1. Bluestone JA, Herold K, Eisenbarth G. Genetics, pathogenesis and clinical interventions in type 1 diabetes. Nature. 2010; 464:1293–1300. PMID:
20432533.
2. Mishra R, Hodge KM, Cousminer DL, Leslie RD, Grant SFA. A global perspective of latent autoimmune diabetes in adults. Trends Endocrinol Metab. 2018; 29:638–650. PMID:
30041834.

3. Tuomi T, Groop LC, Zimmet PZ, Rowley MJ, Knowles W, Mackay IR. Antibodies to glutamic acid decarboxylase reveal latent autoimmune diabetes mellitus in adults with a non-insulin-dependent onset of disease. Diabetes. 1993; 42:359–362. PMID:
8425674.

4. Hawa MI, Kolb H, Schloot N, Beyan H, Paschou SA, Buzzetti R, Mauricio D, De Leiva A, Yderstraede K, Beck-Neilsen H, Tuomilehto J, Sarti C, Thivolet C, Hadden D, Hunter S, Schernthaner G, Scherbaum WA, Williams R, Brophy S, Pozzilli P, Leslie RD. Action LADA consortium. Adult-onset autoimmune diabetes in Europe is prevalent with a broad clinical phenotype: Action LADA 7. Diabetes Care. 2013; 36:908–913. PMID:
23248199.
5. Maddaloni E, Lessan N, Al Tikriti A, Buzzetti R, Pozzilli P, Barakat MT. Latent autoimmune diabetes in adults in the United Arab Emirates: clinical features and factors related to insulin-requirement. PLoS One. 2015; 10:e0131837. PMID:
26252955.

6. Pozzilli P, Di Mario U. Autoimmune diabetes not requiring insulin at diagnosis (latent autoimmune diabetes of the adult): definition, characterization, and potential prevention. Diabetes Care. 2001; 24:1460–1467. PMID:
11473087.
7. American Diabetes Association. (2) Classification and diagnosis of diabetes. Diabetes Care. 2015; 38(Suppl):S8–S16.
8. Leslie RD, Williams R, Pozzilli P. Clinical review: type 1 diabetes and latent autoimmune diabetes in adults: one end of the rainbow. J Clin Endocrinol Metab. 2006; 91:1654–1659. PMID:
16478821.
9. Kobayashi T, Nakanishi K, Murase T, Kosaka K. Small doses of subcutaneous insulin as a strategy for preventing slowly progressive beta-cell failure in islet cell antibody-positive patients with clinical features of NIDDM. Diabetes. 1996; 45:622–626. PMID:
8621013.

10. Yasui J, Kawasaki E, Tanaka S, Awata T, Ikegami H, Imagawa A, Uchigata Y, Osawa H, Kajio H, Kawabata Y, Shimada A, Takahashi K, Yasuda K, Yasuda H, Hanafusa T, Kobayashi T. Japan Diabetes Society Committee on Type 1 Diabetes Mellitus Research. Clinical and genetic characteristics of non-insulin-requiring glutamic acid decarboxylase (GAD) autoantibody-positive diabetes: a nationwide survey in Japan. PLoS One. 2016; 11:e0155643. PMID:
27177031.

11. Sabbah E, Savola K, Ebeling T, Kulmala P, Vahasalo P, Ilonen J, Salmela PI, Knip M. Genetic, autoimmune, and clinical characteristics of childhood- and adult-onset type 1 diabetes. Diabetes Care. 2000; 23:1326–1332. PMID:
10977027.

12. Howson JM, Rosinger S, Smyth DJ, Boehm BO. ADBW-END Study Group. Todd JA. Genetic analysis of adult-onset autoimmune diabetes. Diabetes. 2011; 60:2645–2653. PMID:
21873553.

13. Hernandez M, Mollo A, Marsal JR, Esquerda A, Capel I, Puig-Domingo M, Pozzilli P, de Leiva A, Mauricio D. Action LADA consortium. Insulin secretion in patients with latent autoimmune diabetes (LADA): half way between type 1 and type 2 diabetes: action LADA 9. BMC Endocr Disord. 2015; 15:1. PMID:
25572256.

14. Park Y, Wintergerst KA, Zhou Z. Clinical heterogeneity of type 1 diabetes (T1D) found in Asia. Diabetes Metab Res Rev. 2017; 33:e2907.

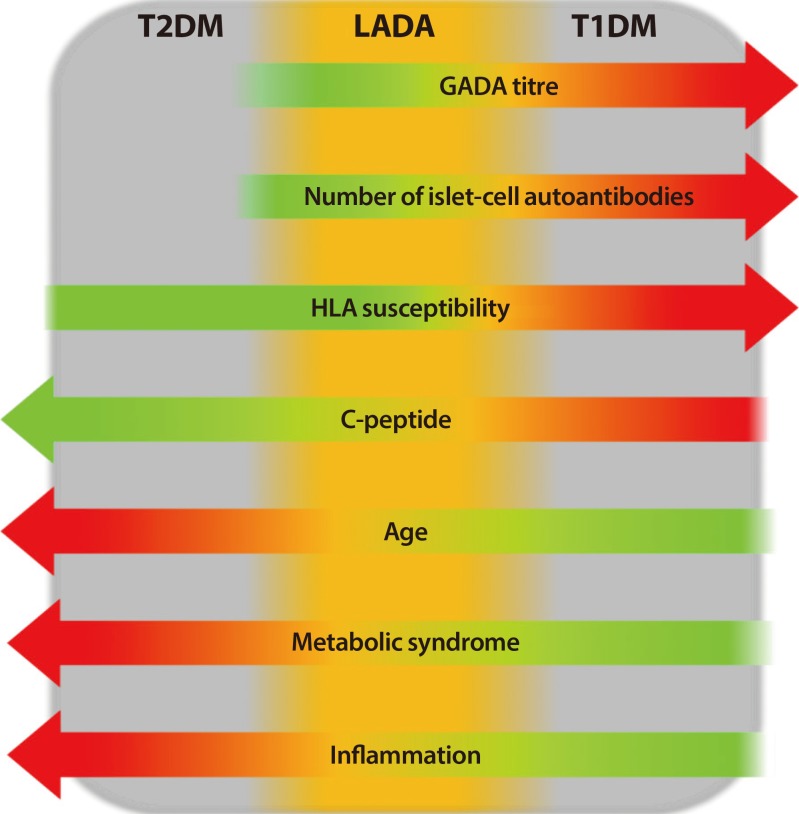
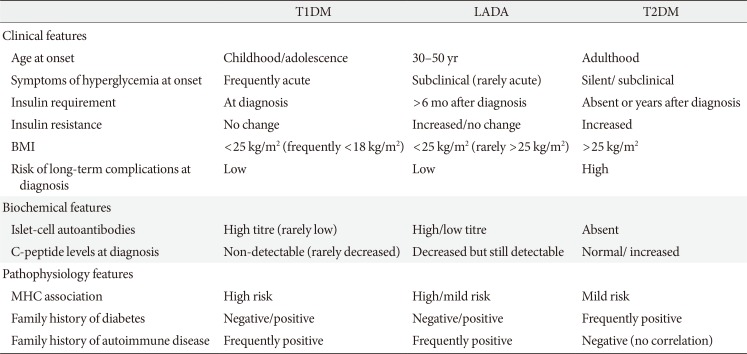
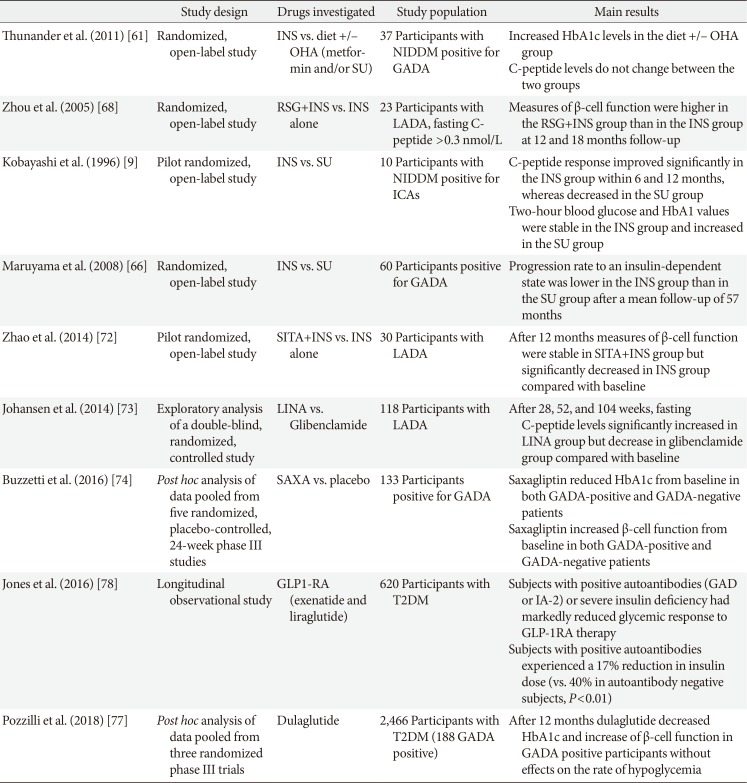
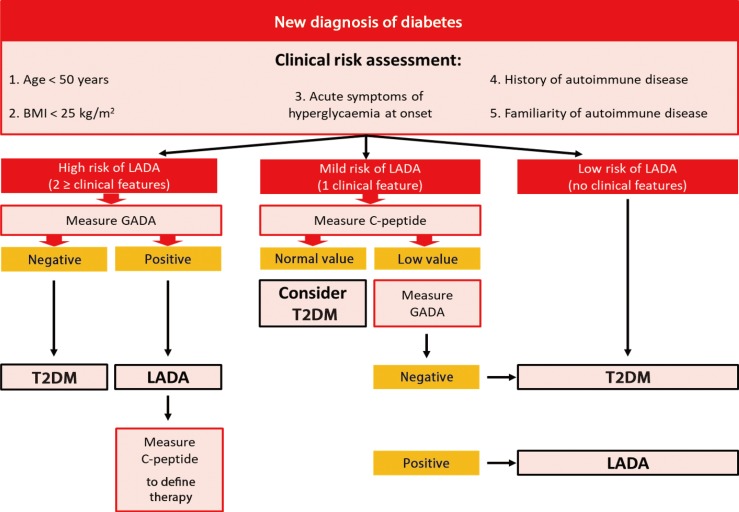
15. Buzzetti R, Zampetti S, Maddaloni E. Adult-onset autoimmune diabetes: current knowledge and implications for management. Nat Rev Endocrinol. 2017; 13:674–686. PMID:
28885622.

16. Fourlanos S, Dotta F, Greenbaum CJ, Palmer JP, Rolandsson O, Colman PG, Harrison LC. Latent autoimmune diabetes in adults (LADA) should be less latent. Diabetologia. 2005; 48:2206–2212. PMID:
16193284.

17. Maioli M, Pes GM, Delitala G, Puddu L, Falorni A, Tolu F, Lampis R, Orrù V, Secchi G, Cicalo AM, Floris R, Madau GF, Pilosu RM, Whalen M, Cucca F. Number of autoantibodies and HLA genotype, more than high titers of glutamic acid decarboxylase autoantibodies, predict insulin dependence in latent autoimmune diabetes of adults. Eur J Endocrinol. 2010; 163:541–549. PMID:
20603341.

18. Roh MO, Jung CH, Kim BY, Mok JO, Kim CH. The prevalence and characteristics of latent autoimmune diabetes in adults (LADA) and its relation with chronic complications in a clinical department of a university hospital in Korea. Acta Diabetol. 2013; 50:129–134. PMID:
20953640.

19. Naik RG, Brooks-Worrell BM, Palmer JP. Latent autoimmune diabetes in adults. J Clin Endocrinol Metab. 2009; 94:4635–4644. PMID:
19837918.

20. Buzzetti R, Di Pietro S, Giaccari A, Petrone A, Locatelli M, Suraci C, Capizzi M, Arpi ML, Bazzigaluppi E, Dotta F, Bosi E. Non Insulin Requiring Autoimmune Diabetes Study Group. High titer of autoantibodies to GAD identifies a specific phenotype of adult-onset autoimmune diabetes. Diabetes Care. 2007; 30:932–938. PMID:
17392553.

21. Radtke MA, Midthjell K, Nilsen TI, Grill V. Heterogeneity of patients with latent autoimmune diabetes in adults: linkage to autoimmunity is apparent only in those with perceived need for insulin treatment: results from the Nord-Trondelag Health (HUNT) study. Diabetes Care. 2009; 32:245–250. PMID:
19001190.
22. Park Y, Hong S, Park L, Woo J, Baik S, Nam M, Lee K, Kim Y. KNDP collaboratory Group. LADA prevalence estimation and insulin dependency during follow-up. Diabetes Metab Res Rev. 2011; 27:975–979. PMID:
22069296.

23. Bruno G, Runzo C, Cavallo-Perin P, Merletti F, Rivetti M, Pinach S, Novelli G, Trovati M, Cerutti F, Pagano G. Piedmont Study Group for Diabetes Epidemiology. Incidence of type 1 and type 2 diabetes in adults aged 30–49 years: the population-based registry in the province of Turin, Italy. Diabetes Care. 2005; 28:2613–2619. PMID:
16249528.
24. Rawshani A, Landin-Olsson M, Svensson AM, Nystrom L, Arnqvist HJ, Bolinder J, Gudbjornsdottir S. The incidence of diabetes among 0–34 year olds in Sweden: new data and better methods. Diabetologia. 2014; 57:1375–1381. PMID:
24710965.
25. Turner R, Stratton I, Horton V, Manley S, Zimmet P, Mackay IR, Shattock M, Bottazzo GF, Holman R. UKPDS 25: autoantibodies to islet-cell cytoplasm and glutamic acid decarboxylase for prediction of insulin requirement in type 2 diabetes. UK Prospective Diabetes Study Group. Lancet. 1997; 350:1288–1293. PMID:
9357409.
26. Tuomi T, Carlsson A, Li H, Isomaa B, Miettinen A, Nilsson A, Nissen M, Ehrnstrom BO, Forsen B, Snickars B, Lahti K, Forsblom C, Saloranta C, Taskinen MR, Groop LC. Clinical and genetic characteristics of type 2 diabetes with and without GAD antibodies. Diabetes. 1999; 48:150–157. PMID:
9892237.

27. Takeda H, Kawasaki E, Shimizu I, Konoue E, Fujiyama M, Murao S, Tanaka K, Mori K, Tarumi Y, Seto I, Fujii Y, Kato K, Kondo S, Takada Y, Kitsuki N, Kaino Y, Kida K, Hashimoto N, Yamane Y, Yamawaki T, Onuma H, Nishimiya T, Osawa H, Saito Y, Makino H. Ehime Study. Clinical, autoimmune, and genetic characteristics of adult-onset diabetic patients with GAD autoantibodies in Japan (Ehime Study). Diabetes Care. 2002; 25:995–1001. PMID:
12032105.

28. Zinman B, Kahn SE, Haffner SM, O'Neill MC, Heise MA, Freed MI. ADOPT Study Group. Phenotypic characteristics of GAD antibody-positive recently diagnosed patients with type 2 diabetes in North America and Europe. Diabetes. 2004; 53:3193–3200. PMID:
15561950.

29. Qi X, Sun J, Wang J, Wang PP, Xu Z, Murphy M, Jia J, Wang J, Xie Y, Xu W. Prevalence and correlates of latent autoimmune diabetes in adults in Tianjin, China: a population-based cross-sectional study. Diabetes Care. 2011; 34:66–70. PMID:
20876205.
30. Lee SH, Kwon HS, Yoo SJ, Ahn YB, Yoon KH, Cha BY, Lee KW, Son HY. Identifying latent autoimmune diabetes in adults in Korea: the role of C-peptide and metabolic syndrome. Diabetes Res Clin Pract. 2009; 83:e62–e65. PMID:
19166794.

31. Britten AC, Jones K, Torn C, Hillman M, Ekholm B, Kumar S, Barnett AH, Kelly MA. Latent autoimmune diabetes in adults in a South Asian population of the U.K. Diabetes Care. 2007; 30:3088–3090. PMID:
17878244.

32. Sachan A, Zaidi G, Sahu RP, Agrawal S, Colman PG, Bhatia E. Low prevalence of latent autoimmune diabetes in adults in northern India. Diabet Med. 2015; 32:810–813. PMID:
25444459.

33. Zhou Z, Xiang Y, Ji L, Jia W, Ning G, Huang G, Yang L, Lin J, Liu Z, Hagopian WA, Leslie RD. LADA China Study Group. Frequency, immunogenetics, and clinical characteristics of latent autoimmune diabetes in China (LADA China study): a nationwide, multicenter, clinic-based cross-sectional study. Diabetes. 2013; 62:543–550. PMID:
23086039.
34. Haller K, Kisand K, Pisarev H, Salur L, Laisk T, Nemvalts V, Uibo R. Insulin gene VNTR, CTLA-4 +49A/G and HLA-DQB1 alleles distinguish latent autoimmune diabetes in adults from type 1 diabetes and from type 2 diabetes group. Tissue Antigens. 2007; 69:121–127. PMID:
17257313.

35. Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J, Helgason A, Stefansson H, Emilsson V, Helgadottir A, Styrkarsdottir U, Magnusson KP, Walters GB, Palsdottir E, Jonsdottir T, Gudmundsdottir T, Gylfason A, Saemundsdottir J, Wilensky RL, Reilly MP, Rader DJ, Bagger Y, Christiansen C, Gudnason V, Sigurdsson G, Thorsteinsdottir U, Gulcher JR, Kong A, Stefansson K. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet. 2006; 38:320–323. PMID:
16415884.

36. Field SF, Howson JM, Smyth DJ, Walker NM, Dunger DB, Todd JA. Analysis of the type 2 diabetes gene, TCF7L2, in 13,795 type 1 diabetes cases and control subjects. Diabetologia. 2007; 50:212–213. PMID:
17063324.

37. Qu HQ, Grant SF, Bradfield JP, Kim C, Frackelton E, Hakonarson H, Polychronakos C. Association analysis of type 2 diabetes Loci in type 1 diabetes. Diabetes. 2008; 57:1983–1986. PMID:
18426861.

38. Desai M, Zeggini E, Horton VA, Owen KR, Hattersley AT, Levy JC, Walker M, Gillespie KM, Bingley PJ, Hitman GA, Holman RR, McCarthy MI, Clark A. An association analysis of the HLA gene region in latent autoimmune diabetes in adults. Diabetologia. 2007; 50:68–73. PMID:
17143607.

39. Andersen MK, Lundgren V, Turunen JA, Forsblom C, Isomaa B, Groop PH, Groop L, Tuomi T. Latent autoimmune diabetes in adults differs genetically from classical type 1 diabetes diagnosed after the age of 35 years. Diabetes Care. 2010; 33:2062–2064. PMID:
20805278.

40. Barinas-Mitchell E, Pietropaolo S, Zhang YJ, Henderson T, Trucco M, Kuller LH, Pietropaolo M. Islet cell autoimmunity in a triethnic adult population of the Third National Health and Nutrition Examination Survey. Diabetes. 2004; 53:1293–1302. PMID:
15111499.

41. Yang Z, Wang K, Li T, Sun W, Li Y, Chang YF, Dorman JS, LaPorte RE. Childhood diabetes in China. Enormous variation by place and ethnic group. Diabetes Care. 1998; 21:525–529. PMID:
9571336.

42. Barker A, Lauria A, Schloot N, Hosszufalusi N, Ludvigsson J, Mathieu C, Mauricio D, Nordwall M, Van der Schueren B, Mandrup-Poulsen T, Scherbaum WA, Weets I, Gorus FK, Wareham N, Leslie RD, Pozzilli P. Age-dependent decline of β-cell function in type 1 diabetes after diagnosis: a multi-centre longitudinal study. Diabetes Obes Metab. 2014; 16:262–267. PMID:
24118704.

43. Lampasona V, Petrone A, Tiberti C, Capizzi M, Spoletini M, di Pietro S, Songini M, Bonicchio S, Giorgino F, Bonifacio E, Bosi E, Buzzetti R. Non Insulin Requiring Autoimmune Diabetes (NIRAD) Study Group. Zinc transporter 8 antibodies complement GAD and IA-2 antibodies in the identification and characterization of adult-onset autoimmune diabetes: Non Insulin Requiring Autoimmune Diabetes (NIRAD) 4. Diabetes Care. 2010; 33:104–108. PMID:
19808923.
44. Tiberti C, Giordano C, Locatelli M, Bosi E, Bottazzo GF, Buzzetti R, Cucinotta D, Galluzzo A, Falorni A, Dotta F. Identification of tyrosine phosphatase 2(256-760) construct as a new, sensitive marker for the detection of islet autoimmunity in type 2 diabetic patients: the non-insulin requiring autoimmune diabetes (NIRAD) study 2. Diabetes. 2008; 57:1276–1283. PMID:
18332100.
45. Buzzetti R, Spoletini M, Zampetti S, Campagna G, Marandola L, Panimolle F, Dotta F, Tiberti C. NIRAD Study Group (NIRAD 8). Tyrosine phosphatase-related islet antigen 2(256-760) autoantibodies, the only marker of islet autoimmunity that increases by increasing the degree of BMI in obese subjects with type 2 diabetes. Diabetes Care. 2015; 38:513–520. PMID:
25567348.
46. Hawa MI, Thivolet C, Mauricio D, Alemanno I, Cipponeri E, Collier D, Hunter S, Buzzetti R, de Leiva A, Pozzilli P, Leslie RD. Action LADA Group. Metabolic syndrome and autoimmune diabetes: action LADA 3. Diabetes Care. 2009; 32:160–164. PMID:
18945926.

47. Hjort R, Ahlqvist E, Carlsson PO, Grill V, Groop L, Martinell M, Rasouli B, Rosengren A, Tuomi T, Asvold BO, Carlsson S. Overweight, obesity and the risk of LADA: results from a Swedish case-control study and the Norwegian HUNT Study. Diabetologia. 2018; 61:1333–1343. PMID:
29589073.

48. Leslie RD, Kolb H, Schloot NC, Buzzetti R, Mauricio D, De Leiva A, Yderstraede K, Sarti C, Thivolet C, Hadden D, Hunter S, Schernthaner G, Scherbaum W, Williams R, Pozzilli P. Diabetes classification: grey zones, sound and smoke: Action LADA 1. Diabetes Metab Res Rev. 2008; 24:511–519. PMID:
18615859.

49. Zampetti S, Capizzi M, Spoletini M, Campagna G, Leto G, Cipolloni L, Tiberti C, Bosi E, Falorni A, Buzzetti R. NIRAD Study Group. GADA titer-related risk for organ-specific autoimmunity in LADA subjects subdivided according to gender (NIRAD study 6). J Clin Endocrinol Metab. 2012; 97:3759–3765. PMID:
22865904.

50. Genovese S, Bazzigaluppi E, Goncalves D, Ciucci A, Cavallo MG, Purrello F, Anello M, Rotella CM, Bardini G, Vaccaro O, Riccardi G, Travaglini P, Morenghi E, Bosi E, Pozzilli P. Clinical phenotype and beta-cell autoimmunity in Italian patients with adult-onset diabetes. Eur J Endocrinol. 2006; 154:441–447. PMID:
16498058.
51. Desai M, Cull CA, Horton VA, Christie MR, Bonifacio E, Lampasona V, Bingley PJ, Levy JC, Mackay IR, Zimmet P, Holman RR, Clark A. GAD autoantibodies and epitope reactivities persist after diagnosis in latent autoimmune diabetes in adults but do not predict disease progression: UKPDS 77. Diabetologia. 2007; 50:2052–2060. PMID:
17657474.

52. Fourlanos S, Perry C, Stein MS, Stankovich J, Harrison LC, Colman PG. A clinical screening tool identifies autoimmune diabetes in adults. Diabetes Care. 2006; 29:970–975. PMID:
16644622.

53. Monge L, Bruno G, Pinach S, Grassi G, Maghenzani G, Dani F, Pagano G. A clinically orientated approach increases the efficiency of screening for latent autoimmune diabetes in adults (LADA) in a large clinic-based cohort of patients with diabetes onset over 50 years. Diabet Med. 2004; 21:456–459. PMID:
15089790.

54. Davis AK, DuBose SN, Haller MJ, Miller KM, DiMeglio LA, Bethin KE, Goland RS, Greenberg EM, Liljenquist DR, Ahmann AJ, Marcovina SM, Peters AL, Beck RW, Greenbaum CJ. T1D Exchange Clinic Network. Prevalence of detectable C-Peptide according to age at diagnosis and duration of type 1 diabetes. Diabetes Care. 2015; 38:476–481. PMID:
25519448.

55. Pipi E, Marketou M, Tsirogianni A. Distinct clinical and laboratory characteristics of latent autoimmune diabetes in adults in relation to type 1 and type 2 diabetes mellitus. World J Diabetes. 2014; 5:505–510. PMID:
25126396.

56. Bell DS, Ovalle F. The role of C-peptide levels in screening for latent autoimmune diabetes in adults. Am J Ther. 2004; 11:308–311. PMID:
15266224.

57. Zampetti S, Campagna G, Tiberti C, Songini M, Arpi ML, De Simone G, Cossu E, Cocco L, Osborn J, Bosi E, Giorgino F, Spoletini M, Buzzetti R. NIRAD Study Group. High GADA titer increases the risk of insulin requirement in LADA patients: a 7-year follow-up (NIRAD study 7). Eur J Endocrinol. 2014; 171:697–704. PMID:
25213702.

58. Argoud GM, Schade DS, Eaton RP. Insulin suppresses its own secretion in vivo. Diabetes. 1987; 36:959–962. PMID:
3297890.

59. Jansen A, Rosmalen JG, Homo-Delarche F, Dardenne M, Drexhage HA. Effect of prophylactic insulin treatment on the number of ER-MP23+ macrophages in the pancreas of NOD mice. Is the prevention of diabetes based on beta-cell rest? J Autoimmun. 1996; 9:341–348. PMID:
8816969.
60. Steffes MW, Sibley S, Jackson M, Thomas W. Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care. 2003; 26:832–836. PMID:
12610045.
61. Thunander M, Thorgeirsson H, Torn C, Petersson C, Landin-Olsson M. β-Cell function and metabolic control in latent autoimmune diabetes in adults with early insulin versus conventional treatment: a 3-year follow-up. Eur J Endocrinol. 2011; 164:239–245. PMID:
21088056.

62. Fuchtenbusch M, Kredel K, Bonifacio E, Schnell O, Ziegler AG. Exposure to exogenous insulin promotes IgG1 and the T-helper 2-associated IgG4 responses to insulin but not to other islet autoantigens. Diabetes. 2000; 49:918–925. PMID:
10866043.
63. Tiittanen M, Huupponen JT, Knip M, Vaarala O. Insulin treatment in patients with type 1 diabetes induces upregulation of regulatory T-cell markers in peripheral blood mononuclear cells stimulated with insulin in vitro. Diabetes. 2006; 55:3446–3454. PMID:
17130491.

64. Schloot N, Eisenbarth GS. Isohormonal therapy of endocrine autoimmunity. Immunol Today. 1995; 16:289–294. PMID:
7662098.

65. Brophy S, Davies H, Mannan S, Brunt H, Williams R. Interventions for latent autoimmune diabetes (LADA) in adults. Cochrane Database Syst Rev. 2011; (9):CD006165. PMID:
21901702.

66. Maruyama T, Tanaka S, Shimada A, Funae O, Kasuga A, Kanatsuka A, Takei I, Yamada S, Harii N, Shimura H, Kobayashi T. Insulin intervention in slowly progressive insulin-dependent (type 1) diabetes mellitus. J Clin Endocrinol Metab. 2008; 93:2115–2121. PMID:
18397986.

67. George P, McCrimmon RJ. Potential role of non-insulin adjunct therapy in type 1 diabetes. Diabet Med. 2013; 30:179–188. PMID:
22804102.
68. Zhou Z, Li X, Huang G, Peng J, Yang L, Yan X, Wang J. Rosiglitazone combined with insulin preserves islet beta cell function in adult-onset latent autoimmune diabetes (LADA). Diabetes Metab Res Rev. 2005; 21:203–208. PMID:
15386806.
69. D'Alessio DA, Denney AM, Hermiller LM, Prigeon RL, Martin JM, Tharp WG, Saylan ML, He Y, Dunning BE, Foley JE, Pratley RE. Treatment with the dipeptidyl peptidase-4 inhibitor vildagliptin improves fasting islet-cell function in subjects with type 2 diabetes. J Clin Endocrinol Metab. 2009; 94:81–88. PMID:
18957505.
70. Foley JE, Bunck MC, Moller-Goede DL, Poelma M, Nijpels G, Eekhoff EM, Schweizer A, Heine RJ, Diamant M. Beta cell function following 1 year vildagliptin or placebo treatment and after 12 week washout in drug-naïve patients with type 2 diabetes and mild hyperglycaemia: a randomised controlled trial. Diabetologia. 2011; 54:1985–1991. PMID:
21547496.
71. Tian L, Gao J, Hao J, Zhang Y, Yi H, O'Brien TD, Sorenson R, Luo J, Guo Z. Reversal of new-onset diabetes through modulating inflammation and stimulating beta-cell replication in nonobese diabetic mice by a dipeptidyl peptidase IV inhibitor. Endocrinology. 2010; 151:3049–3060. PMID:
20444936.
72. Zhao Y, Yang L, Xiang Y, Liu L, Huang G, Long Z, Li X, Leslie RD, Wang X, Zhou Z. Dipeptidyl peptidase 4 inhibitor sitagliptin maintains β-cell function in patients with recent-onset latent autoimmune diabetes in adults: one year prospective study. J Clin Endocrinol Metab. 2014; 99:E876–E880. PMID:
24432999.

73. Johansen OE, Boehm BO, Grill V, Torjesen PA, Bhattacharya S, Patel S, Wetzel K, Woerle HJ. C-peptide levels in latent autoimmune diabetes in adults treated with linagliptin versus glimepiride: exploratory results from a 2-year double-blind, randomized, controlled study. Diabetes Care. 2014; 37:e11–e12. PMID:
24356601.

74. Buzzetti R, Pozzilli P, Frederich R, Iqbal N, Hirshberg B. Saxagliptin improves glycaemic control and C-peptide secretion in latent autoimmune diabetes in adults (LADA). Diabetes Metab Res Rev. 2016; 32:289–296. PMID:
26385269.

75. Dejgaard TF, Frandsen CS, Hansen TS, Almdal T, Urhammer S, Pedersen-Bjergaard U, Jensen T, Jensen AK, Holst JJ, Tarnow L, Knop FK, Madsbad S, Andersen HU. Efficacy and safety of liraglutide for overweight adult patients with type 1 diabetes and insufficient glycaemic control (Lira-1): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2016; 4:221–232. PMID:
26656289.

76. Pettus J, Hirsch I, Edelman S. GLP-1 agonists in type 1 diabetes. Clin Immunol. 2013; 149:317–323. PMID:
23643354.

77. Pozzilli P, Leslie RD, Peters AL, Buzzetti R, Shankar SS, Milicevic Z, Pavo I, Lebrec J, Martin S, Schloot NC. Dulaglutide treatment results in effective glycaemic control in latent autoimmune diabetes in adults (LADA): a post-hoc analysis of the AWARD-2, -4 and -5 trials. Diabetes Obes Metab. 2018; 20:1490–1498. PMID:
29377522.

78. Jones AG, McDonald TJ, Shields BM, Hill AV, Hyde CJ, Knight BA, Hattersley AT. PRIBA Study Group. Markers of β-cell failure predict poor glycemic response to GLP-1 receptor agonist therapy in type 2 diabetes. Diabetes Care. 2016; 39:250–257. PMID:
26242184.

79. Yang Z, Zhou Z, Li X, Huang G, Lin J. Rosiglitazone preserves islet beta-cell function of adult-onset latent autoimmune diabetes in 3 years follow-up study. Diabetes Res Clin Pract. 2009; 83:54–60. PMID:
19008007.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download