See the letter "Letter: Clinical Characteristics of People with Newly Diagnosed Type 2 Diabetes between 2015 and 2016: Difference by Age and Body Mass Index (Diabetes Metab J 2018;42:137-46)" on page 249.
We appreciate Dr. Khang's interest in and comments on our article entitled “Clinical characteristics of people with newly diagnosed type 2 diabetes between 2015 and 2016: difference by age and body mass index” which was published in Diabetes and Metabolism Journal [1].
Both β-cell dysfunction and impaired insulin sensitivity are critical for diabetes pathogenesis. In East Asian populations, diabetes is characterized primarily by β-cell dysfunction, and diabetes with obesity is less common compared to Caucasian populations [2]. However, in Korea, the incidence of diabetes with obesity has been increasing steadily [3]. In addition, the incidence of diabetes (defined as people newly treated with glucose-lowering drugs) among adults aged 20 to 39 years has also increased from 2006 to 2015, according to the National Health Insurance Service-National Sample Cohort database (Fig. 1, unpublished data). This early-onset type 2 diabetes mellitus is expected to be a major health problem because of the high risk of premature death, especially from cardiovascular diseases [4]. Thus, it is necessary to identify the characteristics of early-onset type 2 diabetes mellitus to provide appropriate preventive and therapeutic approaches.
As mentioned in the letter, in our survey we observed that people with early-onset type 2 diabetes mellitus, defined as diagnosis at younger than 40 years, had more severe β-cell dysfunction and more severely impaired insulin sensitivity than people with late-onset diabetes, defined as diagnosis after 65 years [1]. In addition, the frequency of poor glycemic control (defined as glycated hemoglobin ≥10%) was higher in people with early-onset diabetes than late-onset diabetes. Previous studies have also reported that people with early-onset diabetes had worse glycemic control compared with people with late-onset diabetes [567]. However, according to the 2013 to 2016 Korea National Health and Nutrition Examination Survey (KNHANES) data, the median homeostatic model assessment of β-cell function value was higher in people with early-onset diabetes than in those with late-onset diabetes (61.1% and 48.8%, respectively). In addition, in early-onset diabetes, levels of fasting glucose and glycosylated hemoglobin (HbA1c) were lower in the KNHANES dataset than in our survey (fasting glucose, 145.2 mg/dL vs. 172.0 mg/dL; HbA1c, 7.3% vs. 9.2%) (Fig. 2, unpublished data). There are notable differences between our survey and the KNHANES population-based survey in terms of severity of insulin secretion and degree of glycemic control.
In both our survey and the population-based study, people with early-onset diabetes had higher body mass index (BMI) than people with late-onset diabetes. In general, people with insulin resistance do not experience hyperglycemia, when β-cells increase insulin secretion as a compensatory response to the impaired insulin sensitivity [8]. Thus, in our survey, the insulin secretion defects associated with severe insulin resistance in early-onset diabetes may have been due to selection bias, because hospital-based recruitment may be limited to people with severe symptoms, especially in young adults who are unlikely to have diabetes. Although people with early-onset diabetes had more severely impaired insulin sensitivity and β-cell dysfunction than those diagnosed at a later age in the China National Diabetes and Metabolic Disorders Study, the former group had a lower BMI than those with early-onset diabetes among the Korean population [9]. Thus, the factors associated with diabetes in younger age groups vary among countries. However, the KNHANES dataset showed that the disposition index, which is used as an indicator of β-cell function, relative to insulin sensitivity, was lowest in people with early-onset diabetes (unpublished data). Taken together, these findings suggest that diabetes mellitus in younger people is associated with more marked decreases in insulin secretion than are seen in elderly diabetes cases.
Figures and Tables
Fig. 1
Incidence of diabetes among Korean adults aged 20 to 39 years newly treated with glucose-lowering drugs in the period 2006 to 2015.
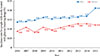
Fig. 2
Clinical characteristics of people with newly diagnosed diabetes in the Korea National Health and Nutrition Examination Survey (KNHANES) for the period 2013 to 2016, and in our survey, by age group [1]. Values are shown as means for normally distributed variables (age, body mass index [BMI], and waist circumference [WC]) and as medians for non-normally distributed variables (fasting glucose, fasting insulin, glycosylated hemoglobin [HbA1c], homeostatic model assessment of β-cell function [HOMA-β], homeostatic model assessment of insulin resistance [HOMA-IR]). a22 people aged <40 years, 128 people aged 40 to 64 years, and 92 people aged ≥65 years were assessed.

ACKNOWLEDGMENTS
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI13C0715).
References
1. Ha KH, Park CY, Jeong IK, Kim HJ, Kim SY, Kim WJ, Yoon JS, Kim IJ, Kim DJ, Kim S. Clinical characteristics of people with newly diagnosed type 2 diabetes between 2015 and 2016: difference by age and body mass index. Diabetes Metab J. 2018; 42:137–146.

2. Yabe D, Seino Y, Fukushima M, Seino S. β Cell dysfunction versus insulin resistance in the pathogenesis of type 2 diabetes in East Asians. Curr Diab Rep. 2015; 15:602.

3. Ha KH, Kim DJ. Trends in the diabetes epidemic in Korea. Endocrinol Metab (Seoul). 2015; 30:142–146.

4. Huo L, Magliano DJ, Ranciere F, Harding JL, Nanayakkara N, Shaw JE, Carstensen B. Impact of age at diagnosis and duration of type 2 diabetes on mortality in Australia 1997–2011. Diabetologia. 2018; 61:1055–1063.

5. Benhalima K, Wilmot E, Khunti K, Gray LJ, Lawrence I, Davies M. Type 2 diabetes in younger adults: clinical characteristics, diabetes-related complications and management of risk factors. Prim Care Diabetes. 2011; 5:57–62.

6. Song SH, Hardisty CA. Early onset type 2 diabetes mellitus: a harbinger for complications in later years: clinical observation from a secondary care cohort. QJM. 2009; 102:799–806.
7. Chuang LM, Soegondo S, Soewondo P, Kim YS, Mohamed M, Dalisay E, Go R, Lee W, Tong-Yuan T, Tandhanand S, Nitiyanant W, The-Trach M, Cockram C, Jing-Ping Y. Comparisons of the outcomes on control, type of management and complications status in early onset and late onset type 2 diabetes in Asia. Diabetes Res Clin Pract. 2006; 71:146–155.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download