INTRODUCTION
To date, numerous preclinical and preliminary clinical evaluations have consistently indicated the potential cardiovascular (CV) benefits of glucagon-like peptide 1 receptor agonists (GLP-1 RAs) [
12]. In addition, the results of three cardiovascular outcome trials (CVOTs) assessing the safety of long-acting GLP-1 RAs have been reported. The Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results (LEADER) study [
3], and the Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN-6) study [
4], not only demonstrated CV safety, but also demonstrated the superiority of liraglutide and semaglutide versus placebo in reducing the risk of cardiovascular disease (CVD). On the contrary, the Exenatide Study of Cardiovascular Event Lowering Trial (EXSCEL) study [
5] demonstrated the CV safety of weekly exenatide but no statistically significant additional CV benefit was seen compared with placebo treatment [
5].
We have conducted a pooled analysis to assess the CV effects of long-acting GLP-1 RAs with a special emphasis on subpopulations in order to find hints as to subgroups experiencing greater of reduced benefits from treatment with long-acting GLP-1 RAs.
RESULTS
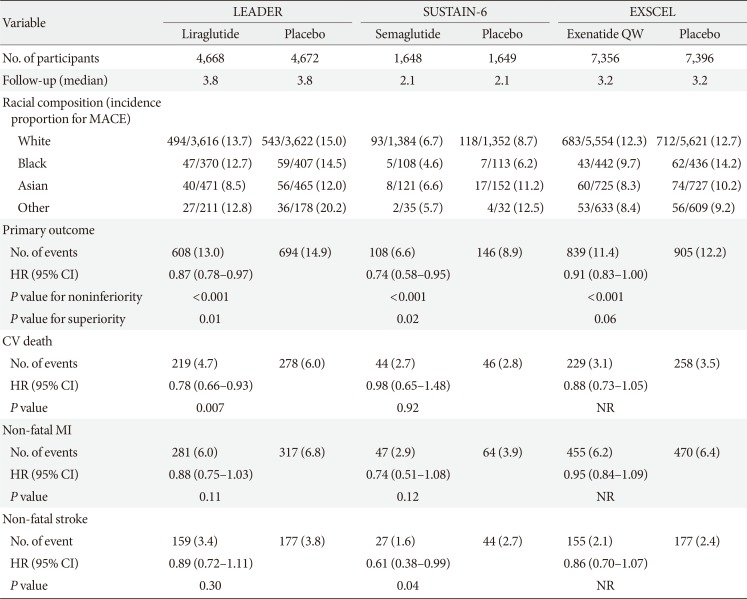
The main results of each CVOT are presented in
Table 1 and the detailed study design, baseline clinical and biochemical characteristics are summarized in
Supplementary Table 1. The EXSCEL study enrolled the largest number of subjects, whereas SUSTAIN-6 enrolled the smallest number of participants with the shortest median follow-up duration. Higher male-to-female participant ratios were observed in all three studies; SUSTAIN-6 had the greatest proportion of female subjects. Participants from various geographic regions were enrolled throughout all three studies, although most patients were from a white racial background.
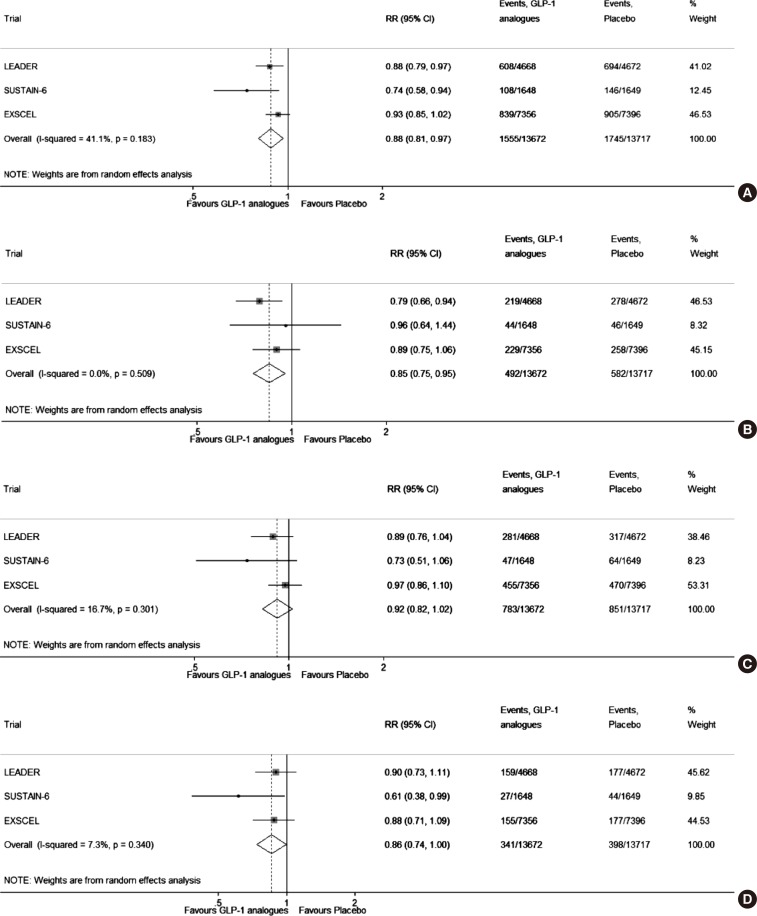
The composite analysis of risk of MACE is illustrated in
Fig. 1. Moderate heterogeneity among the published trials was observed (
I2=41.1%,
P=0.183). Although the reduction in risk of MACE observed in the EXSCEL trial did not reach statistical significance as a single study, the combined analysis of all three CVOTs revealed statistically significant MACE risk reductions (relative risk [RR], 0.88; 95% CI, 0.81 to 0.97) (
Fig. 1A). The combined reduction in RR for CV death was also statistically significant (RR, 0.85; 95% CI, 0.75 to 0.95) (
Fig. 1B). However, the combined analysis of risk reduction in non-fatal MI and stroke did not reach statistical significance (
Fig. 1C and D, respectively).
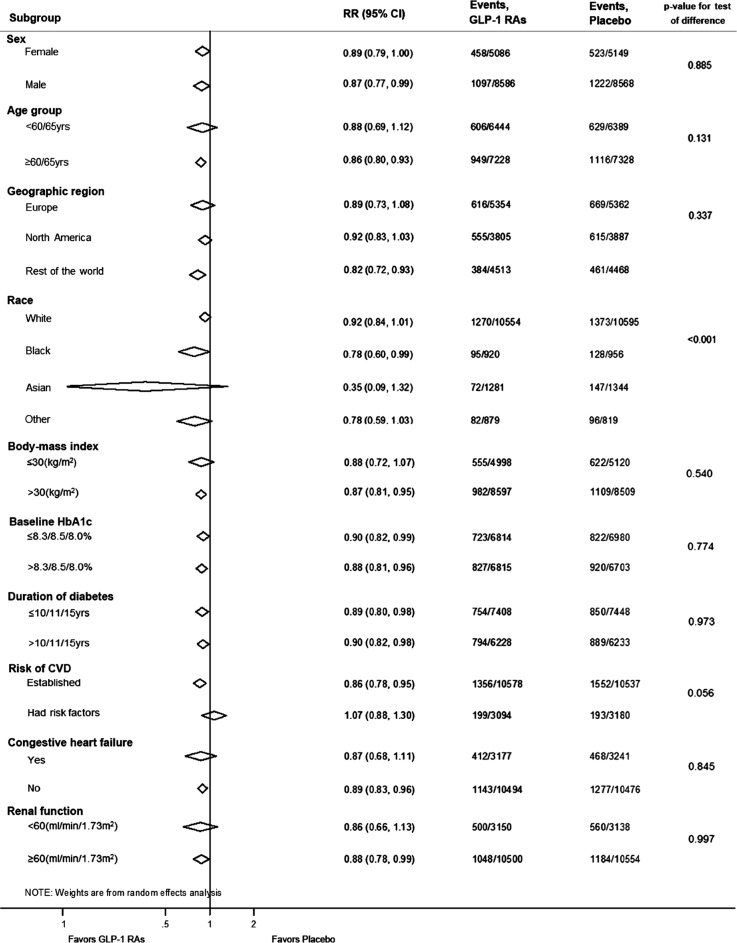
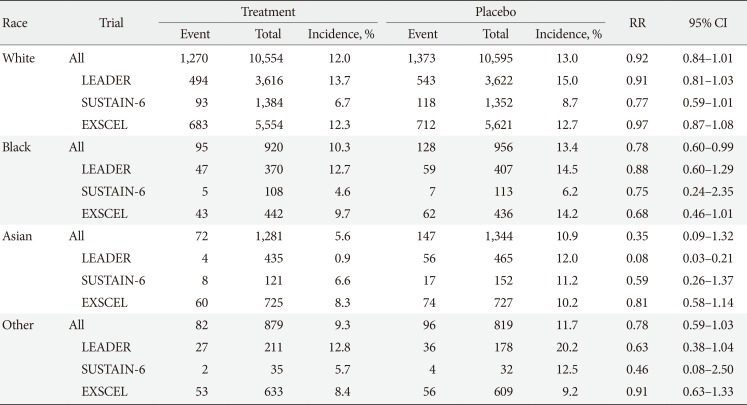
Fig. 2 presents the combined subgroup analysis of the three CVOTs. All subgroups, with the exception of race, showed no statistically significant difference compared with parameters within the same category (i.e.,
P<0.001 for the test of racial difference). Evaluation of patients on the basis of race showed trends of MACE risk reductions in subjects of Black race (RR, 0.78; 95% CI, 0.60 to 0.99) and Asians (RR, 0.35; 95% CI, 0.09 to 1.32]) (
Table 2), but
post hoc analysis using Bonferroni method revealed that only Asians exhibited a significantly greater CV benefit from long-acting GLP-1 RAs, compared with white subjects (
P<0.0001) (
Supplementary Table 2). In addition, subjects with established CVD showed a significant MACE risk reduction (RR, 0.86; 95% CI, 0.78 to 0.95), although those who had CV risks without established CVD did not show significant risk reductions (RR, 1.07; 95% CI, 0.88 to 1.30), albeit statistically nonsignificant
P value for test of interaction (
P=0.056).
To determine the contributing factors that might have led to a favorable CV outcome, CV risk factors from the three CVOTs were analyzed (
Supplementary Fig. 1). All three CVOTs demonstrated significant reductions in HbA1c, systolic blood pressure (SBP), body weight, and heart rate. Combined analysis of these CV risk factors revealed that the overall mean difference in HbA1c in all three CVOTs was −0.65% (95% CI, −0.83 to −0.47) (
Supplementary Fig. 1A). The combined analysis also revealed overall SBP change of −1.5 mm Hg (95% CI, −1.83 to −1.23) (
Supplementary Fig. 1B). The overall body weight change was −2.67 kg (95% CI, −3.74 to −1.59) (
Supplementary Fig. 1C) and the overall change in heart rate was 2.60 bpm (95% CI, 2.26 to 2.94) (
Supplementary Fig. 1D).
DISCUSSION
In line with the recent meta-analysis that observed significantly reduced three-point MACE and mortality with the use of GLP-1 RAs (including the short-acting GLP-1 RA lixisenatide) [
5], the overall results of our combined analysis that exclusively analyzed three CVOTs on long-acting GLP-1 RAs showed the reduced risk of three-point MACE and CV mortality. Of note, our subgroup analysis revealed a differential CV benefit of GLP-1 RAs across ethnic groups with a favorable trend towards Asians.
The mechanisms behind the cardioprotective effect of GLP-1 RAs have been well established in preclinical and clinical studies [
12]. Also as shown in
Supplementary Fig. 1, GLP-1 RAs improve cardiometabolic factors such as HbA1c, SBP, and body weight [
345], and this could have contributed to the overall CV superiority observed in this combined analysis. In addition, abundant GLP-1 receptor expression in cardiac and vascular tissues and the direct effect of GLP-1 to the CV system such as the enhanced endothelial function, ventricular contractility, and myocardial glucose uptake could have contributed simultaneously [
12]. Taken together, the aforementioned direct and indirect effects of GLP-1 RAs might be responsible for the overall risk reduction for MACE [
1].
To our knowledge, this is the first study that showed a statistically meaningful difference in the CV outcome among various racial groups. Although the RR for three-point MACE among Asians did not meet its statistical significance, its favorable trend, as well as the significant
post hoc analysis result, indicate a probably greater CV benefit from the long-acting GLP-1 RAs in Asian subpopulations with type 2 diabetes mellitus, compared with other racial groups (
Supplementary Table 2). Although mechanisms underlying the cardioprotective effect of GLP-1 RAs is sufficiently established, those explaining the differential CV benefit according to race remains unclear. However, there are several previous study findings which we can relate to this phenomenon.
First, Asians, especially East Asians, tend to exhibit lower intact GLP-1 levels whether they are healthy or diabetic [
67]. Impaired GLP-1 secretion, as well as accelerated degradation of endogenous GLP-1 by enhanced dipeptidyl peptidase-4 (DPP-4) among Asians have been proposed to explain the lower GLP-1 levels observed in Asian subjects [
8]. Moreover, a Japanese study observed a blunted post-meal GLP-1 response in people with diabetes [
7]. Therefore, potential metabolic consequences caused by considerably lower total GLP-1 levels and blunted GLP-1 responses might have been compensated for by the exogenous GLP-1 RA administration, exerting more profound GLP-1 effects in the whole body, including the CV system. Second, the preventive effect against CVD could be explained by a greater improvement, by GLP-1 receptor stimulation, in the cardiometabolic risk factor profile in Asian subjects. For example, better glycemic control with incretin-based therapies in Asian type 2 diabetes mellitus patients than in other racial groups has been suggested [
91011]. Kim et al. [
910] ran a series of meta-analyses and observed that DPP-4 inhibitors [
9] and GLP-1 analogues [
10] lead to a significantly greater HbA1c reduction in Asian-dominant studies (i.e., ≥50% Asian participants) than in non-Asian dominant studies (i.e., <50% Asian participants). Suggested mechanisms underlying the greater glucose-lowering efficacy of GLP-1 RAs among Asians may include more profound β-cell dysfunction, genetic factors, a different nutritional composition that might lead to a different incretin response, and a lower BMI (i.e., BMI threshold hypothesis) [
11]. Because Asians exhibit metabolic deterioration at a lower BMI compared to other racial counterparts, the net weight loss achieved by GLP-1 RAs administration could have a significantly greater metabolic impact on the Asian population. Also, with a lower body size and volume of distribution, Asians might be exposed to a higher level of GLP-1 RAs. All of the aforementioned study findings could explain the additional CV benefit from GLP-1 RAs to some extent, however, their actual association with respect to ethnicity, as well as other possible mechanisms should still be investigated in the future comparative studies.
The main limitation of the current study is the possibility of a selection bias attributable to a highly selective study design that recruited several, currently available trial results with CV events as the primary endpoint. Moreover, subjects enrolled in these studies had diabetes and a high risk of CVD and therefore are not representative of patients in ambulatory diabetes care. However, as a result of randomization, the background antidiabetic drugs might have balanced between the treatment and placebo groups. Second, the CVOTs published to date mostly investigated the CV effect of long-acting GLP-1 as a secondary prevention of CVD for efficient study designs. Future studies should validate the effectiveness and utilization of GLP-1 RAs as a primary prevention of CVD. Lastly, because patient-level data were currently unavailable from the included studies, the statistical limitations owing to a small number of Asians enrolled in the CVOTs as well as the lack of other endpoints besides the MACE (e.g., cholesterol levels) or the incidence of established CVDs were inevitable. However, we ran a post hoc analysis using Bonferroni method to delineate the difference among all racial groups. The low proportion of Asian subjects in included studies might also be responsible for the lack of statistical power in our analysis. Therefore, the existence of a racial difference in the CV benefit, as well as potential mechanisms, should be investigated in future studies.
In conclusion, combining data from the major CVOTs of long-acting GLP-1 RAs (i.e., liraglutide, semaglutide, and weekly exenatide), we observed an overall CV superiority of these treatments over placebo, as well as the racial difference in the reduced risk for the three-point MACE. A favorable trend in CV outcomes towards Asians compared to other racial groups in our study should be furthermore validated by future studies with patient-level data to define these observations as a class effect, and evaluation of potential mechanisms underlying differential CV benefits across racial groups is also necessitated. If so, long-acting GLP-1 RAs might be a preferred choice for Asian type 2 diabetes mellitus patients, especially those with established CVDs.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download