1. World Health Organization. Global report on diabetes 2016. Geneva: World Health Organization;2016.
2. Korea Centers for Disease Control and Prevention, Korean Academy of Medical Sciences. 2017 Report for Korea National Health and Nutrition Examination Survey and Korean Youth Risk Behavior Web-based Survey. updated 2017 Nov 9. Available from:
https://knhanes.cdc.go.kr/knhanes/sub04/sub04_04.do.
3. Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, Shuai Y, Zhang B, Zhang J, Thompson TJ, Gerzoff RB, Roglic G, Hu Y, Bennett PH. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet. 2008; 371:1783–1789. PMID:
18502303.

4. Lindstrom J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemio K, Hamalainen H, Harkonen P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Mannelin M, Paturi M, Sundvall J, Valle TT, Uusitupa M, Tuomilehto J. Finnish Diabetes Prevention Study Group. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006; 368:1673–1679. PMID:
17098085.
5. Diabetes Prevention Program Research Group. Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenne-man AT, Brown-Friday JO, Goldberg R, Venditti E, Nathan DM. 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009; 374:1677–1686. PMID:
19878986.
6. Korea Centers for Disease Control and Prevention, Korean Academy of Medical Sciences. Guideline development and dissemination for prevention and control of chronic disease. cited 2018 Oct 10. Available from:
http://www.cdc.go.kr.
7. American Diabetes Association. Diabetes mellitus and exercise. Diabetes Care. 1997; 20:1908–1912. PMID:
9405917.
8. Maeng JY, Oh JK. The effect of 12-weeks of synchronized exercise on insulin resistance in female elderly with type 2 diabetes. Korean J Sport. 2017; 15:937–946.
9. Park JJ, Kim HJ. Effects of combined treatment of aerobic exercise and resistance exercise on hemoglobin A1c, blood lipids, bone mineral content in patients with type II diabetes mellitus. J Korean Soc Living Environ Syst. 2015; 22:722–729.

10. Thomas DE, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2006; (3):CD002968. PMID:
16855995.

11. Kang SJ, Baek UH. Effects of resistance exercise on skeletal muscle index, muscle fitness, HbA1c and cardiovascular risk factors in middle-aged women with type II diabetes mellitus. Korean J Growth Dev. 2015; 23:253–260.
12. Jun JY. The effects of programmed jogging on metabolism and cardio-pulmonary function of type II diabetic patients. Kanhohak Tamgu. 1994; 3:19–42. PMID:
7832871.
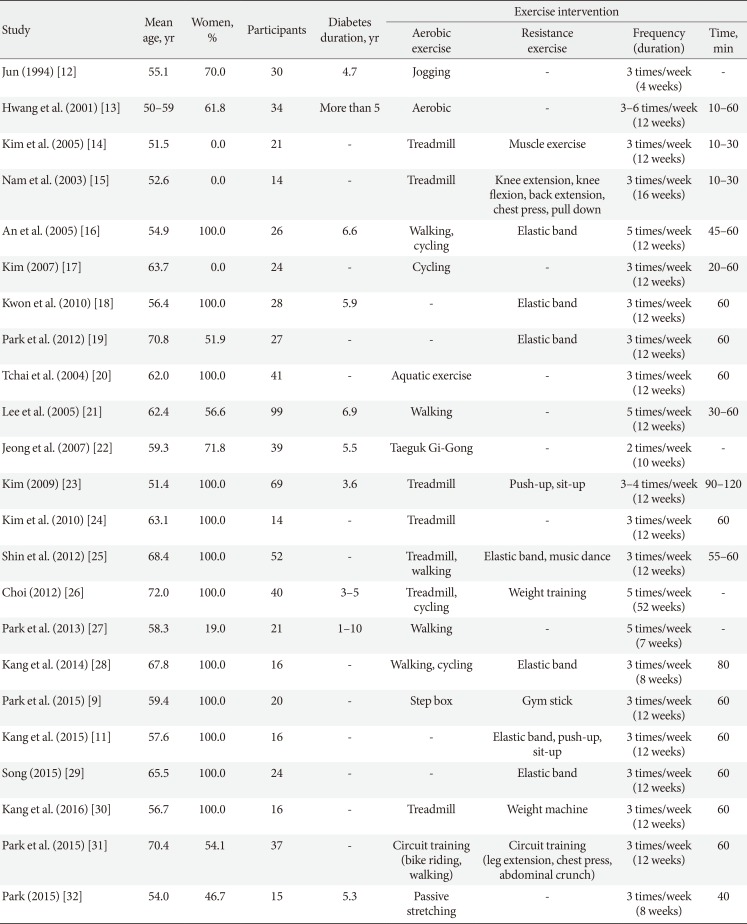
13. Hwang AR, Yoo JS, Kim CJ. The effects of planned exercise program on metabolism, cardiopulmonary function and exercise compliance in type 2 diabetes mellitus patients. J Korean Acad Nurs. 2001; 31:20–30.

14. Kim TH, Kim SS, Hong YS, Shin MS, Chung YR, Kang JY. The effects of 12 weeks exercise program on superoxide dismutase and malondialdehyde of non-insulin dependent diabetes mellitus (NIDDM) patients. J Coach Dev. 2005; 7:217–224.
15. Nam GH, Shin MS, Yu JH, Bae JJ, Lee SH, Kim SS, Hong YS, Byeon JJ, Park HG. The effect of exercise program during 16 weeks on leptin, HbAlc, BMI and body composition in middle aged men with obesity and NIDDM. J Sport Leis Stud. 2003; 20:1115–1126.

16. An KH, Min KW, Han KA. The effects of aerobic training versus resistance training in non-obese type 2 diabetics. J Korean Diabetes Assoc. 2005; 29:486–494.
17. Kim SH. The blood glucose index and lipid peroxidation after 12 weeks of aerobic exercise in type 2 diabetic older patients. J Coach Dev. 2007; 9:327–334.
18. Kwon HR, Han KA, Ku YH, Ahn HJ, Koo BK, Kim HC, Min KW. The effects of resistance training on muscle and body fat mass and muscle strength in type 2 diabetic women. Korean Diabetes J. 2010; 34:101–110. PMID:
20548842.

19. Park SY, Kim CS, Nam SH. Effects of elastic band resistance exercise program on body functions and HbA1c of the elderly with type 2 diabetes. J Korean Soc Phys Ther. 2012; 24:362–369.
20. Tchai E, Park SC, Park JB, Yoon JW. Effects of aquatic exercise program on body composition, blood lipid profiles, insulin sensitivity and aerobic capacity of the old patients with non insulin dependent diabetes mellitus. Korean J Sport Sci. 2004; 13:641–651.
21. Lee HJ, Park KY, Park HS, Kim IJ. The effects of problem solving nursing counseling and intensified walking exercise on diabetic self-care, coping strategies, and glycemic control among clients with DM Type II. Taehan Kanho Hakhoe Chi. 2005; 35:1314–1324. PMID:
16418558.

22. Jeong IS, Lee HJ, Kim MH. The effect of the taeguk gi-gong exercise on insulin resistance and blood glucose in patients with type II diabetes mellitus. J Korean Acad Fundam Nurs. 2007; 14:44–52.
23. Kim NI. The effects of the week exercise time on atherogenic indics and reduce glucose, HbA1c in the type II diabetes melltus. Korean J Sport Sci. 2009; 18:1125–1135.
24. Kim CH, Seo YS, Lee JW. The effect of 12-week aerobic exercise on inflammatory markers of elderly women patients with diabetes mellitus. Korean J Sport Sci. 2010; 19:1337–1349.
25. Shin WT, Lee JW. The effect of exercise type on blood vessel inflammatory markers in elderly women patients with diabetes mellitus. J Korea Soc Wellness. 2012; 7:201–211.
26. Choi PB. Effects and correlation analysis of long-term exercise on diabetes indicators, lipid profile, and pancreatic cancer factor in the elderly with type 2 diabetes mellitus. Korean J Exerc Rehabil. 2012; 8:93–102.
27. Park SM, Kim GC, Kim LS, Kwak YS. Effects of walking exercise on diabetic parameters and vascular compliance in type II diabetes mellitus patients. J Korean Inst Orient Med Diagn. 2013; 17:241–252.
28. Kang SJ, Ryu BH. Effects of combined exercise on HbA1c, cardiovascular disease risk factors, and physical fitness in elderly women with type 2 diabetes mellius. J Korean Acad Kinesiol. 2014; 16:21–30.
29. Song NH. The effects of elastic band training on glycated hemoglobin, insulin resistance of the elderly female patients with diabetes. Korean J Sport Sci. 2015; 24:1359–1369.
30. Kang SJ, Ko KJ, Baek UH. Effects of 12 weeks combined aerobic and resistance exercise on heart rate variability in type 2 diabetes mellitus patients. J Phys Ther Sci. 2016; 28:2088–2093. PMID:
27512271.

31. Park SY, Lee IH. Effects on training and detraining on physical function, control of diabetes and anthropometrics in type 2 diabetes: a randomized controlled trial. Physiother Theory Pract. 2015; 31:83–88. PMID:
25230894.

32. Park SH. Effects of passive static stretching on blood glucose levels in patients with type 2 diabetes mellitus. J Phys Ther Sci. 2015; 27:1463–1465. PMID:
26157241.

33. Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical trials. JAMA. 2001; 286:1218–1227. PMID:
11559268.

34. Irvine C, Taylor NF. Progressive resistance exercise improves glycaemic control in people with type 2 diabetes mellitus: a systematic review. Aust J Physiother. 2009; 55:237–246. PMID:
19929766.

35. Ishiguro H, Kodama S, Horikawa C, Fujihara K, Hirose AS, Hirasawa R, Yachi Y, Ohara N, Shimano H, Hanyu O, Sone H. In search of the ideal resistance training program to improve glycemic control and its indication for patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Sports Med. 2016; 46:67–77. PMID:
26604100.

36. Zou Z, Cai W, Cai M, Xiao M, Wang Z. Influence of the intervention of exercise on obese type II diabetes mellitus: a meta-analysis. Prim Care Diabetes. 2016; 10:186–201. PMID:
26553963.

37. Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. 2006; 29:2518–2527. PMID:
17065697.

38. Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Callister R. Efficacy of interventions that include diet, aerobic and resistance training components for type 2 diabetes prevention: a systematic review with meta-analysis. Int J Behav Nutr Phys Act. 2014; 11:2. PMID:
24423095.

39. Schwingshackl L, Missbach B, Dias S, Konig J, Hoffmann G. Impact of different training modalities on glycaemic control and blood lipids in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetologia. 2014; 57:1789–1797. PMID:
24996616.

40. Qiu S, Cai X, Sun Z, Zugel M, Steinacker JM, Schumann U. Aerobic interval training and cardiometabolic health in patients with type 2 diabetes: a meta-analysis. Front Physiol. 2017; 8:957. PMID:
29218018.

41. de Mello Meirelles C, Gomes PSC. Acute effects of resistance exercise on energy expenditure: revisiting the impact of the training variables. Rev Bras Med Esporte. 2004; 10:122–130.
42. Scala D, McMillan J, Blessing D, Rozenek R, Stone M. Metabolic cost of a preparatory phase of training in weight lifting: a practical observation. J Strength Cond Res. 1987; 1:48–52.

43. Chudyk A, Petrella RJ. Effects of exercise on cardiovascular risk factors in type 2 diabetes: a meta-analysis. Diabetes Care. 2011; 34:1228–1237. PMID:
21525503.
44. Despres JP. Visceral obesity, insulin resistance, and dyslipidemia: contribution of endurance exercise training to the treatment of the plurimetabolic syndrome. Exerc Sport Sci Rev. 1997; 25:271–300. PMID:
9213095.
45. Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, Andrews GR. The effectiveness of exercise training in lowering blood pressure: a meta-analysis of randomised controlled trials of 4 weeks or longer. J Hum Hypertens. 1997; 11:641–649. PMID:
9400906.

46. Nielsen AB, de Fine Olivarius N, Gannik D, Hindsberger C, Hollnagel H. Structured personal diabetes care in primary health care affects only women's HbA1c. Diabetes Care. 2006; 29:963–969. PMID:
16644621.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download