1. Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, Connolly V, King H. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005; 28:2130–2135. PMID:
16123478.
2. Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia. 2001; 44(Suppl 2):S14–S21. PMID:
11587045.

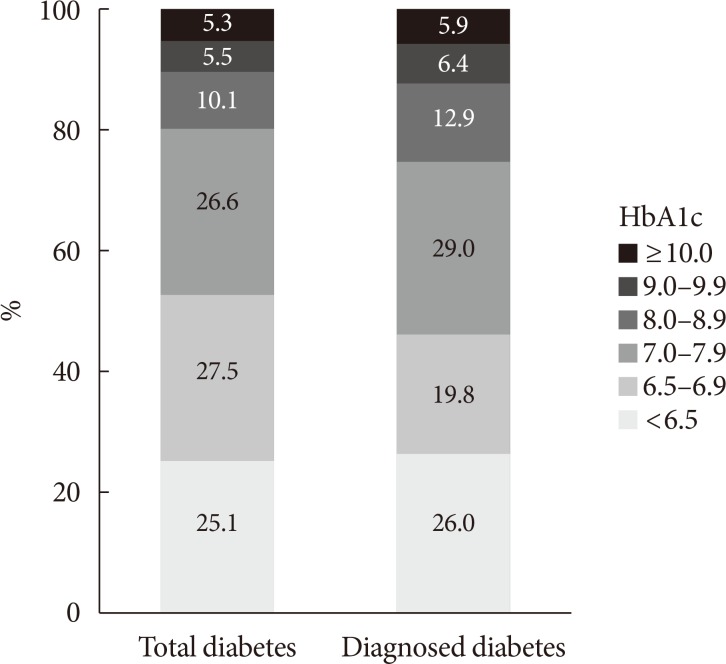
3. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Jang MJ, Kim Y, Oh K, Kim DJ, Cha BY;. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J. 2013; 37:349–357. PMID:
24199164.

4. Jeon JY, Kim DJ, Ko SH, Kwon HS, Lim S, Choi SH, Kim CS, An JH, Kim NH, Won JC, Kim JH, Cha BY, Song KH. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Current status of glycemic control of patients with diabetes in Korea: the fifth Korea National Health and Nutrition Examination Survey. Diabetes Metab J. 2014; 38:197–203. PMID:
25003073.

5. Vital Statistics Division Statistics Korea. Shin HY, Lee JY, Kim JE, Lee S, Youn H, Kim H, Lee J, Park MS, Huh S. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61:573–584.

6. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502. PMID:
4337382.

7. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014; 37(Suppl 1):S81–S90. PMID:
24357215.
8. Oh SW, Shin SA, Yun YH, Yoo T, Huh BY. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res. 2004; 12:2031–2040. PMID:
15687405.

10. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2014 update: a report from the American Heart Association. Circulation. 2014; 129:e28–e92. PMID:
24352519.
11. Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul). 2015; 30:142–146. PMID:
26194073.

12. Sesti G, Antonelli Incalzi R, Bonora E, Consoli A, Giaccari A, Maggi S, Paolisso G, Purrello F, Vendemiale G, Ferrara N. Management of diabetes in older adults. Nutr Metab Cardiovasc Dis. 2018; 28:206–218. PMID:
29337017.

13. Ross NA, Gilmour H, Dasgupta K. 14-Year diabetes incidence: the role of socio-economic status. Health Rep. 2010; 21:19–28.
14. Lee TC, Glynn RJ, Peña JM, Paynter NP, Conen D, Ridker PM, Pradhan AD, Buring JE, Albert MA. Socioeconomic status and incident type 2 diabetes mellitus: data from the Women's Health Study. PLoS One. 2011; 6:e27670. PMID:
22194788.

15. Kim SH, Lee SY, Kim CW, Suh YJ, Hong S, Ahn SH, Seo DH, Nam MS, Chon S, Woo JT, Baik SH, Park Y, Lee KW, Kim YS. KNDP Study Group. Impact of socioeconomic status on health behaviors, metabolic control, and chronic complications in type 2 diabetes mellitus. Diabetes Metab J. 2018; 42:380–393. PMID:
30113143.

16. Shin WY, Kim HC, Lee T, Jeon DH, Ha KH, Kim DJ, Chang HJ. Combined effects of diabetes and low household income on mortality: a 12-year follow-up study of 505 677 Korean adults. Diabet Med. 2018; 35:1345–1354. PMID:
29851428.

17. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020. PMID:
19675201.
18. Ha KH, Kim DJ. Current status of managing diabetes mellitus in Korea. Korean J Intern Med. 2016; 31:845–850. PMID:
27604796.

20. Diabetes Control and Complications Trial Research Group. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993; 329:977–986. PMID:
8366922.

21. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–853. PMID:
9742976.
22. Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, Raskin P, Zinman B. Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005; 353:2643–2653. PMID:
16371630.
23. Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, Willett WC. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001; 345:790–797. PMID:
11556298.

24. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003; 289:76–79. PMID:
12503980.

25. Ajani UA, Hennekens CH, Spelsberg A, Manson JE. Alcohol consumption and risk of type 2 diabetes mellitus among US male physicians. Arch Intern Med. 2000; 160:1025–1030. PMID:
10761969.

26. Davies MJ, Baer DJ, Judd JT, Brown ED, Campbell WS, Taylor PR. Effects of moderate alcohol intake on fasting insulin and glucose concentrations and insulin sensitivity in postmenopausal women: a randomized controlled trial. JAMA. 2002; 287:2559–2562. PMID:
12020337.
27. Seike N, Noda M, Kadowaki T. Alcohol consumption and risk of type 2 diabetes mellitus in Japanese: a systematic review. Asia Pac J Clin Nutr. 2008; 17:545–551. PMID:
19114388.
28. Lee DY, Yoo MG, Kim HJ, Jang HB, Kim JH, Lee HJ, Park SI. Association between alcohol consumption pattern and the incidence risk of type 2 diabetes in Korean men: a 12-years follow-up study. Sci Rep. 2017; 7:7322. PMID:
28779170.

29. Kim JY, Lee DY, Lee YJ, Park KJ, Kim KH, Kim JW, Kim WH. Chronic alcohol consumption potentiates the development of diabetes through pancreatic β-cell dysfunction. World J Biol Chem. 2015; 6:1–15. PMID:
25717351.

30. Min S, Noh S, Shin J, Ahn JS, Kim TH. Alcohol dependence, mortality, and chronic health conditions in a rural population in Korea. J Korean Med Sci. 2008; 23:1–9. PMID:
18303191.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download