Abstract
Background
Intramedullary (IM) nailing is widely performed in elderly patients with trochanteric fractures. Thus, it is important to identify causative factors associated with fixation failure. We investigated fixation failures after IM nailing in elderly patients with trochanteric fractures and compared the failure group with nonfailure group to identify risk factors of fixation failure.
Methods
A total of 396 patients aged 65 years or older underwent IM nailing for trochanteric fractures between January 2012 and August 2016 at our institution. Of those, 194 patients who were followed up for more than 12 months were enrolled in this study; 202 patients were excluded due to death during follow-up, bedridden status before injury, and loss to follow-up. All patients underwent plain radiography and preoperative computed tomography (CT).
Results
Fixation failure occurred in 11 patients (5.7%). Seven patients had stable fractures (AO/OTA); eight patients had basicervical fractures (confirmed by CT). Five patients had comminution in the greater trochanter (confirmed by CT). Regarding fracture reduction, eight patients showed discontinuity in the anterior cortex. The position of the lag screw on the lateral view was in the center in six patients and in a posterior area in the other five patients. On the basis of comparison with the 183 patients without fixation failure, risk factors of fixation failure were higher body mass index (BMI; p = 0.003), basicervical type of fracture (p = 0.037), posterior placement of the lag screw on the lateral view (p < 0.001), and inaccurate reduction of the anterior cortex (p = 0.011).
Conclusions
Among the risk factors of fixation failure after IM nailing in elderly patients with trochanteric fractures, discontinuity of the anterior cortex and posterior position of the lag screw are modifiable surgeon factors, whereas higher BMI and basicervical type of fracture are nonmodifiable patient factors. Therefore, care should be taken to avoid fixation failure in IM nailing for patients with a basicervical type of fracture or higher BMI or both.
The incidence of trochanteric fractures increases as the society ages. A trochanteric fracture is mostly caused by low-energy trauma in elderly patients with low bone mineral density (BMD), and morbidity and mortality rates after this fracture are high.1) The goals of surgical treatment of a trochanteric fracture are to anatomically reduce and firmly stabilize the fracture to restore preinjury functions as soon as possible and to minimize medical and surgical complications.12) Because intramedullary (IM) nails have biomechanical and minimally invasive advantages over sliding hip screws, IM nailing is widely performed for trochanteric fractures. One of the critical complications after surgical treatment of a trochanteric fracture is fixation failure, the incidence of which has been reported as high as 20% especially in unstable fractures. Fixation failure mostly requires reoperation or conversion to arthroplasty. However, for fragile elderly patients, additional surgery itself can be risky and considerably increase the risk of postoperative morbidity and mortality. Therefore, it is important to identify risk factors of fixation failure for prevention. Risk factors of failure after fixation with side plates, such as dynamic hip screws, are well known, but those after IM nailing have not been extensively investigated. Since three-dimensional computed tomography (3D-CT) is effective for assessing fracture stability, we investigated the risk factors of fixation failure after IM nailing in the treatment of trochanteric fractures in the elderly patients by using 3D-CT.
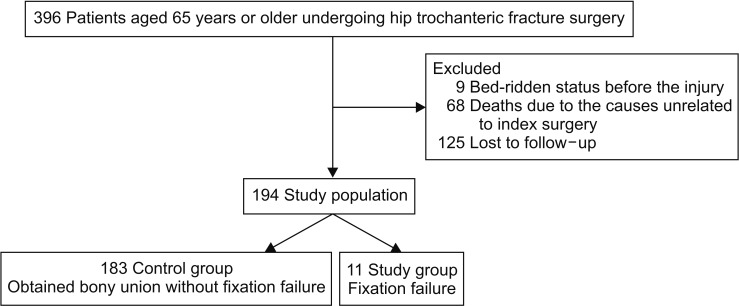
We conducted this study in compliance with the principles of the Declaration of Helsinki. This study was approved by the local Institutional Review Board (IRB No. HUGSSH IRB 2017-07-061-007) and informed consent was obtained from all patients before surgery. We retrospectively reviewed medical records of 396 patients who were aged 65 years or older and underwent IM nailing for a trochanteric fracture between January 2012 and August 2016 at one of the three insitutions. To reduce selection bias caused by including patients with fractures in high-energy injuries, we excluded patients younger than 65 years. Sixty-eight patients died during follow-up for reasons not directly related to the index surgery, nine had been in bedridden status perioperatively, and 125 were lost to follow-up. Patients without imaging follow-up at clinical visits were excluded. Phone interviews were not conducted. Finally, excluding these 202 patients, we included 194 patients who were followed up for more than 12 months in the study. Of the 194 patients, 183 obtained bony union without fixation failure, whereas 11 had fixation failure during follow-up (Fig. 1). The mean age of patients at the index surgery was 79 years (range, 65 to 99 years), and 152 patients were women and 42 were men. The fracture side was right in 72 patients and left in 122 patients. To identify potential risk factors, we investigated the followings: (1) patient factors including patients' age, sex, fracture side, body mass index (BMI), BMD, fracture type and stability according to AO/OTA classification, the presence of comminution of the greater trochanter on CT, and the basicervical type of fracture (confirmed by CT). In this study, we defined basicervical type of fracture as a fracture with the main fracture line presenting between the neck base and the upper margin of the lesser trochanter medially and between the neck base and 1 cm lateral to the tip of the greater trochanter laterally on 3D-CT.345) This fracture type may correspond to A1.1, A1.2, and some of A1.3 fractures and A2.1 and A2.2 fractures on AO/OTA classification (Fig. 2). (2) Surgeon factors including the type of lag screw (thread or blade), quality of reduction (continuity of the anterior and medial cortices), position of a lag screw within the femoral head, tip-apex distance (TAD), and sliding distance of lag screw. In all patients, 3D-CT was performed preoperatively to identify the fracture type, especially basicervical type, and the presence of greater trochanter comminution. For the analysis of fracture type on 3D-CT, three orthopedic surgeons performed measurements three times each with a 4-week interval to minimize interobserver errors. Regarding the implant, a nail with a thread-type lag screw was used in 140 patients (ITST, trochanteric/subtrochanteric fixation system, Zimmer, Warsaw, IN, USA or Gamma 3 nail, Stryker, Schonkirchen, Germany), whereas the helical blade-type nail was used in 54 patients (Proximal Femoral Nail Anti-rotation; AO Synthes, Davos, Switzerland). Fixation failure was defined as conditions requiring reoperation due to implant-related complications.
For comparison of failure group and nonfailure group, because the number of patients in the failure group is small, Shapiro-Wilk normality test was used to determine the normality of the data set. Independent t-test or Mann-Whitney U-test was performed by IBM SPSS ver. 25.0 (IBM Corp., Armonk, NY, USA). Statistical significance was determined as p < 0.05.
The patient was asked to assume a supine position on the fracture bed and received general or spinal anesthesia. After fixation in the fracture bed, manual reduction was performed through traction and internal rotation or adduction or both. Results of reduction were confirmed via fluoroscopy. If manual reduction was unsatisfactory, a long Kelly or Hohmann retractor was used to compress the lateral cortex or the anterior cortex for reduction. Invasive open reduction was not performed. The purpose of manual reduction was to maintain the continuity of the medial and anterior cortices. After manual reduction, an entry point was determined, and a guide pin was inserted. Proximal reaming was performed in the proximal area using a conical reamer thicker than the nail. If a fracture gap was still present, we used a compression technique on each implant for reduction. The distal fixation screw was fixed in a static locking mode regardless of the fracture type in all patients according to the surgeon's preference. Approximately 2 to 3 days postoperatively, when the patient could tolerate weight-bearing in a sitting position, the patient was asked to try to stand by using a tilt table. Weight-bearing walking was allowed as tolerated. Timing and amount of weight-bearing were dependent on the patient's medical condition, not on the fracture stability or bone quality. Follow-up X-ray was routinely performed on the 7th postoperative day or before discharge.
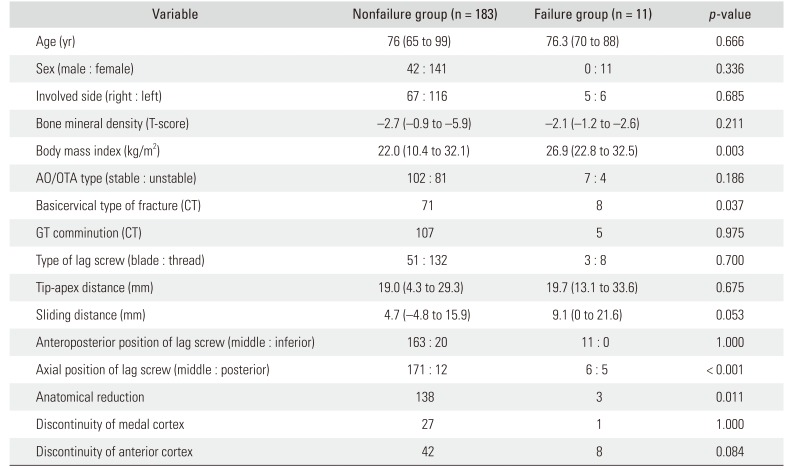
Fixation failure occurred in 11 patients (5.7%). The comparative data were statistically analyzed between the fixation failure group and nonfailure group (Table 1). In the failure group, cut-out of the thread-type lag screw occurred in eight patients (Fig. 3); cut-through of the helical blade, in two (Fig. 4); and nail breakage, in one. According to AO/OTA classification, five failures occurred in A1; five, in A2; and one, in A3. In other words, seven were stable fractures and four were unstable. There is no significant difference in AO/OTA classification between the failure group and nonfailure group (p = 0.186). On BMD, the mean T-score was −2.7 (range, −0.9 to −5.9) in the nonfailure group and −2.1 (range, −1.2 to −2.6) in the failure group (p = 0.211). Five patients had concomitant comminution of the greater trochanter (p = 0.975). In the failure group, the mean TAD was 19.7 mm (range, 13.1 to 33.6; p = 0.675), and the mean sliding distance was 9.1 mm (range, 0 to 21.6 mm; p = 0.053). In all patients, the lag screw was placed in the center of the femoral head on the anteroposterior view. However, on the lateral view, it was in the center of the femoral head in six patients and in posterior to the head center in the other five patients. On fracture reduction, one of the 11 patients showed discontinuity of the medial cortex, but eight patients showed discontinuity of the anterior cortex, thus not achieving anatomical reduction. On the basis of the comparative analysis between the failure and nonfailure groups, the following variables were identified as the risk factors of fixation failure: higher BMI (p = 0.003), basicervical type of fracture (p = 0.037), the position of the lag screw in the posterior to the head center on the lateral view (p < 0.001), and inaccurate, nonanatomical reduction, especially of the anterior cortex (p = 0.011) (Table 1).
For treatment of trochanteric fractures, IM nailing has advantages over the use of sliding hip screws with respect to the operation time, amount of blood loss during surgery, shortening of the lower limb due to malunion, and duration of hospital stay, as well as the biomechanical benefits. Thus, recently, IM nailing has become most commonly used to treat trochanteric fractures.6789) With use of the sliding hip screw, which was most frequently used in the past, fixation failure occurs in approximately 5% to 20% and reoperation may be unavoidable due to pain, loss of ability to walk, and shortening and malrotation of the leg. In addition, fatigue fracture has been reported more often in association with the plate system in comparison to the nail system. Even with the nail system, the incidence of loss of fixation requiring reoperation ranges from 2.5% to 19.1%. Hence, many authors are currently investigating to reduce fixation failure and the need for reoperation.2671011)
Factors that affect osteosynthesis and treatment outcome can be largely categorized into the patient factors including epidemiologic factors and the surgeon factors. Patient factors include epidemiologic factors, fracture side (right or left), patient's age, sex, BMI, the classification of type and stability of fracture, bone quality (characterized by osteoporosis or osteopenia), underlying disease or condition that affects bone quality (rheumatoid arthritis and chronic renal failure), long-term alcohol addiction, and use of steroid. Of these, the most important factor is fracture stability, that is, the type and classification of fracture. However, such patient factors cannot be modified by the surgeon; therefore, more attention should be paid to the surgeon factors. Surgeon factors include the implant choice, reduction quality, and the position of the lag screw, of which reduction quality is the most important factor. Manual closed reduction can be relatively well achieved, and detailed descriptions of reduction techniques using an instrument (Kelly clamp, Hohmann retractor, wire passer, or Schanz screw) are available. These techniques can be performed through a small opening.1112) Extensive research has been performed on the appropriate position of the lag screw in the femoral head because it is considered one of the most important surgeon factors.131415) Risk factors of fixation failure have been well known, and recognition of these factors has helped to decrease the incidence of fixation failure and the need for reoperation. However, fixation failure cannot be completely prevented because of the existence of nonsurgical factors. Especially in the aging society, it is believed that the rate of fixation failure will not decrease in spite of the superiority of the lag screws, improvement of reduction techniques, and proper positioning of the implant because osteoporosis is prevalent and the incidence of unstable fractures increases in the elderly population. In our study, fixation failure occurred in 11 patients comprising 5.7% of the sample. Nonmodifiable patient factors associated with fixation failure was higher BMI (p = 0.003) and basicervical fracture (p = 0.037), and the modifiable surgeon factors of failure were posterior position of the lag screw in the femoral head on a lateral view (p < 0.01) and inaccurate reduction of the anterior cortex (p = 0.011). Of the surgeon factors, inadequate anatomical reduction of both cortices is considered the critical factor of fixation failure. Medial cortex reduction can be obtained by fracture table traction or the instrument buttress technique. If the medial cortex is not properly reduced, valgus reduction is more effective than non-valgus reduction.16) Although fracture reduction of the anterior cortex is done on a fracture table with instrumentation through the mini-open approach, the quality of reduction of the anterior cortex is poorer than that of the medial cortex. This is because when the surgeon pushes the anterior cortex with an instrument, the proximal fragment can protrude posteriorly and the rotational malalignment of the proximal fragment can obstruct accurate reduction.17) Chun et al.18) reported good reduction of anterior cortex by the percutaneous technique in sagittaly unstable trochanteric fractures.
The main finding of our study is that BMI has greater influence on clinical outcomes than BMD does. This finding suggests that IM nailing provides mechanical stability even in patients with osteoporosis. Accurate closed reduction with proper positioning of lag screws can be interfered in high BMI patients because the proper placement of the entry point and closed reduction can be more difficult in them than in low BMI patients. In five of the 11 patients in the failure group, the lag screws were posteriorly positioned, but the posterior positioning can be considered acceptable unless it is very eccentric.15) The fracture type also had a considerable influence on the outcome. We thought that the stability classification system of trochanteric fractures that was established in the past in association with sliding hip screw would be inadequate for classification of fractures treated by the nail system. And we performed preoperative 3D-CT in all patients with fractures and determined fracture types. We hypothesized that a fixation failure should be separately analyzed for different fracture types. Among the stable fractures, the basicervical type fracture is a partial capsular fracture, a variation of trochanteric fracture and can be considered stable from the perspective of femoral neck fractures but unstable from the perspective of trochanteric fractures. A good example would be basicervical type fracture with varus deformity, which shows significant shortening and varus angulation. We believe that such gray-zone fracture should be considered differently from the typical neck fracture or trochanteric fracture. In our study, most patients with fixation failure had a basicervical type fracture, and statistically significant difference was found between the failure and the nonfailure groups. This finding suggests the need for a new classification system for trochanteric fractures treated with the nail system. In patients with a basicervical fracture or an acute varus deformity fracture among the A1, to avoid the toggling effect due to eccentric positioning of the lag screw, the screw should be centered on the anteroposterior and lateral views. That is, in the past, a fixation failure was thought to occur only in unstable fractures on the basis of the results of surgery using sliding hip screws, but our findings strongly suggest that a different conclusion might be made with use of the IM nails, which are biomechanically more stable. In addition, all A3 fractures and trochanteric fractures with lateral wall fractures or the subtrochanteric extension were considered unstable in the past, but most of the fractures were well united without fixation failure in our study. Unlike sliding hip screws, all currently available nail systems use the greater trochanteric tip as the entry point. Unlike plate system, nailing in a comminuted fracture in the greater trochanter might make fish mouth phenomenon, which causes varus angulation and shortening that can progress to fixation failure. So, a greater trochanter with a trochanteric fracture can be a risk factor, but there was no statistical significance.
There are some limitations of this study. First, we had a limited number of patients and follow-up was difficult because the patients were geriatric. If a patient dies or cannot be followed up properly, treatment outcomes cannot be fully evaluated. The statistical power of the study is relatively low because of the small sample size and the big difference in the size of the two groups. Second, the fracture patterns or classifications could have been affected by interobserver variability, although we asked three experts to examine the images. Third, for basicervical type of fractures that include typical two-part basilar neck fractures and highly located trochanteric fractures, we used an arbitrary definition.
Among the risk factors of fixation failure after osteosynthesis using IM nailing in elderly patients with trochanteric fractures, unmodifiable patient factors include a higher BMI, basicervical type of fracture on 3D-CT. Surgeon factors include nonanatomical reduction, especially of the anterior cortex, and posterior positioning of the lag screw on a lateral view. The surgeon should take care during surgery to reduce the impact of these surgeon factors. In addition, although being considered stable according to the AO/OTA classification, basicervical type of fracture on 3D-CT might be highly associated with fixation failure. Fracture classification assisted by 3D-CT can be more beneficial when IM nailing is performed in trochanteric hip fractures.
References
1. Park SR, Kang JS, Kim HS, Lee WH, Kim YH. Treatment of intertrochanteric fracture with the Gamma AP locking nail or by a compression hip screw: a randomised prospective trial. Int Orthop. 1998; 22(3):157–160. PMID: 9728307.
2. Eberle S, Bauer C, Gerber C, von Oldenburg G, Augat P. The stability of a hip fracture determines the fatigue of an intramedullary nail. Proc Inst Mech Eng H. 2010; 224(4):577–584. PMID: 20476505.

3. Ciufo DJ, Zaruta DA, Lipof JS, Judd KT, Gorczyca JT, Ketz JP. Risk factors associated with cephalomedullary nail cutout in the treatment of trochanteric hip fractures. J Orthop Trauma. 2017; 31(11):583–588. PMID: 28827502.

4. Bojan AJ, Beimel C, Taglang G, Collin D, Ekholm C, Jonsson A. Critical factors in cut-out complication after Gamma Nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013; 14:1. PMID: 23281775.

5. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures: mechanical failure after internal fixation. J Bone Joint Surg Br. 1990; 72(1):26–31. PMID: 2298790.

6. Matre K, Vinje T, Havelin LI, et al. TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am. 2013; 95(3):200–208. PMID: 23389782.
7. Fogagnolo F, Kfuri M Jr, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AOASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004; 124(1):31–37. PMID: 13680275.

8. Bess RJ, Jolly SA. Comparison of compression hip screw and gamma nail for treatment of peritrochanteric fractures. J South Orthop Assoc. 1997; 6(3):173–179. PMID: 9322196.
9. Butt MS, Krikler SJ, Nafie S, Ali MS. Comparison of dynamic hip screw and gamma nail: a prospective, randomized, controlled trial. Injury. 1995; 26(9):615–618. PMID: 8550169.

10. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998; (348):87–94. PMID: 9553538.

11. Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. 1949; 31B(2):190–203. PMID: 18150534.

12. Siddiqui SA, Rocco J, McKechnie A, Meyerson RI, Sands AK. Technique for percutaneous insertion of intramedullary nail for intertrochanteric hip fracture. Am J Orthop (Belle Mead NJ). 2004; 33(3):117–120. PMID: 15074458.
13. Siegel RS. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1996; 78(9):1447.
14. Cool P. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1996; 78(9):1447.
15. Cleveland M, Bosworth DM, Thompson FR. Management of the trochanteric fracture of the femur. J Am Med Assoc. 1948; 137(14):1186–1190. PMID: 18871864.

16. Jung EY, Oh IT, Shim SY, Yoon BH, Sung YB. The effect of valgus reduction on the position of the blade of the proximal femoral nail antirotation in intertrochanteric hip fractures. Clin Orthop Surg. 2019; 11(1):36–42. PMID: 30838106.

17. Kim TY, Lee YB, Chang JD, et al. Torsional malalignment, how much significant in the trochanteric fractures? Injury. 2015; 46(11):2196–2200. PMID: 26303999.

18. Chun YS, Oh H, Cho YJ, Rhyu KH. Technique and early results of percutaneous reduction of sagittally unstable intertrochateric fractures. Clin Orthop Surg. 2011; 3(3):217–224. PMID: 21909469.

Fig. 2
Illustration of basicervical type of fracture on a computed tomographic scan. The continuous white line represents the area of typical trochanteric fractures and two interuppted gray lines represent the area of basicervical type of fractures.
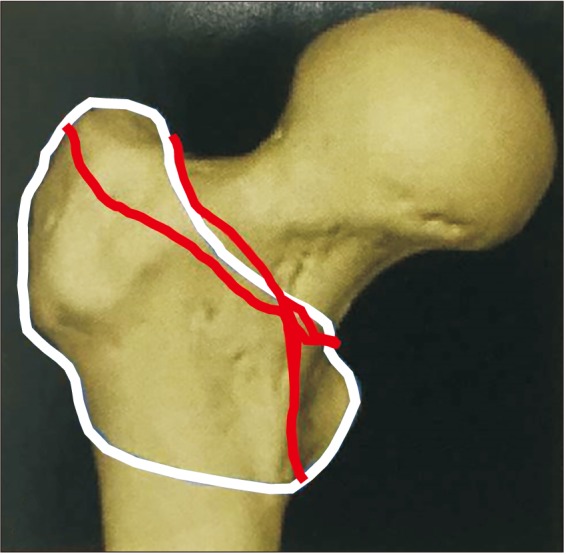
Fig. 3
(A) An 88-year-old woman showed basicervical type of fracture with varus angulation before surgery. (B) The fracture was OTA A12 type fracture with greater trochanter comminution. (C) Surgery was performed by using Zimmer natural nail. (D) The lag screw was pulled out at 2 weeks after surgery. (E) The lag screw was cut out of the femoral head at 6 weeks after surgery.

Fig. 4
(A) An 81-year-old woman fell on the ground. The proximal fragment was short and varus angulated before surgery. (B) The three-dimensional computed tomographic scan shows the OTA-A21 fracture. (C) The fracture was reduced by the Proximal Femoral Nail Anti-rotation. (D) The lag screw was cutting through at 3 months after surgery. (E) Conversion to hemiarthroplasty with wiring was performed.
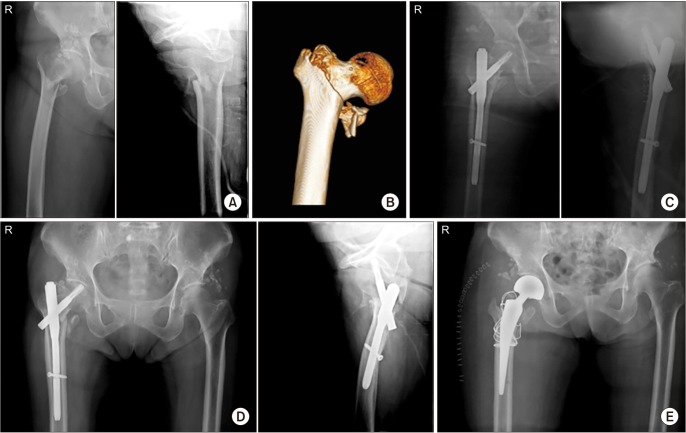
Table 1
Statistical Comparison of Nonfailure and Failure Groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download