthroscopic treatment for synovial chondromatosis of the subacromial bursa associated with partial rotator cuff tear. Knee Surg Sports Traumatol Arthrosc. 2015; 23(2):600–602. PMID: 25217318.

9. Ogawa K, Takahashi M, Inokuchi W. Bilateral osteochondromatosis of the subacromial bursae with incomplete rotator cuff tears. J Shoulder Elbow Surg. 1999; 8(1):78–81. PMID: 10077803.

10. Jeon IH, Ihn JC, Kyung HS. Recurrence of synovial chondromatosis of the glenohumeral joint after arthroscopic treatment. Arthroscopy. 2004; 20(5):524–527. PMID: 15122144.

11. Hamada J, Tamai K, Koguchi Y, Ono W, Saotome K. Case report: a rare condition of secondary synovial osteochondromatosis of the shoulder joint in a young female patient. J Shoulder Elbow Surg. 2005; 14(6):653–656. PMID: 16337537.

12. De Ferm A, Lagae K, Bunker T. Synovial osteochondromatosis: an unusual cause for subacromial impingement. Acta Orthop Belg. 1997; 63(3):218–220. PMID: 9415731.
13. Volpin G, Nerubay J, Oliver S, Katznelson A. Synovial osteochondromatosis of the shoulder joint. Am Surg. 1980; 46(7):422–424. PMID: 7447180.
14. Carpintero P, Luque A, Serrano J. Recurrent osteochondromatosis of the shoulder in a child. Orthopedics. 1998; 21(3):361–362. PMID: 9547821.

15. Kawasaki T, Imanaka T, Matsusue Y. Synovial osteochondromatosis in bilateral subacromial bursae. Mod Rheumatol. 2003; 13(4):367–370. PMID: 24387262.

16. Brodsky AE. Synovial osteochondromatosis of the shoulder. Bull Hosp Joint Dis. 1950; 11(1):14–25. PMID: 14783699.
17. Devgan A, Gupta V, Magu NK, Rohilla R. Primary combined intra-articular and extra-articular synovial osteochondromatosis of shoulder: a case report. Chin Med Sci J. 2014; 29(4):248–250. PMID: 25429753.

18. Milgram JW, Hadesman WM. Synovial osteochondromatosis in the subacromial bursa. Clin Orthop Relat Res. 1988; (236):154–159.

19. Butt SH, Muthukumar T, Cassar-Pullicino VN, Mangham DC. Primary synovial osteochondromatosis presenting as constrictive capsulitis. Skeletal Radiol. 2005; 34(11):707–713. PMID: 16132979.

20. Jones GC, Riley GP, Buttle DJ. The role of proteases in pathologies of the synovial joint. Int J Biochem Cell Biol. 2008; 40(6-7):1199–1218. PMID: 18339575.

21. Ranalletta M, Bongiovanni S, Calvo JM, Gallucci G, Maignon G. Arthroscopic treatment of synovial chondromatosis of the shoulder: report of three patients. J Shoulder Elbow Surg. 2009; 18(3):e4–e8.

22. Horii M, Tamai M, Kido K, Kusuzaki K, Kubo T, Hirasawa Y. Two cases of synovial chondromatosis of the subacromial bursa. J Shoulder Elbow Surg. 2001; 10(2):186–189. PMID: 11307084.

23. Ji JH, Shafi M, Jeong DS. Secondary synovial chondromatosis of the shoulder. Knee Surg Sports Traumatol Arthrosc. 2015; 23(9):2624–2627. PMID: 24803015.

24. Seltzer SE, Weissman BN. CT findings in normal and dislocating shoulders. J Can Assoc Radiol. 1985; 36(1):41–46. PMID: 3980551.
25. Weinstein DM, Bucchieri JS, Pollock RG, Flatow EL, Bigliani LU. Arthroscopic debridement of the shoulder for osteoarthritis. Arthroscopy. 2000; 16(5):471–476. PMID: 10882441.

26. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957; 16(4):494–502. PMID: 13498604.

27. Yucel B, Mutlu S, Komur B, Mutlu H. Arthroscopic removal of giant loose bodies in the glenohumeral joint. Int J Surg Case Rep. 2014; 5(8):459–461. PMID: 24973527.

28. Huang TF, Wu JJ, Chen TS. Bilateral shoulder bursal osteochondromatosis associated with complete rotator cuff tear. J Shoulder Elbow Surg. 2004; 13(1):108–111. PMID: 14735086.

29. Katoh H, Ogawa K, Ikegami H, Inokuchi W, Toyama Y. Osteochondromatosis of the shoulder in a twelve-year-old boy. J Shoulder Elbow Surg. 2007; 16(1):e15–e19.

30. Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am. 1977; 59(6):792–801. PMID: 908703.
31. Chillemi C, Marinelli M, de Cupis V. Primary synovial chondromatosis of the shoulder: clinical, arthroscopic and histopathological aspects. Knee Surg Sports Traumatol Arthrosc. 2005; 13(6):483–488. PMID: 15726326.

32. Sah AP, Geller DS, Mankin HJ, et al. Malignant transformation of synovial chondromatosis of the shoulder to chondrosarcoma: a case report. J Bone Joint Surg Am. 2007; 89(6):1321–1328. PMID: 17545437.
33. Ng VY, Louie P, Punt S, Conrad EU. Malignant transformation of synovial chondromatosis: a systematic review. Open Orthop J. 2017; 11:517–524. PMID: 28694891.

Fig. 1
(A) Preoperative anteroposterior radiograph: a 48-year-old man with primary synovial chondromatosis in the glenohumeral joint (case 8). (B) Histological image of the osteochondral lesion showing cellular metaplastic cartilage nodules in primary synovital chondromatosis (× 100).
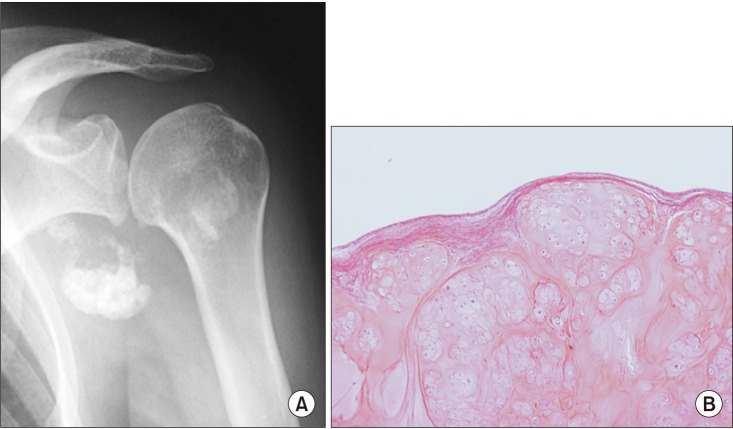
Fig. 2
(A) Preoperative anteroposterior radiograph: a 65-year-old woman with secondary synovial chondromatosis in the subacromial space (case 10). (B) Histological image of the osteochondral lesion showing the ring-like pattern of calcification in secondary synovial chondromatosis (× 40).
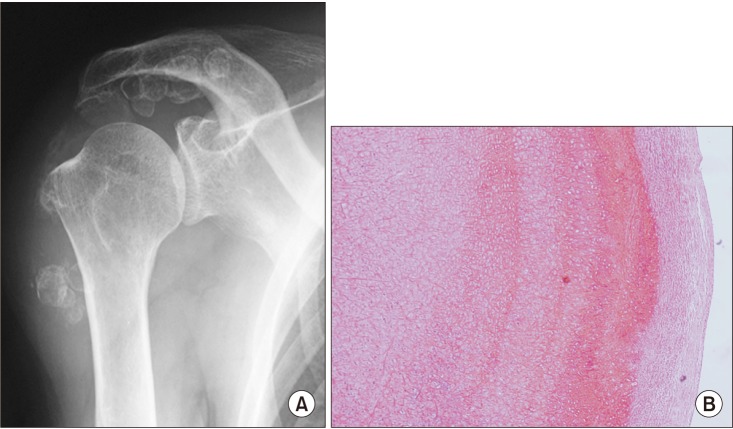
Table 1
Clinical and Histopathological Details of the Patients with Synovial Chondromatosis
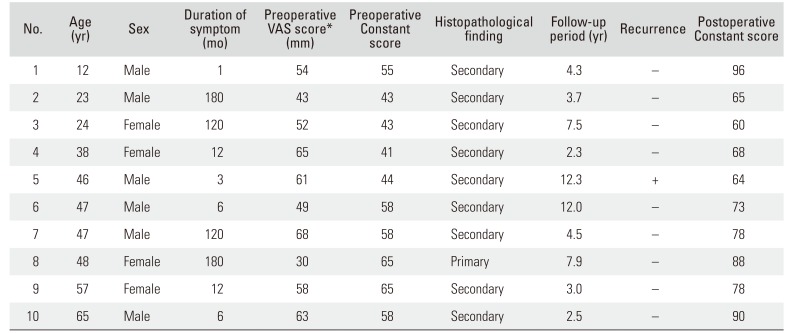
Table 2
Radiographic and Intraoperative Details of the Patients with Synovial Chondromatosis
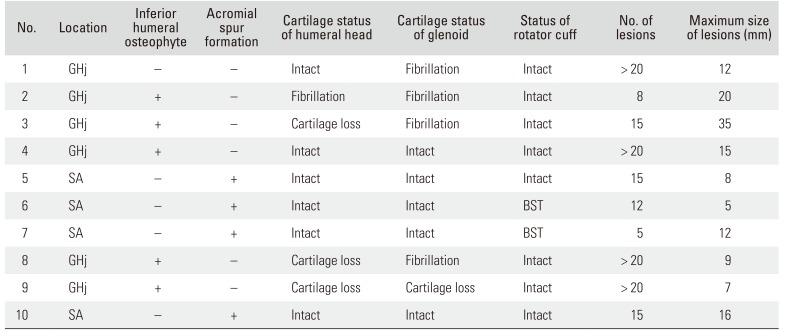
Table 3
Reported Cases of Synovial Chondromatosis in the Shoulder
| Study | Number | Mean age (yr) | Location | Inferior humeral osteophyte | Acromial spur formation | Histopathological identification | Recurrence rate (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| GHj | SA | + | − | + | − | Primary | Secondary | ||||
| Milgram30) | 4 | 39.5 | Not listed | Not listed | Not listed | 0 | 4 | 0 | |||
| Villacin et al.7) | 7 | Not listed | Not listed | Not listed | Not listed | 0 | 7 | 0 | |||
| Lunn et al.6) | 15 | 33.3 | 15 | 0 | 11 | 4 | Not listed | Not listed | 13.3 | ||
| Other case reports | 20 | 39.4 | 12 | 8 | 9 | 7 | 7 | 8 | 3 | 7 | 5.0 |
| This study | 10 | 40.7 | 6 | 4 | 5 | 5 | 4 | 6 | 1 | 9 | 10.0 |
| Total | 56 | 37.7 | 33 | 12 | 25 | 16 | 11 | 14 | 4 | 27 | 7.1 |




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download