Abstract
Distal ulnar fractures are commonly accompanied by distal radial fractures, and several treatment options such as plate osteosynthesis and pinning with Kirschner's wires are used. In this study, we present a technique using headless compression screws to achieve bony union of distal ulnar fractures. From November 2016 to November 2018, we treated 11 patients with distal ulnar fractures combined with distal radial fractures with headless compression screws (DePuy Synthes). Patients were instructed to maintain a short-arm splint for less than two weeks after the treatment. The mean time to bony union was 6.5 weeks, mean Quick Disabilities of the Arm, Shoulder, and Hand score was 14.6 points, and mean visual analog scale score was 1.09 points. Full range of motion was possible in all directions after surgery and no specific complications were observed. The suggested technique allows minimal incision and minimally invasive intramedullary fixation and can promote bony union in a simple way without specific complications.
Distal ulnar neck fractures are commonly accompanied by distal radial fractures.1) The incidence of isolated distal ulnar fractures is lower than that of distal radial fractures, and the optimal treatment remains controversial. Once the fixation of a distal radial fracture is done and the distal ulna is reduced, fixation of the distal ulnar fracture itself could be unnecessary, but if displacement remains, functional problems in the distal radioulnar joint can occur.23) Thus, surgical fixation is necessary if displacement or instability remains. Plate osteosynthesis and pinning are widely used for distal ulnar fractures.4) The same techniques are often performed to treat ulnar fractures combined with radial fractures. To reduce the operation time, we devised a intramedullary fixation technique using a headless compression screw, which is a simple and minimally invasive technique that requires a small skin incision.
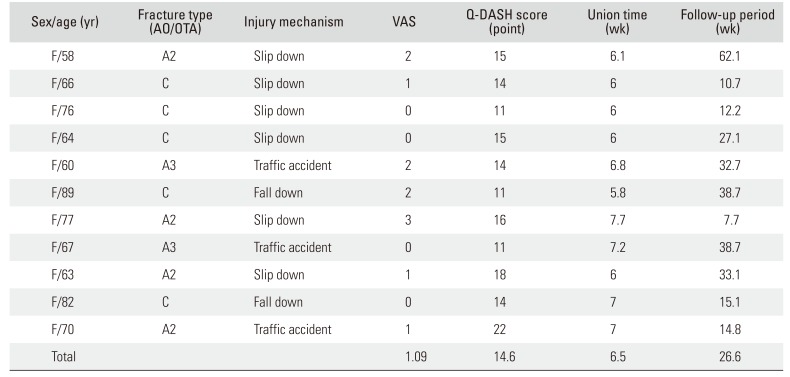
From November 2016 to November 2018, we treated 11 patients with headless compression screws. Surgical indications include displacement over 50%, inclination over 10°, comminuted fractures, intra-articular fractures, instability, and high-energy injuries.456) All patients were women with a mean age of 70 years (range, 58 to 89 years). The mean follow-up period was 26.6 weeks (range, 7.7 to 62.1 weeks). Mechanisms of injury include a slip down (n = 6), fall down (n = 2), and traffic accident (n = 3). According to the AO-Müller/Orthopaedic Trauma Association (AO/OTA) classification, the ulnar fractures were type A2 in four patients, type A3 in two, and type C in five (Table 1).
In all patients, surgery was performed by using Synthes headless compression screws (DePuy Synthes, West Chester, PA, USA), which are offered in three different diameters, 3.0 mm, 4.5 mm, and 6.5 mm. The mean diameter of the ulnar neck and head in our patients was 7.4 mm (range, 5.5 to 9.07 mm) and 20.27 mm (range, 18.7 to 21.9 mm), respectively. To safely avoid the foveal insertion and to fix the shaft proximal to the fracture site, we determined the 4.5-mm screws are optimal. With the wrist flexed to 90°, a focal skin incision is made on the dorsal aspect near the ulnar head. Reduction is done under the C-arm guide, and then a guide pin is inserted with care to avoid the ulnar fovea (the insertion of the triangular fibrocartilage complex [TFCC]) but to pass through the central and radial portion (concave area) in which the articular disc of the TFCC lies. The intramedullary canal is drilled with a 4.0-mm cannulated drill bit. The optimal 4.5-mm headless compression was inserted along the guide pin (Fig. 1). For less than 2 weeks, the wrist is placed in a short-arm splint and a tolerable range of motion including forearm supination and pronation is allowed after that period. Some patients with less pain were permitted to start range of motion exercises the day after the operation.
Functional scores were evaluated at the time of bony union with a visual analog scale (VAS), Quick Disabilities of the Arm, Shoulder, and Hand (Q-DASH) questionnaire,78) and the time required for bony union was checked. The mean VAS score was 1.09, and mean Q-DASH score was 14.6 points, mean time to bony union was 6.5 weeks. All patients were able to perform full range of wrist motions. No specific complications such as screw loosening and infection were seen. No patient complained of ulnar-side wrist pain and signs of TFCC injuries were not checked.
This study was approved by the Institutional Review Board of Wonju Severance Christian Hospital (IRB No. CR319157).
An 89-year-old woman slipped down stairs and sustained an AO/OTA type C , distal ulnar, open, comminuted fracture accompanied by a distal radial fracture. Plate fixation was done for the radial fracture and headless compression screw fixation was done for the distal ulnar fracture. Bony union was achieved at postoperative 5.8 weeks and excellent functional and radiologic results were acquired (Fig. 2).
A 64-year-old woman slipped down and sustained an AO/OTA type C, intra-articular, distal ulnar fracture. Plate fixation was done for the radial fracture and headless compression screw fixation was done for the distal ulnar fracture. Bony union was achieved at postoperative 6 weeks and excellent functional and radiologic results were acquired (Fig. 3).
There is no established treatment for distal ulnar fractures accompanied by distal radial fractures. Fractures in the ulnar styloid process are most common but they sometimes require surgical fixation for fractures of the ulnar head or neck.17) Ring et al.7) mentioned that if displacement or an intra-articular fractures is not see in the distal ulna after reduction of a distal radial fracture, surgical fixation is not required. Richards and Deal8) stated that if there is more than 50% displacement and 10° of inclination in distal ulnar fractures, they imply a rupture of interosseous membrane and longitudinal instability, which are indications for surgical fixation. Cha et al.4) included displacement of more than 50%, inclination over 15°, comminuted fractures, and high-energy trauma in surgical indications. According to Brakenbury et al.,9) the nonunion rate significantly increases in distal-third ulnar fractures because of severed nutritional arteries and lack of covering muscle. In addition, they reported that fixation of the distal ulna enables early range of motion and could result in improved functional outcomes and fewer complications such as stiffness that is caused by a prolonged immobilization period with splints.
Several techniques are used for fixation of the distal ulna. Plate fixation blocks rotation of the fracture site and provides higher union rates than intramedullary nail fixation, but it requires more soft tissue dissection.4) However, distal ulna portion is narrow and curved, so plate fixation can be challenging. Ring et al.7) used condylar blade plate fixation and achieved bony union in all 24 patients but they had difficulty in fixing intra-articular fragments. Kang et al.5) used tension band wiring and achieved good results, but the mean age of the patients was 42 years. Other methods such as percutaneous pinning are simple procedures but fixation strength is weak, so pin loosening can be a problem.267) We tried to suggest an alternative fixation method, which requires minimal dissection but offers stronger fixation than pinning. Intramedullary headless compression screw fixation requires minimal dissection and can achieve firm fixation with a 4.5-mm diameter screw. Entering through the central portion of the TFCC articular disc, while avoiding the rim and insertion site of the TFCC, did not cause any problem in our patients. No patient had ulnar-side wrist pain, secondary arthritis, or distal radioulnar joint instability. This may be related to lack of sensory innervation and tendinous portion of the radial/central portion of the TFCC, in which type IA injuries are treated with debridement only. It can also be assumed that, since no patients showed ulnar-side wrist pain, there were no initial concomitant TFCC tears. This may be due to the distribution of the forces to the ulnar bony structures rather than the ligaments alone. In patients presenting with ulnar-side wrist pain after bony union, initial TFCC tears need to be assumed and additional evaluation with magnetic resonance imaging should be considered.
We hope the suggested technique will be further validated by studies based on the analysis of isolated ulnar fractures, greater study participants, longer follow-up, and functional evaluation without statistical bias.
References
1. Biyani A, Simison AJ, Klenerman L. Fractures of the distal radius and ulna. J Hand Surg Br. 1995; 20(3):357–364. PMID: 7561413.

2. Dennison DG. Open reduction and internal locked fixation of unstable distal ulna fractures with concomitant distal radius fracture. J Hand Surg Am. 2007; 32(6):801–805. PMID: 17606057.

3. Foster BJ, Bindra RR. Intrafocal pin plate fixation of distal ulna fractures associated with distal radius fractures. J Hand Surg Am. 2012; 37(2):356–359. PMID: 22192166.

4. Cha SM, Shin HD, Kim KC, Park E. Treatment of unstable distal ulna fractures associated with distal radius fractures in patients 65 years and older. J Hand Surg Am. 2012; 37(12):2481–2487. PMID: 23044479.

5. Kang HJ, Shim DJ, Yong SW, Yang GH, Hahn SB, Kang ES. Operative treatment for isolated distal ulnar shaft fracture. Yonsei Med J. 2002; 43(5):631–636. PMID: 12402377.

6. Han SH, Hong IT, Kim WH. LCP distal ulna plate fixation of irreducible or unstable distal ulna fractures associated with distal radius fracture. Eur J Orthop Surg Traumatol. 2014; 24(8):1407–1413. PMID: 24566964.

7. Ring D, McCarty LP, Campbell D, Jupiter JB. Condylar blade plate fixation of unstable fractures of the distal ulna associated with fracture of the distal radius. J Hand Surg Am. 2004; 29(1):103–109. PMID: 14751112.

8. Richards TA, Deal DN. Distal ulna fractures. J Hand Surg Am. 2014; 39(2):385–391. PMID: 24411292.

9. Brakenbury PH, Corea JR, Blakemore ME. Non-union of the isolated fracture of the ulnar shaft in adults. Injury. 1981; 12(5):371–375. PMID: 7263044.

Fig. 1
(A) A guide wire was inserted from the ulnar head on the dorsal aspect to the ulnar distal shaft (case I). (B) A 4-mm drill bit was inserted through the guide wire. (C) The 4.5-mm headless compression screw was inserted along the guide wire.
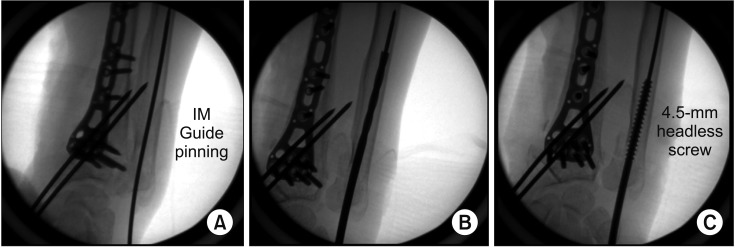
Fig. 2
(A) Radiographs showing an AO type C distal ulnar fracture with comminution. Open wound was noted on the ulnar aspect of the wrist. (B) Radiographs showing internal fixation of the distal radius with use of Arix Volar Distal Radius anatomical plate, screws, and K-wires and fixation of the ulnar neck with use of DePuy Synthes headless compression screw. Ulnar fixation could be done regardless of the open wound. (C) Six months after the operation, complete bony union was achieved. Lt: left.
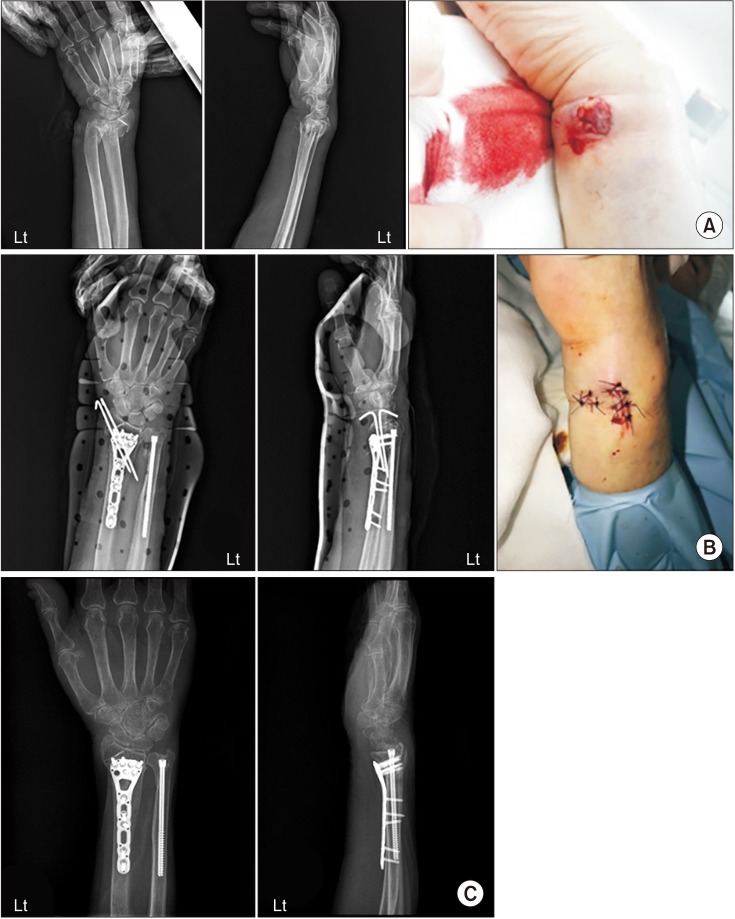
Fig. 3
(A) Radiographs showing distal ulnar intra-articular fracture (AO type C). (B) Radiographs showing internal fixation of both distal radius and ulnar: Arix Volar Distal Radius anatomical plate and screws for distal radius; DePuy Synthes headless compression screw for the ulnar neck. (C) Computed tomographic scans showing the intra-articular fracture pattern with the ulnar neck fracture line extending to the radial sigmoid notch in the axial plane. (D) Clinical photos showing that full range of motion of the wrist is possible in all directions after bony union. Lt: left.

Table 1
Patient Data




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download