Abstract
Purpose
To compare the intraocular pressure (IOP) in diabetic macular edema (DME) patients and macular edema associated with branch retinal vein occlusion (BRVO) patients after intravitreal preservative-free Triamcinolone injection.
Methods
This study included 36 patients diagnosed with DME and 44 patients diagnosed with BRVO with macular edema. Both groups were treated with intravitreal preservative-free Triamcinolone (Maqaid®, Wakamoto Pharmaceutical Co., Ltd., Tokyo, Japan) injection, and we compared the IOPs of the two groups determined before injection and at 1, 2, 3, and 6 months after injection. We also compared the IOP elevation ratios and durations, and central foveal thickness (CFT) changes using optical coherence tomography.
Results
In both groups, there was no statistical significance in the IOP before injection and at 1, 2, 3, and 6 months after injection. However, the IOP elevation ratio in the DME patients (38.9%) was significantly higher than that in the BRVO patients (15.9%) (p = 0.02). The duration of IOP elevation in the DME patients (1.14 ± 1.85 months) was significantly longer than that in the BRVO patients (0.30 ± 1.20 months) (p = 0.03). When the IOP was not controlled, we used IOP-lowering agents, and two patients in the DME were treated with glaucoma surgery. There was no statistical significance in the CFT before injection and at 1, 2, or 3 months after injection between the two groups (p = 0.72, p = 0.26, p = 0.66, p = 0.34, respectively). However, the CFT after 6 months was 328 ± 103 µm in the DME group and 434 ± 189 µm in the BRVO; this difference was significant (p < 0.01).
Figures and Tables
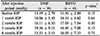
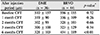
Table 2
Between DME group and BRVO group, comparison of average IOP during 6 months after intravitreal preservative-free triamcinolone injection
References
1. Kim SY, Nah EH, Cho S. Prevalence of comorbidities among patients with diabetes. J Health Inform Stat. 2018; 43:237–244.

2. Yang JY, Kim NK, Lee YJ, et al. Prevalence and factors associated with diabetic retinopathy in a Korean adult population: the 2008-2009 Korea National Health and Nutrition Examination Survey. Diabetes Res Clin Pract. 2013; 102:218–224.


3. Lee JY, Yoon YJ, Kim HK, et al. Baseline characteristics and risk factors of retinal vein occlusion: a study by the Korean RVO Study Group. J Korean Med Sci. 2013; 28:136–144.



4. Lee H, Shah GK. Intravitreal triamcinolone as primary treatment of cystoid macular edema secondary to branch retinal vein occlusion. Retina. 2005; 25:551–555.


5. Gillies MC, Simpson JM, Gaston C, et al. Five-year results of a randomized trial with open-label extension of triamcinolone acetonide for refractory diabetic macular edema. Ophthalmology. 2009; 116:2182–2187.


6. Zhu MD, Cai FY. Development of experimental chronic intraocular hypertension in the rabbit. Aust N Z J Ophthalmol. 1992; 20:225–234.


7. Lee CH, Jang MH, Seo YS. Effectiveness of intravitreal preservative-free triamcinolone injection for refractory macular edema secondary to retinal vein occlusion. J Korean Ophthalmol Soc. 2018; 59:730–737.

8. Becker B. Diabetes mellitus and primary open-angle glaucoma. The XXVII Edward Jackson Memorial Lecture. Am J Ophthalmol. 1971; 71(1 Pt 1):1–16.

9. Podos SM, Becker B, Morton WR. High myopia and primary open-angle glaucoma. Am J Ophthalmol. 1966; 62:1038–1043.


10. Gaston H, Absolon MJ, Thurtle OA, et al. Steroid responsiveness in connective tissue diseases. Br J Ophthalmol. 1983; 67:487–490.



11. Park HY, Yi K, Kim HK. Intraocular pressure elevation after intravitreal triamcinolone acetonide injection. Korean J Ophthalmol. 2005; 19:122–127.


12. Gillies MC, Kuzniarz M, Craig J, et al. Intravitreal triamcinolone-induced elevated intraocular pressure is associated with the development of posterior subcapsular cataract. Ophthalmology. 2005; 112:139–143.


13. Bashshur ZF, Terro AM, Haibi CP, et al. Intravitreal triamcinolone acetonide: pattern of secondary intraocular pressure rise and possible risk factors. Clin Ophthalmol. 2008; 2:269–274.


14. Vasconcelos-Santos DV, Nehemy PG, Schachat AP, Nehemy MB. Secondary ocular hypertension after intravitreal injection of 4 mg of triamcinolone acetonide: incidence and risk factors. Retina. 2008; 28:573–580.

15. Kiddee W, Trope GE, Sheng L, et al. Intraocular pressure monitoring post intravitreal steroids: a systematic review. Surv Ophthalmol. 2013; 58:291–310.


16. Armaly MF. Statistical attributes of the steroid hypertensive response in the clinically normal eye. I. The demonstration of three levels of response. Invest Ophthalmol. 1965; 4:187–197.

17. Armaly MF. Dexamethasone ocular hypertension in the clinically normal eyes: II. The untreated eyes, outflow facility, and concentration. Arch Ophthalmol. 1966; 75:776–782.

18. Wordinger RJ, Clark AF. Effects of glucocorticoids on the trabecular meshwork: towards a better understanding of glaucoma. Prog Retin Eye Res. 1999; 18:629–667.


19. Shaarawy T, Sherwood M, Hitchings R, et al. Glaucoma. 2nd ed. Vol. 1. Philadelphia: Saunders;2014. p. 438.
20. Kang HK, Chin HS. Complications after intravitreal triamcinolone acetonide injection: incidence and risk factors. J Korean Ophthalmol Soc. 2012; 53:76–86.

21. Jonas JB, Kreissig I, Degenring R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol. 2003; 87:24–27.


22. Jonas JB, Kreissig I, Degenring R. Secondary chronic open-angle glaucoma after intravitreal triamcinolone acetonide. Arch Ophthalmol. 2003; 121:729–730.


24. Bernstein HN, Mills DW, Becker B. Steroid-induced elevation of intraocular pressure. Arch Ophthalmol. 1963; 70:15–18.


25. Kalina RE. Increased intraocular pressure following subconjunctival corticosteroid administration. Arch Ophthalmol. 1969; 81:788–790.


26. Wingate RJ, Beaumont PE. Intravitreal triamcinolone and elevated intraocular pressure. Aust N Z J Ophthalmol. 1999; 27:431–432.

27. Cho YK. Early intraocular pressure and anterior chamber depth changes after phacoemulsification and intraocular lens implantation in nonglaucomatous eyes: comparison of groups stratified by axial length. J Cataract Refract Surg. 2008; 34:1104–1109.

28. Karakahya RH, Kalaycı D, Karakurt A. Ocular hypertension and glaucoma after intravitreal injection of triamcinolone acetonide. Middle Black Sea Journal of Health Science. 2018; 4:24–30.

29. Maia M, Farah ME, Belfort RN, et al. Effects of intravitreal triamcinolone acetonide injection with and without preservative. Br J Ophthalmol. 2007; 91:1122–1124.



30. Chang YS, Wu CL, Tseng SH, et al. In vitro benzyl alcohol cytotoxicity: implications for intravitreal use of triamcinolone acetonide. Exp Eye Res. 2008; 86:942–950.


31. Otsuka H, Kawano H, Sonoda S, et al. Particle-induced endophthalmitis: possible mechanisms of sterile endophthalmitis after intravitreal triamcinolone. Invest Ophthalmol Vis Sci. 2013; 54:1758–1766.






 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download